1. Context
Hospital readmission refers to the act of being admitted to the same healthcare facility with the same initial diagnosis within an unspecified timeframe. The importance of understanding post-discharge hospital readmissions has been steadily increasing due to the upward trend in readmission rates observed in hospitals over the past few decades (1). It has been reported that approximately one-fourth of all hospital admissions in the United States consist of readmissions (2). Additionally, one out of every five Medicare beneficiaries is readmitted to the hospital within 30 days of discharge (3).
Unplanned readmissions are commonly regarded as indicators of inadequate healthcare service quality (4) and can signify shortcomings in hospital management or discharge procedures, often being avoidable (5). There is no consensus regarding the proportion of readmissions that can be avoided, with significant variation across studies, ranging from 5% to 79% (6). Another study estimated that approximately 60% of hospital readmissions are potentially preventable (7).
Unplanned readmissions have implications for both individuals and society as a whole. Socially, these consequences exert pressure on healthcare systems and lead to increased hospital expenses (2). Reported estimates indicate that annual healthcare system costs associated with readmissions range from $12 billion to $17.4 billion in the United States and £1.6 billion in Britain (3). These figures underscore the importance of reducing unnecessary expenses related to readmissions (8). Additionally, another study conducted in the United States revealed that readmissions within 30 days of discharge accounted for costs totaling $17.4 billion, with a readmission rate of 19.6% (9).
Penalties established through cost-effective care legislation and readmission reduction programs provide incentives for hospitals to adopt interventions aimed at reducing the likelihood of readmission, particularly within 30 days (10).
Readmission is influenced by various patient-related factors, such as age, gender, ethnicity, the presence of comorbidities, chronic conditions, and functional disabilities. Research indicates that broader organizational factors and care processes also have a significant impact (11).
This scoping review examined the relationship between targeted interventions and hospital readmissions for the following common diagnoses: Cardiovascular disease, surgery, premature infants, psychiatry, respiratory disease, type 2 diabetes, hip and knee replacement, malnutrition, high blood pressure, and chronic obstructive pulmonary disease. In relation to interventions to reduce readmissions, a number of systematic studies have been conducted worldwide.
This study complements previous reviews of the readmission intervention literature, which focused narrowly on appropriate policy-making, interdepartmental communications, pharmaceutical counseling, social support, and disease management programs. In this study, we have determined which types of interventions are more promising for reducing hospital readmissions among patients with common diagnoses.
2. Methods
A scoping review was conducted following the PRISMA guidelines. In the initial stage, the research question was formulated based on the PCC elements. The objective of this study was to identify strategies and interventions used to decrease hospital readmissions (Concept) in the entire population of individuals in all countries of the world (Population) within hospital settings (Context). The search was conducted between February 20 and March 20, 2023.
Research keywords included [(Re-Hospitalization) OR (Readmission, Patient) OR (Hospital Readmission) OR (readmission rates) OR (Rehospitalization) OR (Unplanned Readmissions) OR (Unplanned Hospital Readmissions)) AND ((Early Intervention) OR (preventable) OR (Educational Early Intervention) OR (Reduction Program) OR (Reduction Strategy) OR (Interventions)], which were searched in PubMed, Scopus, Web of Science, and Google Scholar.
The investigated articles have different individual effects, and we have not yet established a relationship between them. The important thing is to determine the information and connections between the articles we reviewed and to maintain a macro view. Depending on the type of study and subject matter, the type of data analysis will vary. Content analysis is one of the qualitative data analysis methods. Our analysis should be scientific, principled, and free from any bias. Text analysis software such as MAXQDA can be used to analyze qualitative data. In this study, the content analysis method and MAXQDA version 10 software were used.
It is better to analyze the data as a team. After recovering, screening, and extracting data, three consecutive meetings were held with health management professors, hospital managers, and experts for thematic analysis and classification of interventions to reduce the rate of re-hospitalization. After the third meeting, the final classification was obtained and confirmed based on the consensus of the participants.
