1. Context
The complexity of hospital activities has led to a corresponding complexity in decision-making. In recent decades, hospitals have sought to optimize their performance by improving decision-making processes through changes in legislation, planning, financing, and organizational structure. This has resulted in changes in various situations, including shifts in power dynamics at the decision-making level. For instance, middle and top managers have been promoted more frequently, while physicians have experienced a decline in their influence. Additionally, employees have enhanced their positions and gained considerable sway in decision-making (1).
The hospital's behavior and orientation are determined by the outcomes and interactions of its decision-making nuclei (2). These interactions illustrate how the hospital responds to various situations and the community's needs. For example, how will the hospital address rising demand, enhance service quality, cut costs, outsource services, and boost revenue? (3, 4). However, the decisions of those in positions of authority should be guided by the goals of ensuring the efficiency, safety, and cost-effectiveness of health services provision, as well as the prioritization of new technologies (3-5).
Identifying key decision-makers can enhance the coordination of hospital strategies and strengthen the priority-setting process (6). Studies have demonstrated that interactions between decision-makers can help hospitals respond more effectively to changes, such as the pressure to increase the quantity and quality of care while reducing costs (7). Identifying power relations can impact clinical supervision and patient referral systems, which are crucial for hospitals and the provision of clinical care services. Consequently, healthcare managers should adopt a dynamic approach to identifying power groups within healthcare systems (8).
Researchers studying healthcare management have raised the question of whether hospitals would perform differently if managed by physicians or professional healthcare managers (9). While both managers and physicians play important roles in hospitals, there is no consensus on which group holds more decision-making power. Furthermore, consultants, such as nurses, are also regarded as pivotal figures within the cohort of specialists (10).
The question of who holds decision-making power in the hospital arises. It is important to determine whether decision-making power lies within the unit, with first-line managers and professional staff, or at a higher level in the organization, with the physician in charge or supervisor. Alternatively, it may lie outside the organization, with unions or politicians (11). Previous research has not comprehensively discussed the critical issues for decision-making and the key decision-makers in hospitals. Therefore, there is no precise definition of the concepts and dimensions involved.
To conduct this study, we used Newhouse's 1970 model of hospital behavioral patterns as a primary framework for identifying decision-makers (12). The Newhouse model is more comprehensive than other models in terms of the decision-makers involved and is also more aligned with hospital conditions. Therefore, it is more appropriate for hospitals as it considers both the decision-makers and the basis of their decisions. The aim of this review is to clarify existing knowledge. The research question is: Who are the influential individuals in hospital decision-making, and what are their areas of responsibility? Answering this question can aid in the professional development of hospital management and health promotion.
2. Methods
2.1. Data Sources
This is a scoping review conducted in January 2024. Scoping reviews aim to provide an exploratory overview of a complex or incompletely researched topic (13-15). Arsky and O'Malley's (16) six-step protocol was used to conduct this study. The protocol includes identifying research questions, identifying related studies using reliable databases, reviewing articles and references in the research area, selecting relevant studies for review from primary studies, extracting data in the form of graphs and tables, and collecting, summarizing, and reporting the findings. Optional consultation with experts about the obtained findings is also included.
The research questions of this study were: "What are the issues that need to be decided in the hospital?" and "Who decides these matters?" Scientific sources were gathered from Web of Science, Scopus, PubMed, and Google Scholar search engines. Additionally, a manual search was conducted for sources related to decision-making issues and decision-makers. The study analyzed articles cited in Newhouse's article by searching for the terms 'Hospital' and 'Decision Maker' both forwards and backwards. Medical Subject Headings (MeSH) such as 'Organizational Decision Making,' 'Hospitals,' and 'Decision Makers' were used in the analysis.
The study's inclusion criteria were English articles published until January 2024 that addressed decision-making and decision-makers in hospitals. Exclusion criteria included studies published in languages other than English, books, conference papers, theses, and any studies related to decision-making and decision-makers in a specific area of health, such as clinical studies or specific diseases.
