1. Background
The emergence and spread of the novel human coronavirus, known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), through the air has become a subject of debate among scientists (1-3). Various microorganisms, including algae, protozoa, yeasts, molds, and viruses, can be transmitted through the air, primarily via dust and water droplets. Despite the significant role of hospital-acquired respiratory viral infections in the morbidity and mortality of hospitalized patients, studies on such infections remain limited. A study on acute respiratory infections in hospitalized patients revealed that many cases were of viral origin (1).
Infection control precautions in hospitals include not only hygiene and sanitation but also transmission-based strategies tailored to the mode of infection spread (4, 5). Droplet nuclei, primarily smaller than 5 µm (6), can remain suspended in the air for extended periods and are likely involved in airborne transmission in both clinical and non-clinical indoor environments (5, 7). Proper ventilation management through mechanical systems, especially in high-risk areas such as operating rooms, transplant facilities, and intensive care units (ICUs), has been suggested as an effective strategy to reduce infection transmission (5, 8). Enhanced mechanical ventilation involves not just increasing airflow rates but also controlling pressure differentials and airflow patterns (5, 9). A review examining the relationship between ventilation, airflow control, and the spread of infectious diseases highlighted the importance of negative pressure isolation rooms for patients with various infectious conditions (10).
With the increasing number of COVID-19 cases and related deaths, the demand for medical resources—including medications, experienced healthcare personnel, medical equipment, and critical infrastructure like airborne infection isolation rooms (AIIRs)—has risen dramatically. For severe cases requiring ICU admission and aerosol-generating procedures (e.g., mechanical ventilation or tracheal suction), isolating patients in designated rooms is essential to prevent the spread of infection to healthcare workers and other patients (11). Although the primary mode of SARS-CoV-2 transmission remains unclear, respiratory droplets and potentially small aerosols are considered the main vectors. The Centers for Disease Control and Prevention (CDC) recommends that patients with confirmed or suspected SARS-CoV-2 infection requiring aerosol-generating procedures be placed in single-person, negative-pressure rooms with closed doors (12).
A recent assessment in the United States revealed that less than 6% of acute hospital beds are in isolation rooms (13). A study conducted in an ICU equipped with a heating, ventilation, and air conditioning (HVAC) system using negative pressure for SARS-CoV-2 patients demonstrated the HVAC system’s role in reducing viral spread. However, the study also showed that air circulation within ICU rooms—from supply diffusers to exhaust grills — can expose healthcare providers to airborne SARS-CoV-2, as some viral particles may bypass the ventilation system and enter the respiratory tract (14). In another study evaluating 16 isolation rooms, air change rates per hour met standards in only 5.3% of cases, temperature in 10.2%, and humidity in 94.7%. No significant correlation was found between biological growth and temperature, humidity, or ventilation rates (15).
According to established standards, key parameters for controlling airborne infections include managing pressure differentials to maintain proper airflow direction and ensuring adequate air changes per hour for dilution. The recommended pressure differential in respiratory isolation rooms is 2.5 pascals (16). These rooms must maintain negative pressure and be equipped with HEPA filters capable of achieving 10 - 15 air changes per hour (17, 18). To ensure consistent negative pressure, doors should close automatically, and all structural components—walls, ceilings, windows, and floors—must be sealed (19).
2. Objectives
Given the importance of AIIRs in controlling the spread of infectious diseases in healthcare settings, this study aimed to evaluate the compliance of AIIRs with standard conditions during the COVID-19 outbreak.
3. Methods
In a cross-sectional descriptive study conducted in Mashhad, the compliance of hospital isolation rooms with standard conditions was evaluated using a checklist (Table 1) designed based on the 2020 isolation room standards. The checklist was developed according to the ventilation system guidelines established by the Iran Environment and Work Health Center (17). In this study, a total of 13 hospitals and 31 isolation rooms were assessed.