2.1. Inclusion and Exclusion Criteria
The selection criteria included articles related to the purpose of the research, published in English and Farsi in domestic and international scientific-research journals. Articles were excluded if the full text was not available, if the topic was deemed irrelevant after reading the article, or if the article was repetitive. Protocols and review studies were not included in the present research.
2.2. Quality Assessment of Articles
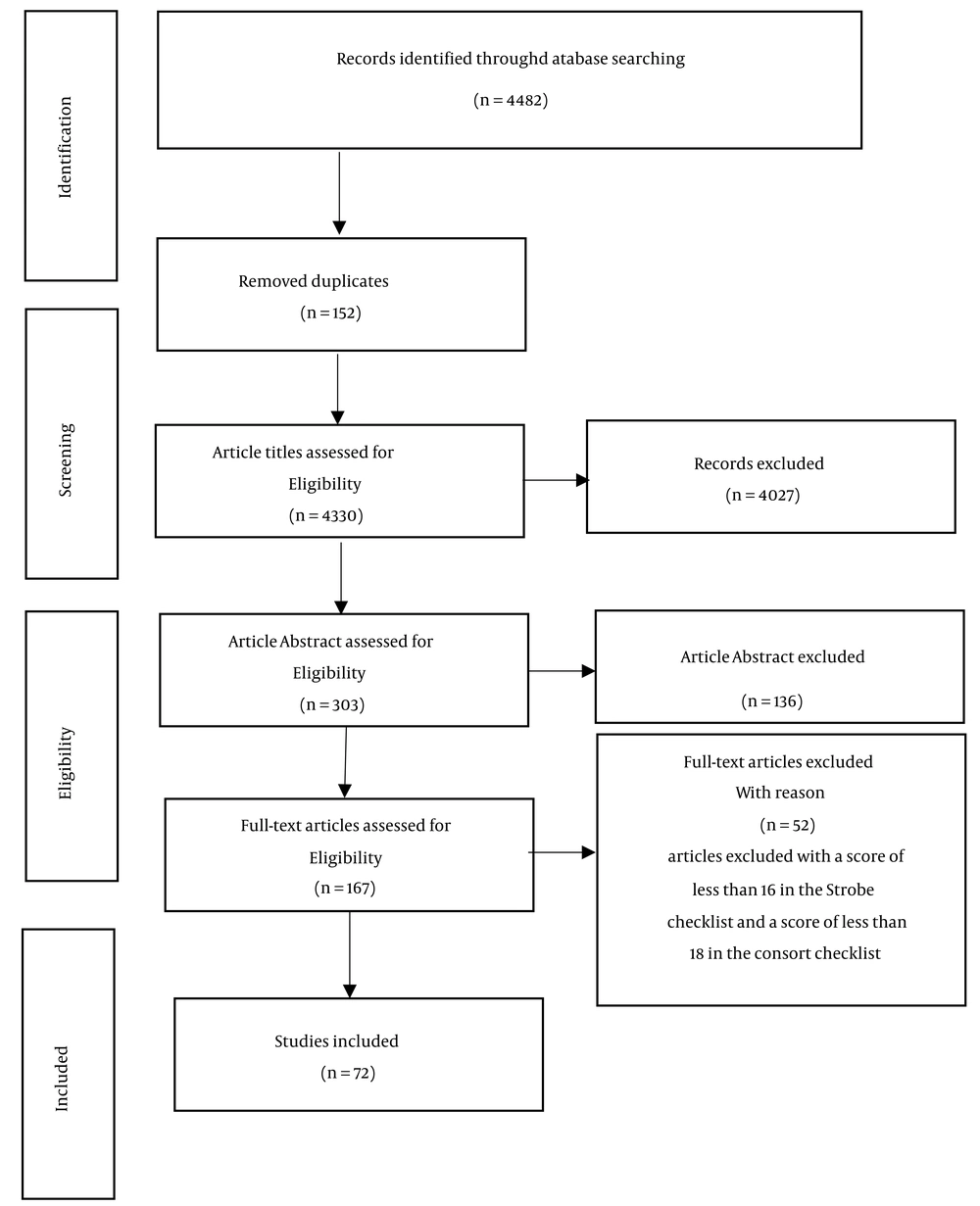
Unduplicated articles were evaluated by two researchers based on the title, abstract, and text of the article using the STROBE checklist (https://www.strobe-statement.org/) and CONSORT checklist (https://www.consort-statement.org/). In case of disagreement between the two reviewers on the inclusion of articles, a third reviewer or an independent reviewer was consulted to provide an unbiased judgment. According to the agreement of the research team members, the selected articles had to cover at least 16 out of 22 points on the STROBE checklist and at least 18 out of 25 points on the CONSORT checklist. Articles with a lower score were excluded from the review.
