1. Background
General practitioners (GPs) are considered the gatekeepers of the health care system since they are the providers of a wide range of services: Promotive, protective, preventive, curative, rehabilitative, and palliative care, both to individuals and families within their communities (1). In this way, the GP contributes to continuity and coordination of care, enabling a good patient-provider relationship in the long term, making certain that patients receive personalized care and support over time. This comprehensive approach supports better health outcomes and enhances the overall effectiveness of the healthcare system by reducing the unnecessary use of emergency and specialist services (2, 3). Additionally, general physicians have been shown to be effective in managing chronic diseases such as diabetes, hypertension, and heart disease, leading to improved patient outcomes and reduced hospitalizations (4).
In the recent decade, there has been a growing interest in primary health care, with the role of GPs at the center. The world faces several health challenges, including aging populations, chronic diseases, inequitable access to health services, and outbreaks such as COVID-19 (5). To address these challenges, primary care and GPs have been promoted as essential tools for advancing public health and reducing health disparities. There is strong evidence that health systems that prioritize primary care and the role of GPs can reduce healthcare costs while improving health outcomes (6).
Iran's health system has made a remarkable improvement during the last few decades, especially in terms of access to primary health care services (7). Despite these efforts, however, there are still gaps in the delivery of primary care services, especially in rural and underserved areas (8). These challenges highlight the need for a better understanding of the role and importance of general physicians in the Iranian context.
In this qualitative study, we aim to explore the roles and responsibilities of general physicians in the Iranian health system from the perspectives of both general physicians and policymakers. Through in-depth interviews with general physicians and policymakers, we seek to gain valuable insights into the challenges faced by general physicians in delivering high-quality primary care services and identify potential solutions to address these issues.
2. Objectives
This study seeks to enrich the existing literature on the Iranian healthcare system by examining the experiences and viewpoints of general physicians and other key stakeholders. Our goal is to inform policies that will bolster primary care services and enhance the quality of primary care delivered by general physicians and improve the overall health system in Iran.
3. Methods
3.1. Study Design
In this study, we employed a qualitative research design to explore the role and position of general physicians within Iran's healthcare system. To collect data, we conducted semi-structured interviews with various stakeholders, including health policymakers and general physicians practicing in Iran.
3.2. Study Setting
This study was conducted in Iran, with participants recruited from various provinces and cities across the country. Our goal was to gather a diverse group of individuals whose varied perspectives and experiences would allow us to gain a comprehensive understanding of the research topic. To achieve this, we collected data through interviews conducted in multiple settings, including offices, hospitals, clinics, and primary care centers located in several provinces of Iran. Prior to each interview, all participants were asked to provide informed consent to take part in the study.
3.3. Sampling and Recruitment of Participants
For this study, we employed purposive sampling to select participants whose perspectives could provide valuable insights into the role and position of general physicians in Iran's healthcare system. To ensure a comprehensive understanding, we identified key health policymakers and practicing general physicians from both the public and private sectors as the primary inclusion criteria. Specifically, we referred to national documents such as the family physician program in Iran, the General Medical Curriculum Revision, and the Association of general practitioners to identify and recruit participants who are influential in shaping healthcare policies and educational frameworks.
3.4. Identification and Recruitment Process
3.4.1. Key Health Policymakers
We focused on policymakers who have a major impact on the execution and monitoring of healthcare policies in Iran. These individuals were selected due to their participation in national health initiatives and their positions within the Ministry of Health and Medical Education. Special attention was given to those involved with the family physician program, which is essential for delivering primary healthcare in Iran.
3.4.2. General Medical Curriculum Revision
Policymakers and educational leaders involved in the recent revision of the general medical curriculum were also included. These participants were identified through their contributions to national curriculum development committees and their roles in academic institutions.
3.4.3. Association of General Practitioners
Members of the Association of general practitioners, which represents the interests of general physicians in Iran, were also included. This group provided valuable insights into the professional challenges and opportunities faced by GPs in both urban and rural settings.
