1. Context
Migration and addressing the medical needs of migrants is a complex issue in the field of international health that requires an integrated, evidence-based, and human rights-focused response (1). One of the challenges posed by migration is the transfer of infectious diseases from countries of origin to countries of destination, which can increase the risk of infectious diseases not only among immigrants but also among the host population. Common infectious diseases among immigrants include respiratory diseases, tuberculosis (TB), tooth and mouth diseases, malaria, typhoid, hepatitis viruses, and acquired immunodeficiency syndrome (AIDS). Some of these diseases are prevalent in the countries of origin, and immigrants migrating from these regions may be familiar with them (2).
The globalization of infectious diseases due to migration and the movement of people worldwide is a serious challenge to public health. Migration can increase the prevalence of infectious diseases in the new host country, as individuals may be exposed to conditions that facilitate disease transmission (1). Additionally, migrant individuals may face financial, legal, or other barriers to accessing appropriate treatment in host countries, which can exacerbate the disease and its consequences. Therefore, addressing the medical needs of migrants is crucial for preventing the spread of infectious diseases (3, 4). This includes providing access to appropriate treatment, promoting better health conditions, increasing access to healthcare services, and creating better social and economic conditions for immigrants. By taking a comprehensive and human rights-focused approach, we can ensure that migrants receive the medical care they need and prevent the spread of infectious diseases across borders. People with infectious diseases can increase the risk of transmitting the disease to others, especially in cases where the disease has progressed due to an inability to access treatment. Migration may also contribute to increased drug resistance in infectious diseases, stemming from the improper and illegal use of drugs by immigrants and the inability to control this usage. Infectious diseases among immigrants may lead to economic and social consequences for host countries, due to the costs of treatment, reduced productivity, and increased patient numbers (5-8).
Economic factors can significantly impact the risk of infectious diseases among immigrants. Economic crises, in particular, can heighten the risk of infectious diseases among migrants due to their direct and indirect effects on health conditions and the productivity of healthcare systems in host countries (9). During economic crises, decreases in income and increases in inflation can reduce access to food, beverages, and health products, which ultimately decline the efficiency of healthcare systems and increase the spread of infectious diseases. Additionally, economic crises may cause more migration, which, in turn, raises the risk of infectious disease transmission as the migrant population grows (9). Furthermore, economic crises may reduce host countries' ability to provide health services to migrants, leading to decreased access to appropriate treatment and early diagnosis. Therefore, it is necessary to address this issue when planning and implementing health and economic policies.
The risk of infectious diseases can vary across different migratory phases (10). During the pre-immigration stage, immigrants may live in unsanitary conditions and suffer from infectious diseases. During the migration phase, migrants may come into contact with infectious agents in different environments. Finally, immigrants may live in conditions where they have limited access to healthcare services, further increasing the risk of contracting infectious diseases (10-16). Infectious diseases such as TB, smallpox, tooth-and-mouth disease, hepatitis, and AIDS may pose a greater risk to immigrants due to factors such as lack of access to appropriate vaccines, poor sanitary conditions, environmental changes, and unfavorable social and economic conditions (17). Therefore, these issues must be considered when planning and implementing health and economic policies in host countries. To strengthen the health status and prevent invasive infections in the community, health policymakers should implement appropriate measures (18, 19). This includes providing vaccines and access to appropriate healthcare services, promoting better health conditions, increasing access to healthcare services, and creating improved social and economic conditions for immigrants.
There has been significant research on the implications of migration in Latin America, particularly concerning health and infectious diseases. Studies highlight how migration, especially in the context of climate change and socio-economic factors, affects health outcomes. Migrants in Latin America are more vulnerable to infectious diseases like malaria, dengue, and Chagas disease, as well as non-communicable diseases and inadequate healthcare access. Migration has also been studied concerning the spread of vector-borne diseases, which are prevalent in this region (20, 21).