3. Results
A total of 4482 articles were retrieved, and after screening, 72 studies met the eligibility criteria for inclusion in the study. The article retrieval and screening process is shown in Figure 1. Descriptive characteristics of the included articles are provided in Table 1. The articles selected for this study spanned from 1990 to 2023, with many (50%) published between 2015 and 2019. Due to increased awareness of the importance of this issue and the rise in the number of studies in recent years, more research has been conducted under the title of readmission strategies in developed countries.
| Participant or Study Characteristic | Number of Studies b | References |
|---|---|---|
| Year of publication | ||
| 1990 - 1999 | 1 (1.5) | (12) |
| 2000 - 2004 | 2 (2.5) | (13, 14) |
| 2005 - 2009 | 3 (6) | (15-17) |
| 2010 - 2014 | 15 (20) | (18-32) |
| 2015 - 2019 | 36 (50) | (6, 9, 10,33-65) |
| 2020 - 2023 | 15 (20) | (5, 66-79) |
| Country | ||
| Developed nations | 39 (55) | (6, 14, 22-24, 27-32, 39-42, 44-47, 50, 51, 53-59, 61-64, 71-74, 77, 78) |
| Developing nations | 33 (45) | (5, 10, 12, 13, 15-21, 25, 26, 33-38, 43, 48, 49, 52, 60, 65-70, 75, 76, 79) |
| Study design | ||
| Historical cohort study | 9 (12.6) | (6, 21, 24, 30, 50, 65, 72, 75, 77) |
| Cross-sectional study | 19 (26.7) | (10, 28, 31, 32, 40-42, 45, 52-54, 57-62, 73, 74) |
| Clinical trial | 36 (50) | (5, 9, 13, 15-20, 22, 23, 26, 27, 33-39, 43, 44, 46-49, 51, (63, 66-71, 76, 79) |
| Case-control study | 4 (5.6) | (12, 29, 55, 78) |
| Before-after study | 2 (2.8) | (14, 25) |
| Qualitative | 1 (2.30 | (64) |
| Hospital readmission period | ||
| < 30 days | 6 (9) | (13, 21, 34, 40, 63, 67) |
| 30 days | 29 (44) | (5, 10, 12, 19, 23, 24, 27, 30, 35, 36, 41-43, 45-48, 50-52, 54, 59, 61, 65, 66, 71, 72, 76, 79) |
| 60 days | 4 (8) | (9, 10, 16, 35) |
| 90 days | 12 (18) | (5, 17, 18, 20, 33, 35, 38, 44, 51, 68, 70, 73) |
| Six months to one year | 14 (21) | (6, 14, 15, 22, 25, 26, 28, 37, 39, 49, 53, 55, 62, 69) |
| Sample size | ||
| < 100 | 22 (37) | (5, 12, 13, 15-18, 26, 28, 34-38, 44, 49, 66-70, 74) |
| 100 - 499 | 23 (39) | (9, 14, 19-21, 23-25, 27, 33, 39, 40, 43, 46-48, 51, 55, 63, 65, 71, 76, 77) |
| 500 - 999 | 4 (8) | (6, 30, 32, 79) |
| ≥ 1,000 | 10 (16) | (22, 41, 42, 45, 50, 52-54, 72, 75) |
| Type of Disease | ||
| Cardiovascular disease | 19 (40) | (9, 12, 13, 15, 16, 18, 20, 22, 32, 33, 35, 38, 39, 43, 46, 57, 62, 67-70) |
| Surgery | 3 (6) | (40, 58, 60) |
| Premature infants | 5 (10.5) | (19, 34, 36, 48, 66) |
| Psychiatry | 5 (10.5) | (14, 17, 26, 27, 37) |
| Respiratory disease | 3 (6) | (24, 25, 44) |
| Type 2 diabetes | 1 (3.5) | (71) |
| Hip and knee replacement | 2 (3.5) | (29, 45) |
| Malnutrition | 3 (6) | (28, 49-54) |
| Blood pressure | 1 (3.5) | (75) |
| Chronic obstructive pulmonary disease | 5 (10.5) | (24, 25, 44, 51, 52) |
a Limitations: All the information displayed in the above table is based on the available articles, and more than 95% of the articles in each category have been repeated.