| Items to be Controlled in Isolated Room | According to the Standard | Non-compliance with the Standard |
|---|---|---|
| Is the room sealed? | ||
| Is it possible to recirculate the air in the room? | ||
| Is the air inlet near the ceiling at the top of the patient's head and the air outlet at the bottom of the patient's feet at 15-30 cm from the floor? | ||
| Is the width of the doors at least 1.2 meters? | ||
| Is the warning system for reduced pressure, humidity, heat, and opened door installed and active? | ||
| Does the isolation room have three parts: anteroom, patient room, and bathroom? | ||
| Is the existing system for ventilation and creating negative pressure independent and separate from the hospital's ventilation system? | ||
| Does the HEPA filter system have at least two primary pre-filters? | ||
| Has the necessary area for the anteroom space been considered (at least 6 to 9 square meters)? | ||
| Does the anteroom have the same pressure system as the isolated room? | ||
| Is there a proper distance between the beds in the isolation room? (at least 1 meter, preferably 2.5 meters with a partition) | ||
| Is the humidity of the isolated room optimal (30 - 60%)? | ||
| Is the isolation room temperature optimal (20 - 24 degrees Celsius)? |
A digital manometer (MP 120) was used to measure the pressure. Additionally, the concentration of carbon dioxide, a critical parameter for evaluating ventilation efficiency, was measured using the AirCon2rol3000 device. Airflow velocity at each air inlet and outlet was calculated based on air-conditioning engineers (ASHRAE) standards, as illustrated in Figure 1, using a TES 1340 thermal anemometer (Taiwan) in accordance with ACGIH standards. To enhance data reliability, sampling was conducted three times at each location. The dimensions and shape of each air conditioning inlet were taken into account during the measurements.
Airflow velocity was measured at multiple points on both the air inlet and outlet grilles in all isolation rooms. Subsequently, the air exchange rate per hour (ACH) was calculated using specific formulas (Equations 1 and 2):
V = Air speed (fpm); A= Area of inlet (ft2).
That Q (ft3/min) = air flow and V = volume of room (ft3)
4. Results
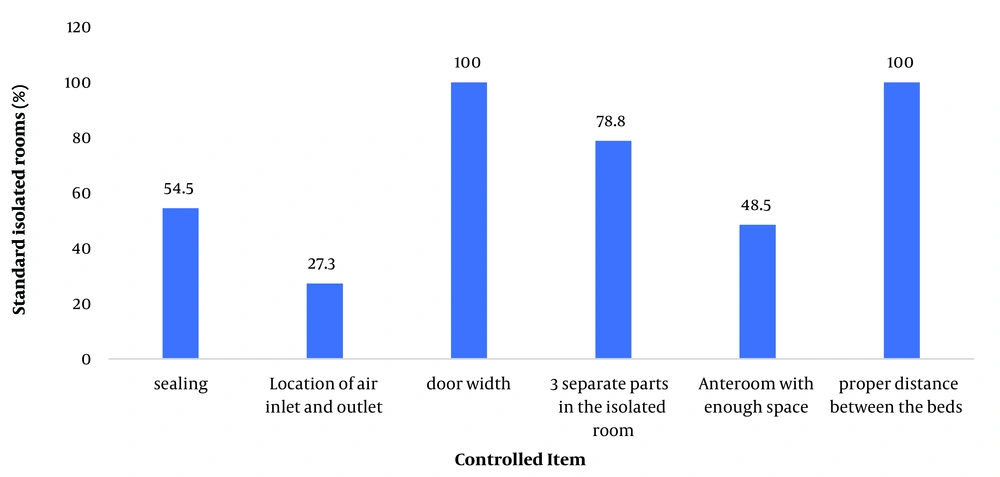
A total of 33 isolation rooms across 13 different hospitals were investigated. The results are presented as figures illustrating the compliance of the isolation rooms with established hospital standards. The data related to the physical conditions of the rooms, including spatial measurements and distances, are shown in Figure 2.
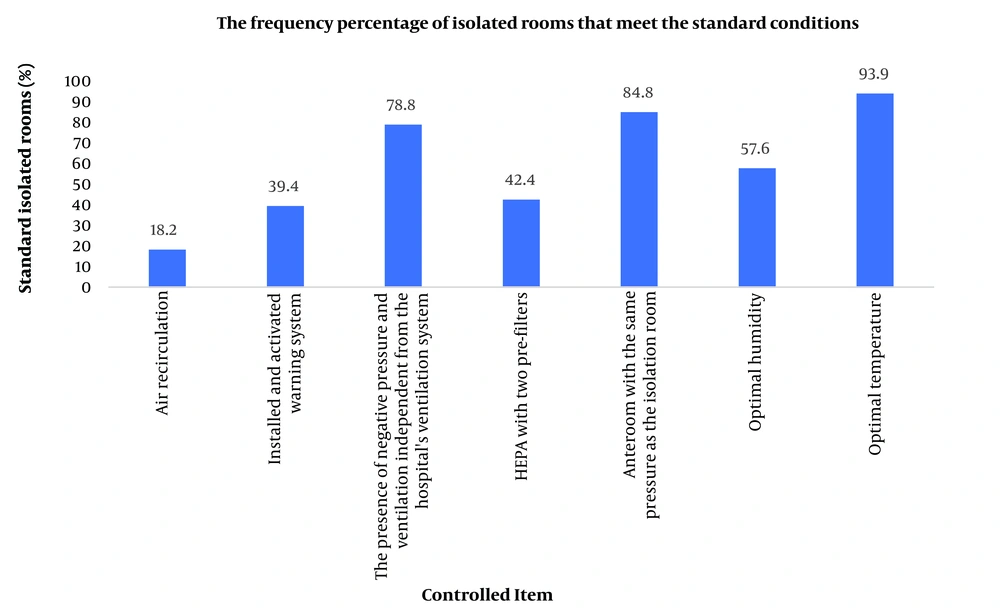
Figure 3 presents the findings related to ventilation, filtration, pressure, temperature, and humidity. Additional results, not depicted in the figures, indicated that the air change rate per hour met the standard in 27.27% of cases. Regarding the pressure difference between the respiratory isolation rooms and the adjacent wards, 63.64% of the rooms maintained the standard pressure differential.