Additionally, climate change can significantly impact global health and the spread of infectious diseases. These changes may increase the risk of contracting infectious diseases due to unfavorable environmental, economic, and social conditions among migrants (10-16, 22-25). Certain diseases, such as malaria, dysentery, leishmaniasis, bacterial lymphoma, and influenza, may become more severe under specific climatic conditions. For example, an increase in temperature could lead to a rise in the number of disease-carrying mosquitoes, resulting in a surge in malaria epidemics in some regions. Similarly, changing rainfall patterns could increase the risk of water-borne diseases, such as smallpox and clostridium. Furthermore, climate change could exacerbate cardiovascular, respiratory, and diabetes-related diseases due to increased air pollution and respiratory risks (26) and pose additional risks to individuals moving across different geographical locations. Thus, this article aims to investigate migration patterns in Latin America and their implications for health and infectious diseases evaluation with a focus on HIV.
2. Objectives
In this comprehensive review, we examined literature investigating the health concerns of migration in Latin America specifically related to human immunodeficiency virus (HIV) infection. We enhanced the validity and authenticity of this study by adhering to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist. Additionally, the risk of bias was assessed using the National Institutes of Health (NIH) quality assessment and risk of bias tool.
3. Data Sources
We conducted an extensive search of the PubMed/MEDLINE online database using a combination of relevant keywords. Articles in the English language were reviewed as of February 26, 2023. Our search strategy executed on the PubMed database was as follows: ("Latin America"[Mesh] OR Latin America[tiab]) AND ("Human Migration"[Mesh] OR "Emigration and Immigration"[Mesh] OR Migration[tiab] OR Emigration[tiab] OR Immigration[tiab] OR Border Crossing[tiab] OR Diaspora[tiab]) AND ("HIV"[Mesh] OR HIV[tiab] OR Human Immunodeficiency Virus[tiab] OR AIDS Virus[tiab] OR Acquired Immune Deficiency Syndrome Virus[tiab] OR Acquired Immunodeficiency Syndrome Virus[tiab] OR HIV-1[tiab] OR HIV-2[tiab]).
4. Study Selection
To enhance the selection process, we employed a two-step method. In the initial step, two researchers screened the titles and abstracts of the retrieved articles against the inclusion and exclusion criteria. In the second, more comprehensive step, three researchers thoroughly read the full texts of the screened articles. Pertinent articles meeting the inclusion/exclusion criteria were advanced to data extraction. Articles were included if they were original, English, peer-reviewed, and specifically assessed the issue in Latin America. Studies were excluded if they involved non-human research participants, were ongoing, lacked published data, were duplications, umbrella or narrative reviews, abstracts without accessible full texts, conference abstracts, editorial letters, preprint papers, case series, or case reports. The inclusion and exclusion criteria were aligned with the PICOTS framework, explicitly defined as follows:
- Population: Migrants in Latin America.
- Intervention/exposure: Migration and its associated health and social factors, with a particular focus on HIV and other infectious diseases.
- Comparator: Not applicable for this study, as the focus was on the descriptive synthesis of migration's health implications.
- Outcomes: Prevalence and burden of infectious diseases, specifically HIV, and associated health challenges such as mental health issues.
- Time: Studies published up to February 26, 2023, with no restrictions on the time of data collection in the included studies.
- Study type: Peer-reviewed original articles, excluding narrative reviews, editorials, case reports, preprints, and conference abstracts.
5. Data Extraction
The extraction of relevant data from the eligible articles was performed by three independent researchers and entered into a spreadsheet (Table 1). The final results were reviewed by other team members to prevent duplication and ensure the accuracy of the extracted data.
