1. Background
Stroke is the most prevalent neurological disorder and the leading cause of long-term disabilities, imposing significant financial burdens on society and families (1-3). Post-stroke impairments include muscle weakness, alterations in muscle tone, sensory and cognitive issues, restricted range of motion, pain, spasticity, and muscle coordination disorders (4, 5). Delays in initiating motor activity, timing, sequencing of muscle activity, and asynchronous muscle contractions contribute to postural synergy disorders, leading to balance and gait disturbances (6, 7).
Balance disorder is the most common functional impairment following a stroke, affecting approximately 83% of patients (8, 9). Balance disturbances are a critical predictor of falls (10). Reduced balance control, low confidence in balance, and a high incidence of falls are common post-stroke outcomes, negatively impacting patients' quality of life and daily activities, often resulting in social isolation (11). Falls can cause injuries, fractures (notably hip fractures) (12), prolonged hospitalization, and further diminish quality of life, thereby increasing financial strain (8).
Reactive and proactive balance responses are impaired in stroke patients (12). Predictable postural strategies, or proactive control, operate via a feedforward mechanism and involve anticipatory reactions initiated by the individual. Any voluntary movement, particularly rapid ones, can cause postural disturbances by shifting the body's center of gravity. These movements can be partially anticipated by the central nervous system, which regulates postural muscle activity both before and in response to disturbances (13). Predictable postural strategies manage the body's center of mass by activating trunk-stabilizing muscles prior to limb movement and anticipated disturbances, thereby minimizing displacement. These strategies are developed through learning and prior experiences (14). Compensatory postural strategies, or reactive control, function via a feedback mechanism and involve compensatory reactions triggered by sensory feedback signals. These strategies restore the body's center of mass to a stable range following an unexpected disturbance (15). Reactive postural control is essentially the ability to respond swiftly after a balance disturbance (16).
DE Kam et al. (as cited by Handelzalts) reported that automatic postural responses in chronic stroke patients are delayed and smaller in amplitude (12). Previous studies have indicated that the slowness of voluntary proactive steps, combined with the ineffective and delayed implementation of reactive steps to increase the range of stability when balance is unexpectedly disturbed, significantly increases the risk of falls in these patients (12). A primary goal in the rehabilitation treatment of these patients is to enhance postural control and balance (17). Recovery of motor activities post-stroke may occur due to neuroplasticity in the brain (7).
In recent decades, numerous advanced methods have been employed in stroke rehabilitation, including robotic technology and virtual reality. However, traditional treatment methods such as conventional exercises, proprioceptive neuromuscular facilitation (PNF), and functional movements continue to be utilized. Some studies have demonstrated that voluntary balance control is significantly improved with conventional exercises focusing on walking training, weight lifting, and muscle strengthening (1). Additionally, perturbation-based balance exercises have been shown to be effective in improving the speed of voluntary movements, enhancing quick balance reactions, controlling reactive balance, and reducing fall rates in stroke patients. However, the impact of these exercises on overall balance performance and maintenance remains inconclusive (11).
2. Objectives
Despite numerous studies conducted in the field of exercise therapy to enhance the balance of stroke patients, there remains a lack of robust and sufficient evidence demonstrating the effects of specific balance exercises focused on various dimensions of balance and identifying which types of exercises are most effective. Consequently, this study was designed and implemented. It is structured to align with the current conditions in physiotherapy clinics, utilizing therapeutic exercise methods that do not require special equipment or impose exorbitant costs on the patient and therapist. The present study aimed to compare conventional physiotherapy exercises with specialized reactive and proactive exercises in stroke patients. The authors hypothesize that the use of reactive and proactive exercises will improve the balance performance of these patients more effectively than conventional exercises.
3. Methods
This study is a double-blind randomized clinical trial. All stages of the study, including initial clinical evaluations and treatment sessions, were conducted in the Physiotherapy Department of Ayatollah Kashani Hospital in Isfahan, from July 2022 to March 2024. Participants willing to join the study were required to sign a written ethics consent form. Eligible patients were then randomly allocated into experimental groups (reactive and proactive) and a control group (conventional). Patients were assigned to these groups using the random block method by the clinic secretary, who was unaware of the study details. The patients themselves were blinded to their group assignments and the differences between groups, with separate visit times to maintain blinding. Ethics approval was obtained from the Medical Ethics Committee of Isfahan University of Medical Sciences (IR.MUI.RESEARCH.REC.1399.224), and the study protocol was registered in Iran's prospective clinical trial registration system (IRCT20200101045970N1).