2.2. Study Selection
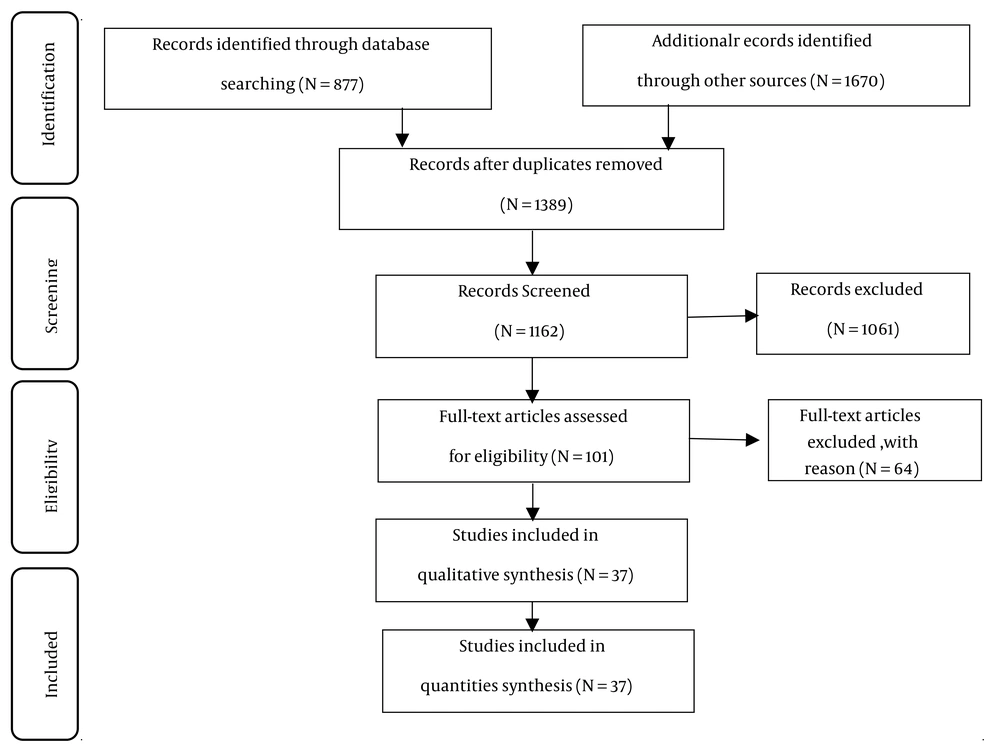
Two researchers independently screened the articles, and any disagreements were resolved by a third researcher. The identified articles were sorted by year of publication. The search scope was expanded by altering the search method and using the sources cited in the obtained articles. A total of 2,547 articles were found. During the initial stage, 1,389 articles were excluded due to repetition, lack of text, theses, books, and non-English language based on their titles. Subsequently, 1,061 unrelated articles were removed after reviewing their abstracts. In the third stage, after a thorough examination of the remaining articles, 64 were eliminated for not mentioning decision-makers. Ultimately, this research utilized 37 articles that were relevant to hospital decision-makers.
2.3. Data Extraction
The 37 articles that formed the basis of this literature review are listed in the appendices. The selected articles were studied, and evidence was extracted using a data extraction form agreed upon by the research team. The form includes sections for the authors' profiles, year of publication, journal name, decision-makers, and cases for which decisions were made.
The study used Lacey's 5-step framework analysis technique for data analysis, which involves familiarization with data, identifying a thematic framework, indexing, charting, mapping, and interpretation (17). Data analysis was conducted using Atlas-ti software. Ethical considerations were adhered to in the review research, including preventing the influence of researchers' opinions on employee perspectives during data collection, analysis, and reporting.
3. Results
The results at different stages are combined in the PRISMA diagram in Figure 1 (18). Thirty-three studies mentioned decision-makers in the hospital. One review focused on evidence-based management in healthcare and also referred to hospital decision-makers. A comprehensive review of the information on hospital decision-makers and the issues they addressed across 37 articles is presented in the appendices.
The study identified a total of 160 indicators used by decision-makers. These indicators were grouped into six categories: Strategic management (organizational strategic planning, hospital social functions, organizational performance management); human resource management (employee performance assessment, hiring and firing of employees, employee allocation, employee training); financial management (maximizing revenue, financial resources, allocation of resources, controlling and reducing costs); employee compensation payment (compensation pay, payment specifications, payment distribution); physical resource management (equipment maintenance, equipment brand, physical facilities development); service delivery management (hospital bed management, patient selection, treatment type selection, services quantity management, services quality management); and hospital reputation (patient satisfaction, hospital prestige, physician skills, hospital appearance). Table 1 shows the classification of 19 decision-makers in the hospital into six categories: Managerial group, physicians group, nursing group, board of directors, government, and political groups.