| Authors, References | Gender (N) | Age a | Country of Origin | Destination Country | Disease or Syndrome | Study Population | High-Prevalence Regions | Risk Factors for Health | Reasons for Migration | Main Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Cassels et al. (27) | Male (16) | 35 (23 - 54) | Mexico: 13; El Salvador: 2; Texas: 1 | USA, California | HIV+, mental health | Latinx migrant MSM | N/A | Using drugs | Access to health supports | N/A |
| Crabtree‐Ramirez et al. (28) | Male (1,900,000) | N/A | Latin America | Venezuela, Argentina, Chile, Colombia, Mexico, Peru | HIV+ | MSM, transgender women, sex workers, people who inject drugs | Brazil | Drug use and dependence, STIs, new sexual partners | Lack of existing healthcare infrastructure for HIV care and the unavailability of international financial support | Migration significantly impacts HIV care and control programs, but through regional collaboration across borders, and international funding, assisting migrants and providing coordinated healthcare services, can be feasible |
| Konda et al. (29) | Female (494) | (18 - 24), (25 - 34), (> 34) | Mexico, Peru, Brazil | N/A | HIV+, TB, DM | MSM, cisgender men | Peru | Transactional sex, STIs, sex partners, binge drinking, Stimulant use | N/A | N/A |
| Obach et al. (30) | Male and Female (17) | (18 - 25) | Ecuador, Colombia, Venezuela, Peru | Chile | N/A | Young pregnant women, young migrants, adolescent, international migrants | N/A | Sexual violence, racism, sexual abuse | Access to healthcare and social contexts of reduced gender, the need to have access to healthcare and the social pressure of reduced gender discrimination | N/A |
| Ottenheimer et al. (31) | Female (14) | 37 (SD = 6.4) | ElSalvador, Guatemala, Honduras, Mexico | USA | HIV+ | Migrant, adult women with a history of sterilization | N/A | Sterilization, sexual violence, the presence of pervasive poverty, lack of protection from law enforcement, emotional abuse, discriminatory behavior | Coerced sterilization at the hands of their health care providers in their countries of origin | N/A |
| Page et al. (32) | N/A | N/A | Latin America | USA | HIV+/mental health | Latinx immigrants | N/A | Diverse sexual relations | Economic, social, and political forces | N/A |
| Huerta-Vera et al. (33) | Male (N = 360, 90.5%) | 30 (26 - 37) | Venezuela | Peru (Lima) | HIV+ | PLWH: 398 | N/A | N/A | Socioeconomic crisis/the health system deterioration | Facilitate legal status with migration policies and regulations/expanding access to diagnostic tests/interventions to strengthen patient-centered HIV services |
| Rashak et al. (34) | Male (3198); female (2310) | > 18 (mean ± SD = 43.7 ± 17.4) | Central America (Guatemala, Honduras, El Salvador), the Caribbean (Haiti, Cuba), South America (Ecuador, Brazil) | Mexico (Chiapas) | HIV+, TB, DM | New adult TB patients diagnosed: 5508 | Tapachula (Mexico) | Under-nutrition, alcoholism | Better job opportunities/escaping from areas of conflict | N/A |
Abbreviations: HIV, human immunodeficiency virus; TB, tuberculosis; DM, diabetes mellitus; PLWH, people living with HIV/AIDS; STIs, sexually transmitted infections; MSM, men who have sex with men; N/A, not applicable.
a Values are presented as age (range) unless otherwise indicated.
5.1.Quality and Risk of Bias Evaluation
As mentioned above, the reliability of the included papers was obtained by adhering to the preferred reporting items for PRISMA checklist and bias risk was evaluated using the NIH tool for quality and bias risk assessment. Table 2 demonstrates the summary of the assessment for included articles using NIH. Two independent researchers assessed and rated the included studies based on the questionnaire at the bottom of the table. The rating scores of individual papers are presented in the last two columns of Table 2. In cases of disagreement, a third independent researcher resolved the issue.
| First Authors | Questions | Rating by Reviewers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | A | B | |
| Cassels et al. (27) | Yes | Yes | CD | NR | Yes | Yes | CD | Yes | CD | Fair | Fair |
| Crabtree‐Ramirez et al. (28) | Yes | Yes | CD | Yes | CD | N/A | CD | N/A | Yes | Fair | Fair |
| Konda et al. (29) | Yes | Yes | CD | Yes | NR | NR | Yes | Yes | CD | Fair | Fair |
| Obach et al. (30) | Yes | Yes | CD | NR | NR | Yes | Yes | CD | Yes | Fair | Fair |
| Ottenheimer et al. (31) | Yes | NR | CD | N/A | CD | Yes | Yes | Yes | Yes | Fair | Fair |
| Page et al. (32) | Yes | Yes | CD | Yes | NR | Yes | NR | CD | Yes | Fair | Fair |
| Huerta-Vera et al. (33) | Yes | Yes | NR | Yes | CD | Yes | NR | Yes | CD | Fair | Fair |
| Rashak et al. (34) | Yes | Yes | CD | NR | Yes | Yes | CD | Yes | CD | Fair | Fair |
Abbreviations: CD, cannot determine; NR, not reported; N/A, not applicable.