b Values are expressed as No. (%).
Out of these studies, rehospitalization within 30 days after discharge was monitored in 29 studies (44%). The sample sizes of the studies varied from 40 to over 1000 participants, with almost 39% of the studies including a study population ranging from 100 to 499 individuals. Cardiac diseases were the focus of most studies (43%). Approximately 50% of the studies utilized clinical trial methodology, comparing intervention groups with control or placebo groups to investigate the effectiveness of interventions.
Other findings reveal that a total of fourteen key intervention groups have been suggested as effective in reducing hospital readmissions. These interventions encompass disease management programs, appropriate policy-making, utilization of advanced discharge planning models, education, post-discharge patient follow-up, implementation of health information technology, interdepartmental communication, departmental structure, adequate staffing, professional skill development, social support, pharmaceutical counseling, rehabilitation and recovery, and nutritional counseling (Table 2). Each group includes several categories, the findings of which are shown in Table 2.
| Row | Interventions | References |
|---|---|---|
| 1 | Disease management programs | |
| Implementation of continuous care model | (15) | |
| Daily patient assessments during hospitalization | (56, 75) | |
| Improvement of the quality of nursing services during hospitalization | (74) | |
| 2 | Appropriate policy-making | |
| Changing insurance reimbursement policies | (58, 59, 73) | |
| Awareness among service providers about the economic consequences and quality of life | (29) | |
| Establishing a continuous review committee for readmission indicators | (64) | |
| Creating a mechanism for case-specific discharge reviews (disease-specific) | (64) | |
| 3 | Utilization of advanced discharge planning models | |
| Discharging plan | (66) | |
| Implementing a readiness program for discharge, including pre-discharge check-ups | (62, 74) | |
| 4 | Education | |
| Patient-centered education | (35, 39) | |
| OR companion-centered education (based on needs assessment) | (35) | |
| Empowering the patient | (5, 9, 12, 13, 17, 18, 20, 22, 33, 35, 44, 69) | |
| Empowering the companion | (9, 17, 19, 34-37, 48, 66) | |
| Feedback-oriented education | (68, 70) | |
| 5 | Post-discharge patient follow-up | |
| Follow-up by a family physician | (29, 57, 64) | |
| Telephone follow-up | (6, 9, 18, 20-23, 31, 37, 38, 40, 44, 63, 66, 67, 69, 71, 76) | |
| Follow-up at the clinic | (12, 25) | |
| Post-discharge physician visit at the office | (17, 24, 42) | |
| 6 | Implementation of health information technology | |
| Development of computer technology for patient coordination and monitoring | (32) | |
| Development of remote care technologies | (79) | |
| Utilization of decision support systems | (10) | |
| Development of electronic health records (EHR) | (64) | |
| 7 | Interdepartmental communications | |
| Establishment of post-discharge emergency services at the hospital | (78) | |
| Enhancement of communication between hospital departments and other service providers | (30, 60, 61, 65) | |
| 8 | Departmental structure | |
| Promoting a culture of teamwork among healthcare professionals | (77) | |
| 9 | Adequate staffing | |
| Increasing the number of nursing staff | (45) | |
| 10 | Development of specialized skills | |
| Training and employing specialized personnel for transitions (transition nurses) | (71, 76) | |
| 11 | Social support | |
| Family support | (14) | |
| Social worker assistance | (23, 41) | |
| Peer support (mentoring) | (14, 26, 27) | |
| 12 | Pharmaceutical counseling | |
| Employment of clinical pharmacists in the hospital | (46, 71) | |
| Provision of necessary medications at the time of discharge | (72) | |
| Utilization of social pharmacists | (47) | |