3.5. Data Collection
The primary method of data collection in this study was semi-structured interviews, conducted either in person or remotely, depending on the participants' locations. Permission to audio-record the interviews was obtained from all participants. The interviewers involved in the study were highly trained and experienced researchers with a Ph.D. in healthcare management. To ensure consistency across interviews while allowing flexibility to explore emerging topics, a semi-structured interview guide was utilized (Table 1).
| Guide | Content |
|---|---|
| 1 | What are the primary roles and responsibilities of general practitioners in Iran's healthcare system and how have they evolved over time? |
| 2 | How do general practitioners in Iran perceive their roles and responsibilities and what challenges do they face in fulfilling them? |
| 3 | How does the Iranian government support and regulate the work of general practitioners and how has this changed over the years? |
| 4 | How do patients in Iran view the role and value of general practitioners and how does this impact their healthcare-seeking behaviors? |
| 5 | In what ways can general practitioners in Iran be better supported to provide high-quality primary care services and what policy changes would be necessary to enable this? |
At the beginning of each interview, the interviewer established rapport with the participant and explained the purpose of the study. During the interview process, open-ended questions were asked to gain insight into participants' experiences and perspectives on the role and position of general physicians within Iran's health system. If necessary, repeat interviews were conducted. All interviews were audio-recorded and transcribed, and field notes were taken during each session. The duration of each interview was also documented.
Participants were informed that their participation was voluntary and that they could withdraw at any time. To protect confidentiality, each participant was assigned a unique identification number. Overall, the use of semi-structured interviews provided rich and diverse data, which were analyzed to gain valuable insights into the role and position of general physicians within Iran's health system.
To ensure data validity, four criteria were used: Credibility, transferability, confirmability, and dependability, according to the rigor criteria of Lincoln and Guba (9). For credibility, the initial codes were sent to some of the participants to ensure the consistency of the results. For transferability, the authors described the data-gathering method and the analysis of the data. To ensure confirmability, all codes, subcategories, and categories were reviewed by several experts in the related field. For dependability, the steps of the research were clearly described for other researchers.
3.6. Data Analysis Approach
The data collected from the interviews were transcribed verbatim and analyzed using a combination of inductive and deductive content analysis. Initially, deductive coding was applied in accordance with the research questions to establish a framework for analysis. This was followed by an inductive approach to identify emergent concepts and themes within the data. This combined approach allowed us to identify common patterns and themes across the data while also capturing individual perspectives and experiences.
We utilized MAXQDA 2022 software to manage and analyze the data, implementing a structured five-step data analysis process (10). The analysis consisted of several stages, including familiarization with the data, coding, theme development, and final interpretation. In the initial stage, two independent researchers engaged in deductive coding, categorizing the transcripts based on the established research questions. This was followed by an iterative process of reading and re-reading the transcripts to identify emergent themes and sub-themes through inductive coding.
Throughout the data analysis process, both the methodological orientation and theoretical frameworks were taken into consideration, ensuring a comprehensive understanding of the data.
4. Results
In this research, 32 participants (21 men and 11 women) were interviewed. These participants included 12 health policymakers from different levels and 20 general physicians, with an average age of 42.4 years (Table 2). The data collection and analysis for the study took over 8 months (April 2021 to December 2021).
| Demographic Variables and Categories | Frequency |
|---|---|
| Gender | |
| Male | 21 |
| Female | 11 |
| Age (y) | |
| 30 - 40 | 6 |
| 40 - 50 | 17 |
| 50 - 60 | 9 |
| Experience (y) | |
| 1 - 5 | 5 |
| 6 - 10 | 7 |
| 11 - 15 | 10 |
| 16 - 20 | 6 |
| > 21 | 4 |
| Sector | |
| Public | 21 |
| Private | 11 |
| Role | |
| General physician | 20 |
| Health policymaker | 12 |
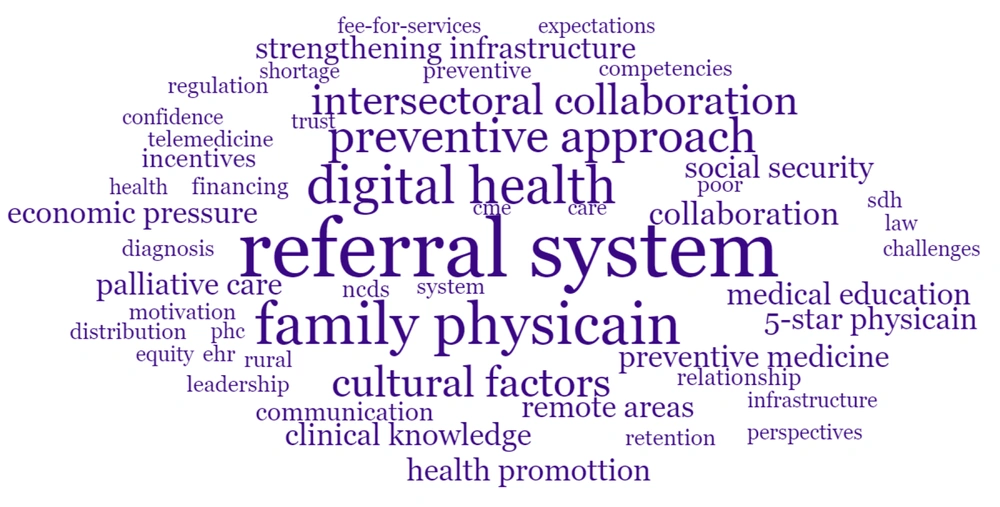
During the data analysis process, 173 primary codes were identified and categorized into four themes: "The Evolving Role of GPs", "The Skills and Competencies of GPs", "Personal Requirements of general practitioner Reinforcement", and "System Requirements of general practitioner Reinforcement". These categories were further divided into 14 subthemes. The themes and subthemes are provided in Table 3. Figure 1 shows the word cloud of domain codes in this study.