6. Results
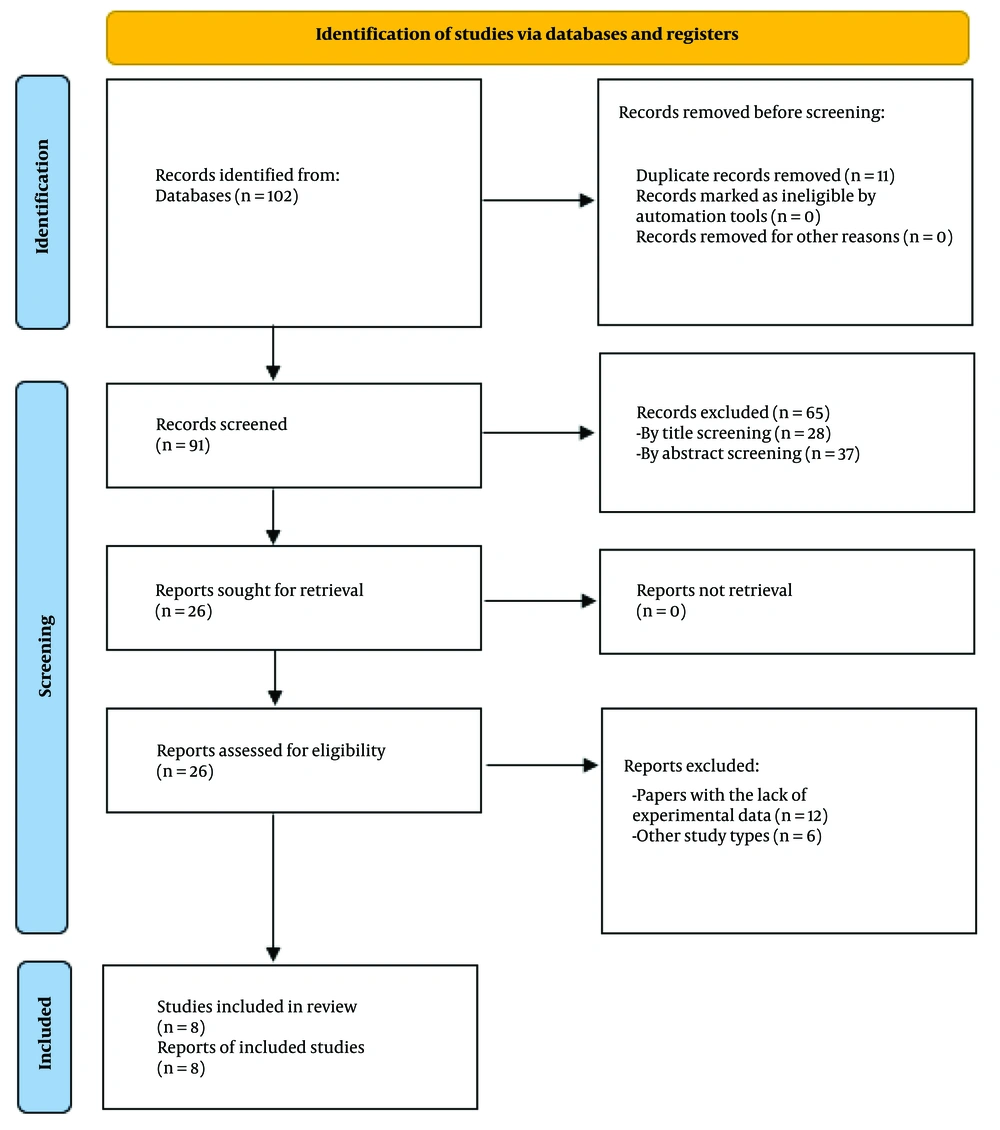
In total, 102 documents were identified using a comprehensive search strategy. After the initial screening, 11 duplicate studies were excluded, and the titles and abstracts of 91 studies were thoroughly reviewed. Applying the inclusion and exclusion criteria, 83 studies were removed, leaving 8 studies for the final evaluation (Figure 1). The necessary data, including the name of the first author (reference), participants' sex and age, country of origin, destination country, disease or syndrome, study population, high-prevalence regions, health risk factors, reasons for migration, and a summary of findings, were extracted and organized in Table 1.