| Variables | Strategic Management | Human Resource Management | Financial Management | Physical Resource Management | Employee Compensation Payment | Service Delivery Management | Hospital's Reputation |
|---|---|---|---|---|---|---|---|
| Manager | 29 | 12 | 31 | 8 | 10 | 35 | 7 |
| Chairs of departments-head of ward | 7 | 1 | 1 | 1 | |||
| Total | 36 | 13 | 31 | 9 | 10 | 35 | 8 |
| Physicians | 13 | 8 | 24 | 2 | 4 | 30 | 4 |
| Academic faculty | 5 | 1 | 2 | 3 | |||
| Researchers | 4 | 1 | |||||
| Total | 22 | 10 | 26 | 2 | 4 | 33 | 4 |
| Nurses-metron | 6 | 2 | 4 | 2 | 5 | 2 | |
| Board | 11 | 7 | 14 | 6 | 12 | 4 | |
| University | 3 | 1 | 4 | 1 | |||
| Ministry | 3 | 1 | 4 | 1 | |||
| Policy-makers | 4 | 1 | 1 | ||||
| Total | 21 | 10 | 23 | 2 | 6 | 12 | 4 |
| Government | 12 | 6 | 17 | 6 | 5 | 14 | |
| Investors | 4 | 1 | |||||
| Legislatures | 1 | 3 | 2 | 1 | |||
| Municipalities | 1 | 3 | 2 | 1 | |||
| Total | 16 | 8 | 24 | 6 | 9 | 16 | |
| Political groups | 5 | 2 | 5 | 5 | 5 | ||
| Church members | 5 | 1 | 2 | 3 | |||
| Insurance organizations | 3 | 3 | 11 | 1 | 2 | 2 | |
| Medical council | 3 | 1 | 3 | 1 | |||
| Accountants | 2 | 1 | 2 | ||||
| Media | 3 | 1 | |||||
| Total | 16 | 7 | 23 | 2 | 11 | 13 |
4. Discussion
The aim of this study was to identify decision-making issues and the relevant decision-makers in a hospital. The research identified six decision-making groups responsible for decisions on seven issues. The primary decision-makers were the group of managers, who handled three topics: Strategic management, financial management, and the hospital's reputation. They also shared responsibility for human resource management with the board of directors. The following text explains each of the issues and the respective decision-makers.
4.1. Strategic Management
According to the research findings, hospital managers are the primary decision-makers for strategic management issues, with a distinct rank compared to other decision-makers. Senior managers make strategic decisions (19). These findings align with Feldstein's study (20), which suggests that hospital managers, rather than physicians or the board of directors, are the main decision-makers in the operational reality of hospitals. Pauly and Redisch's study (21) suggests that physicians have complete control of the hospital, while Ford-Eickhoff et al. (22) acknowledges the involvement of the board of directors in strategic decisions. Additionally, Jafari et al. (23) argues that the role of the university headquarters or board of directors extends beyond that of managers and physicians. The centralized management approach of administrative units in Iran, which is entirely dependent on the government, may contribute to this situation.
4.2. Human Resource Management
The research findings suggest that the board of directors and managers are the key decision-makers in human resource management. Hospital managers can aid in decision-making by providing resources, including human resources. The board of directors can influence the hospital's focus by intervening in decisions (24, 25). These results are consistent with the research findings of Ancarani et al. (26), Schubert and Willems (27), Seyedin et al. (28), and Jafari et al. (23), but differ from Rayburn, J. M. and Rayburn, L.G.'s study (29), which considers physicians to be the main factor in the hospital's power structure, and Pauly and Redisch's study (21), which also identifies physicians as the primary decision-makers. Additionally, this study disagrees with Xie et al.'s (30) suggestion that government intervention is necessary for hiring and firing hospital employees, and with Doshmangir et al.'s (31) findings that hospitals lack the authority to determine their required staff numbers. In Iran, universities are responsible for hiring and firing employees, while hospitals and their managers have limited involvement.
4.3. Financial Management
The research findings suggest that hospital managers are primarily responsible for financial management decisions. Their main responsibility is to allocate resources to situations where the amount of service provided is greater (20). Managers allocate non-medical resources to physicians to facilitate expensive care (32). This finding aligns with the studies conducted by Vaseva et al. (33), Maleki et al. (34), and Waitzberg et al. (35), which recommend that hospital managers make cost-effective decisions for the operation of the medical center. However, it contradicts the studies by Boadway et al. (32), Rayburn, J. M. and Rayburn, L.G. (29), and Cinaroglu (9). Boadway argued that the government's choice of financing mechanism influences the hospital, while Rayburn acknowledged that hospital accountants determine which departments receive funding. Cinaroglu suggested that physicians can also improve the hospital's financial performance. Baghbanian et al. (36) found that allocation decision-making involves a multifaceted interplay of elements in situations of action. The variation in decision-making among financial managers may be attributed to the wide range of financial matters and associated responsibilities.