| Themes | Sub-theme |
|---|---|
| 1. The evolving role of GPs | 1. The historical development of general practice |
| 2. The current state of general practice | |
| 3. The future of general practice | |
| 2. The skills and competencies of GPs | 1. Clinical knowledge and skills |
| 2. Communication and interpersonal skills | |
| 3. Collaboration skills | |
| 4. Leadership skills | |
| 3. Personal requirements of general practitioner reinforcement | 1. The challenges of being a GP |
| 2. Ongoing professional development | |
| 3. The future directions for general practice | |
| 4. System requirements of general practitioner reinforcement | 1. Strengthening infrastructure |
| 2. Addressing workforce shortages | |
| 3. Promoting intersectoral collaboration | |
| 4. Strong referral systems |
Abbreviation: GPs, general practitioners.
4.1. Theme 1: The Evolving Role of General Practitioners
Most interviews highlighted that the role and responsibilities of GPs in Iran have evolved over time, largely in response to changing public needs.
A core focus of their role remains on preventive care, health promotion, and the management of common conditions affecting the population under their care. Following the COVID-19 pandemic and the widespread adoption of online medical consultation systems, GPs have begun to incorporate virtual consultations and online visits alongside traditional in-person services. This emerging mode of service delivery is expected to become even more prevalent in the future.
Another important factor influencing the evolving role of GPs is the demographic and epidemiological shifts within the population. These external changes highlight the necessity for the ongoing development and empowerment of GPs to meet the dynamic needs of the population effectively.
4.1.1. Sub-theme 1.1: The Historical Development of General Practice
This sub-theme explores the evolution of general practice in Iran, tracing its early beginnings to its current state. It examines various milestones that have shaped the development of general practice over time, including the initial establishment of GP training programs in Iran and other key events that have influenced the field's growth.
4.1.2. Sub-theme 1.2: The Current State of General Practice
This sub-theme aims to provide a comprehensive picture of the current state of general practice in Iran. It examines the roles and responsibilities of GPs, as well as their relationships with other healthcare providers. Additionally, it explores the challenges and opportunities that GPs face in their day-to-day work, such as issues related to workload, resource allocation, and patient care.
4.1.3. Sub-theme 1.3: The Future of General Practice
This sub-theme focuses on potential future directions for general practice in Iran. It considers emerging trends and technologies that will shape the future of the field, as well as broader social, economic, and political developments that impact the role of GPs in the healthcare system.
P 06: “Over time, the roles and responsibilities of GPs in Iran's healthcare system have evolved to include more emphasis on preventive care and health promotion. Additionally, there has been a greater focus on developing and implementing guidelines for the management of chronic diseases such as diabetes, hypertension, and asthma, which is an area where GPs play a critical role.”
P 07: “GPs should be an integral part of a strong referral system that allows them to refer their patients to specialists when necessary.”
4.2. Theme 2: The Skills and Competencies of General Practitioners
This theme refers to the abilities and qualities that GPs need to effectively perform their roles as healthcare providers.
4.2.1. Sub-theme 2.1: Clinical Knowledge and Skills
This sub-theme pertains to the medical expertise and proficiency in diagnosis, treatment, and management of various health conditions that GPs must possess.
4.2.2. Sub-theme 2.2: Communication and Interpersonal Skills
This sub-theme covers the capacity to effectively communicate with patients and other healthcare professionals. It includes not only verbal communication but also nonverbal cues such as body language, tone, and empathy. Trust and confidence are critical factors in establishing a good doctor-patient relationship, which can lead to better health outcomes. Moreover, understanding patients' expectations and needs can help GPs provide more patient-centered care.
4.2.3. Sub-theme 2.3: Collaboration Skills
Collaboration skills involve the ability to work effectively within interdisciplinary teams and to engage in shared decision-making practices with other healthcare professionals. General practitioners need to be able to build trust and negotiate differences to ensure high-quality patient care.
4.2.4. Sub-theme 2.4: Leadership Skills
Leadership skills refer to the ability to motivate and inspire team members, set goals, and manage resources effectively.