In total, 1,904,387 individuals with an average age of 31.10 years were included in this systematic review. The main countries of origin were Mexico (n = 3) and El Salvador (n = 3), with other regions and countries such as Latin America (n = 2), Brazil (n = 2), Ecuador (n = 2), Venezuela (n = 2), Peru (n = 2), Guatemala (n = 2), and Honduras (n = 2) also represented. The most frequent countries of destination were Chile (n = 2), Mexico (n = 2), Peru (n = 2), and the USA (n = 2). The main diseases or syndromes identified were HIV infection, mental health issues, TB, and diabetes mellitus (DM).
The included studies represent a heterogeneous population consisting of men who have sex with men (MSM), transgender women, sex workers, people who inject drugs, cisgender men, young pregnant women, adolescents, internal and international migrants, adult women with a history of sterilization, people living with HIV/AIDS (PLWH), and newly diagnosed adult TB patients (Table 1).
Brazil, Peru, and Tapachula were identified as regions with a high prevalence and burden of disease attributable to migration. Risk factors faced by migrants in different phases of migration included drug use and dependence, sexually transmitted infections (STIs), transactional sex, binge drinking, stimulant use, sexual violence and abuse, racism, sterilization, poverty, lack of protection from law enforcement, emotional abuse, discriminatory behavior, diverse sexual relations, under-nutrition, and alcoholism. In general, economic, social, and health system crises were among the reasons for migration in this study.
Some studies suggested solutions to improve the welfare and status of immigrants through internationally funded initiatives (28), such as overcoming the risk approach and focusing primarily on maternal health (30), facilitating legal status by advocating for migration policies and regulations (33), expanding access to diagnostic tests (33), and interventions to strengthen patient-centered HIV services (33).
7. Discussion
This study aimed to investigate migration patterns in Latin America and their potential health implications, with a particular focus on infectious diseases, especially among people living with HIV. Migration in Latin America has been a long-standing challenge, with countries in the region serving as both origin and destination. According to the latest reports, the number of immigrants in Latin America increased from 7 million in 1990 to 15 million in 2020 (35). Our findings indicate that Mexico and El Salvador are the main countries of origin for migration, likely due to economic instability, government corruption, and high rates of crime and violence in these regions (36).
Immigrants have diverse motivations for migrating, which can be classified into three main categories. The first category is health issues, including lack of access to healthcare and inadequate infrastructure for HIV care. People, especially those living with HIV, may be compelled to migrate to seek medical care or escape discrimination and stigma related to their HIV status or sexual identity. A study in Peru indicated that HIV-infected Venezuelan migrants diagnosed in Peru had better outcomes for viral suppression (74.2% vs. 70.7%) and virologic failure (6.9% vs. 16.5%) compared to those diagnosed in Venezuela (33). According to a qualitative study, a group of young immigrant women in Chile reported that prenatal and gynecological services in Chile were of superior quality compared to their country of origin (30).
The second category is economic status, encompassing factors such as poverty, insufficient financial support, and limited employment opportunities. In interviews with young Latin American migrants, all expressed that improving their quality of life and economic status was their primary motive for migration (30). The last category is social issues, including gender discrimination, sexual violence, sexual abuse, and discriminatory behavior. Of all the transgender women reported murdered worldwide from 2008 to 2015, 78% were killed in Latin America (28). A cohort study in the USA on immigrant women who had undergone forced sterilization revealed that most had experienced prolonged physical or emotional violence and sexual abuse (31). A qualitative study found that migrants chose destination countries with progressive societies that welcomed gender-based diversities and prioritized their rights (27).