4.4. Physical Resource Management
The research findings indicate that the government plays a crucial role in physical resource management, particularly in making resource allocation decisions and in the physical development of hospitals. The government can limit the use of expensive care by controlling the size of hospital equipment through contracts with hospitals (32). These findings are consistent with Xie et al.'s studies (30, 37), which indicate that government intervention at various levels impacts major decisions such as hospital construction and development. However, this contradicts Harris's study (38), which suggests that hospital decisions are solely made by managers and physicians, and Newhouse's study (12), which considers only managers, physicians, and the board of directors as decision-makers. Additionally, Jafari et al.'s study (23) indicates that the university headquarters holds decision-making authority over all hospital properties, while the university's technical office is responsible for repairs and construction. This highlights a potential discrepancy regarding hospital autonomy in Iran compared to other countries.
4.5. Employee Compensation Payment
The research indicates that political groups have a significant influence on employee compensation decisions. This is supported by various studies, including Jensen and Murphy's (39) research, which found that political forces in the public sector significantly impact executive pay and bonuses. Similarly, Eldenburg and Krishnan's (24) study concluded that hospitals pay CEOs less compensation under political pressure. This finding contradicts the studies by Harris (38) and Newhouse (12), which consider managers, physicians, and the board of directors as the primary decision-makers, as well as Jafari et al. (23), who stated that the employee payment system is controlled by the ministry and the government. Furthermore, Jensen and Murphy (39) noted that high payments to managers are influenced by media criticism and ridicule. Differences in decision-making regarding this issue may be attributed to variations in organizational structures across different countries.
4.6. Service Delivery Management
The research suggests that physicians play a significant role in managing service delivery and are closely involved with managers. It is widely acknowledged that physicians can influence hospital policies to some extent (20). This finding aligns with Pauly and Redisch's (21) and Waring's (40) studies, which suggest that physicians have substantial control over hospitals. Rayburn, J. M. and Rayburn, L.G. (29), Boadway et al. (32), Waitzberg et al. (35), and Kirkpatrick et al. (41) have demonstrated that physicians have the legal authority to make decisions, such as selecting hospitals for patients, ordering tests, and choosing treatment methods. Crilly and Le Grand (42) supports this view, stating that physicians determine the quality and volume of services provided. However, studies by Harris (38), Raoofi et al. (43), and Cinaroglu (9) suggest that managers can also enhance the quality of care. Carroll and Ruseski (44) argues that managers play a crucial role in increasing the volume of services provided by hospitals. Jelovac and Macho-Stadler (45) found that insurance can impact the production of health services through contracts.
4.7. Hospital's Reputation
The research indicates that the hospital's reputation is primarily influenced by the group of decision-making managers. However, the reviewed articles did not extensively address this issue, and no significant differences in rank between decision-makers were found. These findings align with Giroti et al. (46) and Ancarani et al.'s research (26), which suggests that managers seek prestige to improve efficiency. Newhouse (12) and Lee (47) identify both managers and physicians as key decision-makers in a hospital's prestige. The hospital's reputation can be affected by several factors, which may contradict these findings. For example, Jafari et al. (23) acknowledges that insurance does not fully cover the cost of hospitals' social functions. Jelovac and Macho-Stadler (45) argues that financial constraints may compromise physicians' quality of work. Crilly and Le Grand's (42) findings highlight nurses as the primary actors in maintaining service quality.
Although the study closely examines decision-making issues and decision-makers in the hospital, caution should be exercised when making policy recommendations based on the scoping review. The research is based solely on the selected articles, and the findings may change with the addition of new articles.
5. Conclusions
Several issues need to be decided within the hospital, and various groups are involved in decision-making, each with different levels of influence. It is crucial to ensure that all decision-making groups are represented and involved in the process. Newhouse's article introduced the main decision-makers in the hospital, including managers, physicians, and the board of directors. However, this research identified six decision-making groups responsible for decisions in seven areas. The majority of the hospital's decisions in these areas were made by managers, physicians, and the government, respectively. Other decision-makers are also concerned with the successful implementation of healthcare policies and laws. These groups include government agencies and ministries, insurance organizations, department heads, nurses, researchers, faculty members, and medical councils. Additionally, policymakers, investors, accountants, political groups, the community, church members, university staff, legislators, municipalities, and the media may also play a role.