P 09: “When a patient comes to me with a chronic condition such as arthritis, I take the time to understand how it affects their day-to-day life and work with them to develop a comprehensive plan that incorporates both medical treatments and lifestyle modifications.”
P 01: “Fortunately, in my experience as a general practitioner in Iran, I have found that most patients have a high level of trust and confidence in their GP. This is partly due to the fact that GPs in Iran are required to meet certain standards of training and education, and often they are talented people in the country.”
P 03: “When a patient has multiple health issues that require coordination between multiple specialists, I work with the patient and other healthcare providers to ensure that they receive the best possible care.”
P 05: “As GPs, we should be able to think strategically and make clear decisions under pressure.”
4.3. Theme 3: Personal Requirements for General Practitioner Reinforcement
General practitioners in Iran generally perceive their role as multifaceted and challenging, given the complex healthcare needs of the Iranian population. While they are trained to provide comprehensive care to patients, many GPs in Iran express that there is a lack of recognition and appreciation for the important work they do in the healthcare system from policymakers' viewpoints.
4.3.1. Sub-theme 3.1: The Challenges of Being a General Practitioner
This sub-theme focuses on the difficulties that GPs face in their daily work. The GPs should be familiar with the challenges in their roles to acquire the skills needed to address these issues. It includes challenges such as heavy workloads, patient expectations, and balancing clinical and administrative responsibilities.
4.3.2. Sub-theme 3.2: Ongoing Professional Development
This sub-theme addresses how GPs maintain and develop their professional skills over time. It includes areas such as continuing education, keeping up to date with medical advances, and professional networking.
4.3.3. Sub-theme 3.3: Future Directions for General Practice
This sub-theme considers the future of the general practice profession. It includes discussions about changing demographics, emerging technologies, and shifting patient needs. Understanding these changes helps GPs prepare for new challenges and provide better care to their patients.
P 09: “There is a lack of recognition and appreciation for the important work that GPs do in the healthcare system.”
P 02: “There are some challenges that GPs in Iran face in fulfilling their roles and responsibilities. One challenge is the shortage of GPs, particularly in rural areas, which can result in a heavy workload for those who are practicing. Another challenge is the pressure to see many patients in a short amount of time, which can impact the quality of care that is provided.”
P 12: “GPs in Iran face various challenges in fulfilling their roles and responsibilities due to several factors, including limited resources, inadequate infrastructure, and a shortage of skilled healthcare professionals.”
P 08: “Most of my time is spent entering information into the systems.”
P 14: “GPs need to receive comprehensive education and training to ensure that they have the necessary medical knowledge and skills to provide high-quality care to their patients. This includes both theoretical and practical training, as well as ongoing opportunities for professional development.”
P 01: “We know that there needs to be a greater emphasis on preventative healthcare measures, increased investment in primary care infrastructure, better integration between primary care providers and specialist services, and an emphasis on digital health solutions and telemedicine.”
4.4. Theme 4: System Requirements for General Practitioner Reinforcement
A large number of interviewees acknowledged that the position of the general practitioner in the Iranian health system needs to be strengthened, and this will not happen unless the family medicine system and referral system are widespread in Iran. Currently, the patient pathway process is very confusing, and the initial point of contact for even simple illnesses is specialist doctors, especially in large cities. Some of the sub-themes that emerged include:
4.4.1. Sub-theme 4.1: Strengthening Infrastructure
Investing in infrastructure such as electronic medical record systems, telemedicine technologies, and referral networks should be considered more than before.
4.4.2. Sub-theme 4.2: Addressing Workforce Shortages
Recruiting and retaining more GPs in underserved areas and improving their working conditions can help ensure that patients have access to high-quality primary care services, regardless of their location.
4.4.3. Sub-theme 4.3: Promoting Intersectoral Collaboration
Encouraging collaboration between various sectors such as health, education, and social services can support the development of more holistic and integrated primary care services.
4.4.4. Sub-theme 4.4: Strengthening the Referral System
Addressing weaknesses in the referral system will require a multifaceted approach, including better communication and coordination between healthcare providers, more comprehensive guidelines for referrals, and improvements in access to specialized care and diagnostic resources.
P 17: “One of the challenges to achieving effective intersectoral collaboration is the limited involvement of non-health sectors such as education, housing, and transportation in healthcare planning and implementation. These sectors play an important role in determining people's health outcomes, and their participation could help address social determinants of health and reduce health inequities.”
P 04: “I believe that there are several weaknesses in the referral system in our healthcare system. One of the main issues is the lack of clear guidelines for referrals. Often, we as GPs are unclear about when and where to refer patients, which can lead to delays in treatment and unnecessary healthcare costs.”