Our study reveals that Chile, Mexico, the USA, and Peru were the most common destination countries for Latin American migrants. Several factors contribute to this trend, including favorable migration policies, a well-organized health system providing care to a significant portion of the population, and support for vulnerable groups with a high burden of disease. These destination countries offer a higher quality of life and better economic opportunities. According to a study, LGBTQ immigrants expressed gratitude for the acceptance and freedom to openly express their sexual identities in their new country of residence. Research indicates that immigrants continue to face challenges even after arriving in their destination country (32). A study in Peru demonstrated that 10% of the study population did not begin antiretroviral therapy due to financial problems (33). Poverty, lack of social support, and high medical care costs make HIV care unaffordable. Another study in Chile showed that violence and discrimination towards immigrants are common, coming from both native residents and established immigrant communities (30).
Improving health outcomes in Latin America requires an approach that considers the difficulties experienced by the population. Strategies to improve health outcomes, especially among people living with HIV, include expanding access to diagnostic tests for prevention and early diagnosis, and checking viral load and CD4 count to prevent disease progression. Latin America has a significant number of intravenous drug users at high risk of HIV. To reduce this risk, there is a need for a structure to design, finance, and implement strategies aimed at reducing HIV incidence among at-risk individuals. To enhance global HIV control, policymakers should implement migration policies and regulations that enable legal status and appropriate medical care for vulnerable groups and special cases. Such measures could significantly improve HIV control, especially in regions with high migration rates (28, 30, 33).
Regarding other studies on migration's impact on HIV spread and prevalence, it has been reported that from 2007 to 2012, migrants were responsible for two-fifths of HIV cases reported in the European Union (37). Moreover, a strong association was found between migration and HIV prevalence in women in Sub-Saharan Africa (38), and HIV-1 non-B variants significantly increased in the last 10 to 15 years in the Maghreb and Southern Europe due to migration from West Africa (39). Unfortunately, studies on migration and its impact on HIV spread and prevalence in the Middle East and North Africa (MENA) are limited.
Although the quality of the included studies in our review was relatively fair with a low risk of bias, different study designs and populations may impact our understanding of the situation. Additionally, our study focused on Latin America, so the findings may not fully apply to other regions, such as MENA, due to cultural, social, and healthcare system differences. For future directions, exploring understudied regions such as MENA by leveraging findings from Latin America and Sub-Saharan Africa may be beneficial.
Overall, achieving better health outcomes in Latin America requires a strategic approach involving regional leadership and cooperation to ensure policies are coordinated with local needs. These approaches require international funding to support intervention implementation. Our strategies must be evidence-based, addressing specific challenges faced by Latin Americans, and should consider all factors, especially socio-economic and health, to shape health outcomes.
7.1. Conclusions
In conclusion, this systematic review highlights the health implications of migration in Latin America, with a focus on HIV infection. Despite the limited number of studies that met the inclusion criteria, the findings suggest that several factors influence the health of Latin American immigrants, including economic, social, and health system disadvantages. The study found that HIV infection, mental illness, TB, and DM were among the common diseases and syndromes affecting migrants. The high-prevalence countries were Brazil, Peru, and Tapachula. The most common countries of origin were Mexico and El Salvador, while the most common destination countries were Chile, Mexico, Peru, and the USA.
However, the study has limitations, including the limited number of studies available and potential sources of bias or confounding factors that may have influenced the results. The studies also reveal diverse health risk factors associated with migration, including drug use, binge drinking, and malnutrition. Another limitation was that many studies focus on marginalized populations such as Latino immigrant MSM, transgender women, sex workers, and intravenous drug users, highlighting the need for targeted interventions to address the unique health challenges faced by these groups.
Finally, this review relied on a single database, PubMed/MEDLINE, which may have introduced selection bias by excluding studies from other high-profile databases such as Scopus, Web of Science, and Cochrane. While this approach was chosen to maintain focus and feasibility, it may have omitted relevant studies that could provide a more comprehensive understanding of the topic. Future reviews should expand the scope by incorporating additional databases and grey literature to address this limitation and ensure a broader perspective on migration and health.
The findings of this study call for more attention and resources to be directed toward improving the health outcomes of migrants in Latin America, particularly concerning infectious diseases like HIV. These findings can also inform the development of evidence-based interventions to improve health outcomes for migrant populations, especially concentrating on infectious diseases. In addition, the findings underscore the importance of addressing the underlying social and economic factors that drive migration in the region. Further research is needed to investigate the health implications of migration in this region and to identify effective strategies to mitigate these problems.