1. Background
Optical coherence tomography (OCT) is a non-invasive imaging modality widely used for obtaining high-resolution cross-sectional images of the retina, optic nerve, and other anatomical structures of the eye. This technology works by measuring the reflection of near-infrared light to create detailed images, allowing for a thorough evaluation of various ocular conditions, including macular degeneration, glaucoma, and diabetic retinopathy (1).
A major advancement in intraoperative OCT (IOCT) systems was the integration of OCT with microscope optics, enabling real-time visualization of instrument-tissue interactions. This innovation provides immediate imaging feedback to surgeons, enhancing precision and efficiency during surgical procedures. The incorporation of z-tracking and focus controls into these devices has further improved image stability and quality, ultimately contributing to better surgical outcomes (2).
Previous research, including the landmark Pioneer and Discover studies (3, 4), has explored the role of intraoperative OCT in ocular surgeries. These studies were conducted in resource-rich settings with relatively balanced patient turnover. Optical coherence tomography has been demonstrated to be a non-invasive and highly effective tool that enhances visualization in the surgical field.
2. Objectives
The aim of this study was to evaluate the feasibility and utility of deploying intraoperative OCT in a developing country where limited resources necessitate efficient and productive use. Additionally, the role of intraoperative OCT in cases of retinal detachment was specifically assessed.
3. Methods
3.1. Study Design and Participants
A case series study involving fifteen patients was conducted at a tertiary care facility, the Layton Rahmatullah Benevolent Trust (LRBT) Eye Hospital in Lahore, Pakistan. All surgeries were performed by a single senior consultant to ensure consistency in assessment across cases. The Enfocus microscope-integrated intraoperative optical coherence tomography (Bioptigen/Leica Microsystems, Wetzlar, Germany) was utilized. The study was initiated following approval from the hospital and in adherence to the principles of the Declaration of Helsinki. Informed consent was obtained from all patients.
Patients with retinal detachments scheduled for retinal surgery through the outpatient department (OPD) were included. The clinicians ensured that either the patients themselves or their guardians provided written informed consent. Both male and female patients aged 10 - 70 years were eligible for inclusion in the study.
3.2. Questionnaire
The diagnosis, diagrams of retinal pathology, and the required surgical procedures were documented in a tabulated format. A questionnaire was designed for the surgeon to complete after each surgery, evaluating the effectiveness of the modality in identifying critical surgical landmarks and any modifications made to the original surgical plan.
3.3. Data Analysis
The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS), version 25.0 (IBM Statistics, Chicago, IL, USA).
4. Results
A total of 15 patients with retinal detachment as the primary pathology and a mean age of 35.33 ± 8.27 years (95% confidence interval) were included in the study (Table 1). Clear OCT images were successfully obtained in 100% of the cases. Key surgical landmarks identified included epiretinal membranes, posterior vitreous detachment, areas of vitreomacular traction, and subretinal fluid.
| No. | Age (y) | Diagnosis and Relevant Retinal Findings | Vitreoretinal Surgery | Specific Indication of Using Intraoperative OCT | Utility of Intraoperative OCT | ||