The average measured carbon dioxide (CO₂) concentration in the isolation rooms was 562 ppm. Additionally, the average airflow rate in the isolation rooms was estimated to be 299.3 cubic meters per minute.
5. Discussion
Indoor air's physical, chemical, and biological characteristics affect people's health and comfort. The air quality inside buildings is not easily controllable, and poor air quality in medical centers may lead to adverse effects on the health of medical personnel. Hospital air contains a wide range of pathogenic microorganisms (20). To minimize and control SARS-CoV-2 transmission between residents and staff, a study was conducted to create an isolation space at a skilled nursing facility in Lancaster, Pennsylvania. The isolation space was built by modifying an existing HVAC system. The isolation space was successfully implemented, and SARS-CoV-2 was not transmitted between residents isolated in the space, staff, or other residents (21).
According to the results of the current study, more than half of the isolation rooms (57.6%) were not equipped with HEPA filters as required under standard conditions, even though using high-efficiency filters is a critical method for reducing the potential transmission of airborne pathogens. The room pressure difference is also essential in controlling airflow between areas inside the building. For example, the isolation room must always have negative pressure compared to adjacent areas to prevent the escape of pathogenic agents through airflow (22). In this study, 78.8% of the rooms had a negative pressure ventilation system independent of the hospital’s central ventilation system.
This study showed that although the distance between beds was appropriate in all cases, the location of the air inlets and outlets relative to the patient’s bed was non-standard in 72.7% of the rooms. The position of the patient’s bed, as a source of bioaerosol emission, relative to the ventilation system significantly affects the exposure of medical personnel to airborne bioaerosols (23).
Studies highlight the importance of air inlet and outlet placement concerning ventilation. For example, in a study by Melikov et al. (24), the use of new ventilation systems at patients’ bedsides and the installation of suction systems near the bed and the patient’s mouth reduced healthcare providers' exposure to exhaled air both at the bedside and in other parts of the room.
Carbon dioxide measurement is a valuable tool for determining the amount of exhaled air based on the number of people in a given space (25). The American Society of Heating, Refrigerating, and ASHRAE recommends that indoor carbon dioxide levels range between 1000 - 1200 ppm, although different standards may specify varying values (26). In the present study, the average carbon dioxide concentration was 562 ppm, which may indicate an adequate ventilation rate since CO₂ levels tend to increase as ventilation decreases in indoor environments (27).
According to the standard, the air exchange rate per hour (ACH) for a respiratory isolation room (negative pressure) must be greater than or equal to 12 air changes per hour (28). Unfortunately, the results of the present study showed that the ACH met this standard in only 27.27% of cases.
In a study by Lee and Song in South Korea, temporary AIIRs were assembled using mobile negative-air machines in ICUs to care for critically ill COVID-19 patients. This study demonstrated that renovating ICUs with temporary AIIRs was a critical measure during the COVID-19 outbreak, effectively protecting severely ill patients (29). In a study conducted in Taiwan by Wang et al., during the COVID-19 outbreak, isolation rooms located in the emergency department were investigated through field measurements to evaluate ventilation performance. According to the study’s results, rearranging the location of exhaust air grills improved ventilation performance (30).
5.1. Conclusions
The results showed that a high percentage of isolation rooms did not meet standard conditions, posing a significant risk to the health of both patients and hospital staff due to the potential spread of airborne infectious diseases.
5.2. Limitation
At the time of the measurements, the COVID-19 situation was classified as yellow or more acute. Consequently, the use of personal protective equipment (PPE) and the presence of patients in the isolation rooms made data collection slow and challenging.
5.3. Suggestion
Future studies should focus on evaluating the performance of ventilation and filtration systems, with particular attention to the efficiency and functionality of HEPA filters to ensure optimal infection control.