5. Discussion
The study's findings highlight the need for immediate action to address the challenges faced by GPs and to adapt to the changing healthcare landscape to ensure sustainable, accessible, and high-quality primary care services. Additionally, the study underscores the importance of policymakers and health organizations recognizing the critical role of GPs in the healthcare system and providing adequate support to attract and retain these physicians in the field of general practice. Similarly, a paper titled "the future general practitioner: Out of date and running out of time" highlights the challenges that GPs face after completing their training (11). This study argues that the current model of GP training is outdated and inadequate in equipping GPs with the necessary skills and knowledge required to meet the evolving healthcare needs of society. As a result, many GPs lose interest in pursuing a career in general practice. A study by Kringos et al. emphasizes the need for GPs to adopt a more patient-centered approach and engage in health promotion activities, which aligns with the findings of this study (12).
Another significant theme that emerged from this study is the notable change in the role of GPs over the past decade. This finding is consistent with the study by Patterson et al., which highlights the essential competencies required for GPs, including empathy, sensitivity, communication skills, and clinical expertise. These competencies suggest that personal attributes should be given greater consideration in recruitment and training processes (13). The findings of this study align with previous research indicating that patients place great importance on trust, accessibility, and satisfaction with the quality of care delivered by GPs. For instance, a study by Ahmed et al. emphasizes the significance of patient-centered care and improving access to primary care services (14).
The study's findings regarding the challenges faced by GPs and the need for ongoing professional development are consistent with other studies. One study highlights the importance of addressing challenges such as workload and stress to improve job satisfaction and retention in this field (15).
The study's themes on improving training and education align with research by Tulinius and Holge-Hazelton, which shows the need for ongoing professional development and training for GPs (16). Additionally, another sub-theme of this study, focusing on strengthening regulatory frameworks, is consistent with studies emphasizing the importance of developing effective regulatory policies to ensure high-quality primary care services (17-20).
One of the key factors in improving the quality of primary care is enhancing the knowledge and skills of GPs. Several studies have suggested that providing regular training and education opportunities can help enhance the competencies of healthcare providers, ultimately leading to better outcomes for patients (21, 22).
According to the results, effective communication and collaboration between GPs and other healthcare providers are essential for ensuring efficient and coordinated patient care. Studies have shown that communication breakdowns between healthcare providers often result in medical errors and adverse outcomes for patients (23). Therefore, it is necessary to establish effective communication protocols and encourage interdisciplinary collaboration.
The study results reveal that the shortage of GPs and other healthcare providers is a significant challenge that affects the delivery of healthcare services. Several studies have identified that addressing workforce shortages requires strategies such as increasing residency positions, incentivizing general practice, and creating opportunities for international medical graduates to work in underserved areas (24-26).
Overall, GPs play an essential role in healthcare service delivery. They are responsible for providing comprehensive and continuous care to patients, managing chronic diseases, providing preventive care services, prescribing medications, and referring patients to specialists or hospitals when necessary (4).
The study also revealed that there are challenges facing GPs in Iran's healthcare system, including a lack of resources, inadequate training, and a high workload. Despite these challenges, GPs have demonstrated dedication and commitment to their patients and profession.
To improve the quality of primary care services in Iran, there is a need for increased investment in resources, training, and infrastructure. Additionally, policies should be implemented to address the workload and incentivize GPs to remain in primary care practice. Overall, these findings highlight the importance of GPs in Iran's healthcare system and the need for ongoing support to strengthen their role in providing high-quality primary care services.
5.1. Conclusions
The findings of this qualitative study highlight the critical connection between enhancing the role of GPs and strengthening primary health services in Iran. General practitioners play a pivotal role in the healthcare delivery system; however, they face several significant challenges, including inadequate compensation, limited access to continuing education and professional development, an inequitable distribution of resources, and the ineffective implementation of family physician and referral system programs. Additionally, the current healthcare delivery model tends to prioritize specialty care and curative approaches over preventive care.
A top priority should be strengthening the implementation of family physician and referral systems, which requires clear guidelines, training, and support for GPs to ensure their effective integration into the healthcare system. Moreover, shifting the focus from curative to preventive care is essential; the healthcare model must promote public health initiatives and educate GPs about preventive practices. To further strengthen the primary care system and elevate the role of GPs, it is essential to revise and update medical education programs to align them with current healthcare demands. Promoting applied research that addresses societal needs can significantly enhance service quality. Finally, fostering interprofessional collaboration and integrating digital health solutions into primary care will improve the overall performance of GPs in delivering health services.