|---|---|---|---|---|---|---|---|
| Identification of Important Retinal Structures | Surgeon’s Decision Making | Confirmation of Surgeon’s Surgical Decision | |||||
| 1 | 60 | Retinal detachment | PPV with silicon oil tamponade | To rule out any macular pathology such as macular edema or AMD | Yes | No | Yes |
| 2 | 16 | Re-retinal detachment | Redo PPV with silicon band | To rule out sub-retinal oil preoperatively and confirmation of retinal attachment at the end of surgery | Yes | No | Yes |
| 3 | 45 | Rhegmatogenous retinal detachment | PPV with silicon oil | To confirm the presence of detachment and to rule out any sub-retinal oil after the procedure. | Yes | No | Yes |
| 4 | 40 | Myopic retinal detachment with PVR and multiple retinal breaks | PPV with silicon oil | To confirm the presence of ERM and completion of posterior vitreous detachment as the vitreous was very adherent | Yes | Yes | Yes |
| 5 | 66 | Inferior bullous retinal detachment with extensive macular scarring | Inferior band + PPV with silicon oil | To confirm the cause of macular scarring, which turned out to be active choroidal neovascularization and ensure complete removal of perfluorocarbon | Yes | Yes | Yes |
| 6 | 61 | Diabetic vitreous hemorrhage with TRD | PPV with silicon oil | To ascertain the location of TRD and residual ERMs | Yes | Yes | Yes |
| 7 | 30 | Emulsified silicon oil causing glaucoma | Removal of silicon oil | Removal of silicon oil revealed macular hole, which was confirmed using intraoperative OCT | Yes | No | Yes |
| 8 | 28 | Traumatic retinal detachment with ERM | PPV with silicon oil | To confirm retina attachment and any remnant ERM after ERM peeling | Yes | No | Yes |
| 9 | 24 | Total retinal detachment with PVR | Band + PPV + silicon oil | To determine the presence of any ERM and confirmation of complete removal of heavy liquid and retinal attachment at the end | Yes | No | Yes |
| 10 | 20 | Diabetic TRD | PPV + silicon oil | To confirm the removal of tractional elements. | Yes | No | Yes |
| 11 | 35 | Total RD | PPV + silicon oil | To confirm the removal of silicon oil | Yes | No | Yes |
| 12 | 15 | Retinal detachment with very adherent PVD | PPV + silicon oil | To assess the completion of PVD and any residual traction on the macula | Yes | No | Yes |
| 13 | 27 | Diabetic TRD with extensive ERMs | PPV + silicon oil | To confirm any remnant retinal tractions and ensure complete removal of ERMs | Yes | No | Yes |
| 14 | 25 | Traumatic retinal detachment | PPV with silicon oil | To confirm retina attachment after PPV | Yes | No | Yes |
| 15 | 38 | Rhegmatogenous retinal detachment | PPV with silicon oil | To confirm the presence of detachment at the end of the procedure. | Yes | No | Yes |
Abbreviations: OCT, optical coherence tomography; PPV, pars plana vitrectomy; TRD, tractional retinal detachment; ERM, epiretinal membrane; PVR, proliferative vitreoretinopathy.
4.1. Instances Where Intra-Operative Optical Coherence Tomography Altered the Surgical Plan
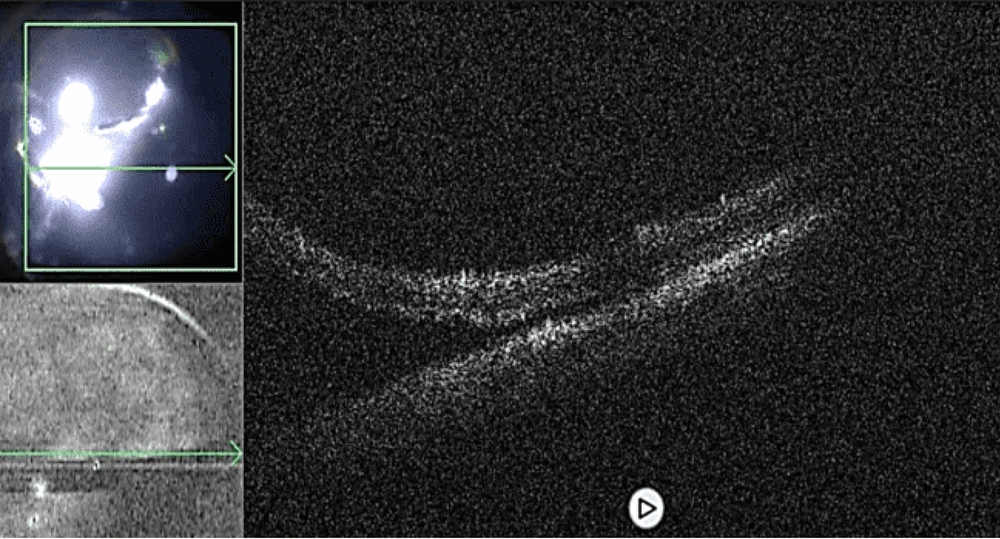
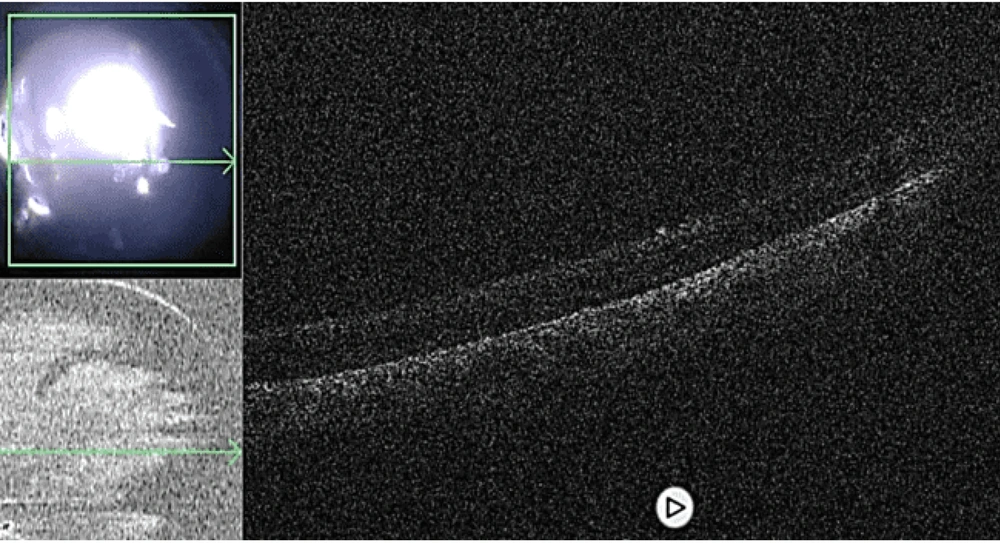
The surgeon modified the surgical plan in 4 cases of retinal detachment surgery (36%). In two cases, IOCT allowed the surgeon to identify residual subretinal fluid (Figure 1), which had appeared perioperatively to have been fully drained with the retina successfully reattached. Based on the IOCT detection of residual subretinal fluid, additional drainage was performed, and further images were taken to confirm both the completion of drainage and successful retinal attachment (Figure 2). In another two cases, IOCT facilitated the delineation of adherent vitreous at the posterior pole, which was not visible through the surgical microscope. This enabled the surgeon to complete the posterior vitreous detachment (PVD) successfully.