| 13 | Rehabilitation and recovery | |
| Rehabilitation and recovery | (16, 25, 56) | |
| Exercise training | (12, 13, 43, 44, 63) | |
| 14 | Nutritional counseling | |
| Nutritional support during discharge | (28, 49-51, 53, 54) | |
| Nutritional support after discharge | (54) | |
| Individual nutrition counseling over the phone | (49, 52) | |
| In-person individual nutrition counseling | (52) | |
| Dietary supplements and improving food status | (50, 51, 55) |
4. Discussion
Reducing hospital readmissions is a top priority in any healthcare system, and several interventions have been proposed to address this issue. Post-discharge patient follow-up was identified as the most crucial intervention, with telephone follow-up being the most frequent category. Among the eighteen intervention studies that included telephone follow-up, twelve demonstrated significant effectiveness in reducing readmission rates (6, 9, 19), (21-23), (32, 38, 39), (41, 64, 67). Most of these studies integrated telephone follow-up with other interventions, while only five studies focused exclusively on telephone follow-up (6, 22, 39, 41, 68).
Educational interventions were identified as the second most common approach. Our findings indicate that educational interventions are often integrated with telephone follow-up, pharmaceutical counseling, and discharge planning (9, 16, 19), (23, 35, 38), (45, 48, 63), (70, 77). Our investigation incorporates evidence from various authors who have assessed the impact of educational interventions on aspects such as quality of life, disease awareness, self-care, reduction in readmission costs, and cost-effectiveness of the intervention (5, 9, 13), (14, 18, 19), (21, 23, 34, 70).
Nutritional interventions included individual nutrition counseling during discharge. Supplementation with oral nutritional supplements (ONS), whether administered during hospitalization or in a community setting following discharge, contributes to a reduction in readmissions (51, 52, 56).
A community-based care transition program illustrates a well-established and formal network of collaborations between acute care hospitals and community-based organizations. These collaborations involve social service organizations that offer timely post-discharge care to patients and monitor their progress. Among the five available studies, four have highlighted the impact of these collaborations on reducing hospital readmissions (31, 61, 62, 66). In another study, EMS personnel played a key role in connecting patients to community-based support mechanisms for both physical and mental health. Patients who received the intervention experienced a relative decrease of 44% in physician visits and a relative reduction of 28.4% in 30-day readmissions.
Providing medication upon patient discharge is crucial for preventing errors and ensuring continuity of care. Delivering post-discharge medications at the bedside and providing medications to patients before discharge can help overcome initial barriers to medication access and address any insurance or medication discrepancies that may arise (73).
4.1. Conclusions
Post-discharge follow-up and patient education were identified as two effective interventions for reducing readmissions. However, their effectiveness can be enhanced when combined with other interventions. Furthermore, our study provides strong evidence supporting the effectiveness of community-based interventions in reducing readmissions, including appropriate policy-making, interdepartmental communications, pharmaceutical counseling, social support, and disease management programs. The results of this study offer valuable insights for health policymakers and hospital administrators, particularly on a global scale.
4.2. Limitations
It is possible that our search method did not capture all relevant studies. To mitigate this, all steps were performed by two independent researchers.