4.2. Instances where Intra-Operative Optical Coherence Tomography Assisted the Surgeon During the Surgery
In cases of retinal detachment surgery, IOCT assisted the surgeon in confirming the successful reattachment of the retina before proceeding to the next step. Additional maneuvers, such as the removal of silicone oil and heavy liquid, were performed under IOCT visualization, further guiding the surgeon’s course of action.
5. Discussion
Intraoperative optical coherence tomography offers numerous advantages, including real-time visualization of the surgical field and enhanced accuracy in evaluation and guidance during the surgical process (5, 6). The use of this technology has been shown to empower surgeons to make informed decisions and immediate adjustments, thereby improving the overall quality of surgical outcomes (7, 8).
Landmark research has demonstrated that IOCT usage leads to changes in surgical decision-making in a substantial proportion of cases, ranging from 29.2% to 43% (9, 10). For example, a clinical trial on retinal detachment repair surgeries revealed that IOCT provided significant feedback to surgeons in 36% of cases, resulting in surgical decision changes in 12% of cases (11). Additionally, another study showed that during surgeries for proliferative diabetic retinopathy, surgeons found IOCT valuable in approximately 50.6% of cases, with a discernible impact on surgical decision-making in 26% of cases. These findings highlight the considerable influence of IOCT in improving surgical outcomes and guiding clinical management strategies (12).
This investigation confirmed that IOCT led to modifications in the surgical approach in 36% of retinal detachment surgery cases. The research underscores the importance of IOCT in identifying critical anatomical features, such as the extent of posterior vitreous detachment and the presence of epiretinal membranes.
Notably, IOCT enabled the surgeon to confidently confirm the successful reattachment of the retina, allowing the procedure to be concluded with a high degree of certainty. However, several limitations of the study must be acknowledged. The small sample size restricts the generalizability and validation of the findings. Furthermore, the mere presence of IOCT in the operating room does not guarantee the surgeon's proficiency in its effective use. The IOCT is a novel and advanced modality with a significant learning curve, requiring surgeons to undergo extensive training to maximize its utility.
Additionally, the accessibility of IOCT may have introduced a bias among surgeons in favor of using the system for guidance, which could have influenced the outcomes and the resulting conclusions. Addressing these limitations will be essential for future studies to validate the broader applicability and effectiveness of IOCT in diverse surgical settings.
5.1. Conclusions
The use of this technology has been shown to significantly influence the decision-making process of surgeons, particularly in retinal detachment surgeries, where precise and timely interventions are essential for successful outcomes. The ability to visualize detailed anatomical structures and pathological changes intraoperatively through OCT scans enhances the surgeon's capacity to accurately assess the situation and make informed decisions, ultimately improving surgical outcomes in retinal detachment procedures.