Eligibility criteria included a history of the first unilateral stroke confirmed by a neurologist through CT scan or MRI findings (18), a minimum of 6 months since the onset of stroke symptoms (16, 19), a suitable cognitive state to understand and follow simple verbal commands (18, 19) based on the Persian version of the mini-mental status examination (score ≥ 24), the ability to stand and walk independently without aid (5), and muscle spasticity in the gastrocnemius (Modified Ashworth Scale score ≥ 1) (18). Exclusion criteria included the presence of other neurological disorders such as Parkinson's disease or diabetes (16), severe vision, depth, and vestibular disorders (5), severe orthopedic disorders such as fixed contracture in the lower limb (18), severe pain in the lower limb (VAS Pain Scale score between 75 and 100 mm) (20), participation in other physical therapy interventions (18), use of drugs affecting balance function (tone, sensory system, and muscle strength) (21), weight over 150 kg, and height over 1.2 meters (22).
The sample size was calculated based on previous similar studies using the following formula, considering a 95% confidence level and 80% test power (16). The estimated sample size was 10 participants per group (reactive exercises, proactive exercises, and control), totaling 30 participants:
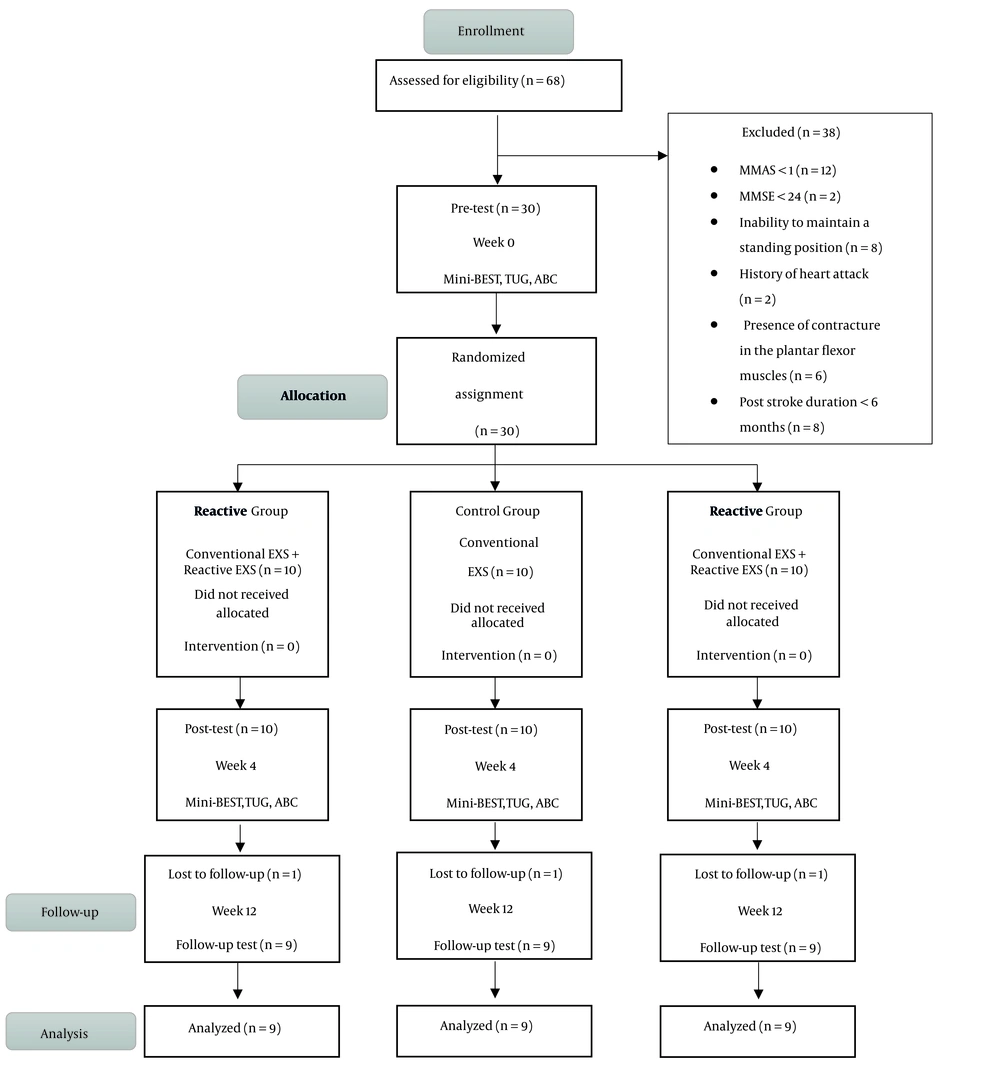
Sixty-eight individuals with stroke were evaluated, and 38 were excluded from the study due to not meeting entry criteria, meeting exit criteria, or declining participation. Thirty stroke patients were randomly assigned to one of the three groups: Control, reactive, and proactive (Figure 1).
3.1. Tools and Methods of Data Collection
The evaluation of study outcomes was conducted in three stages: Before the intervention, at the end of the treatment period, and two months post-treatment. All evaluations were performed by a physiotherapist who was blinded to the treatment groups.
3.1.1. Mini Balance Evaluation Systems Test
This tool is used to evaluate balance performance, and its validity has been established for stroke patients in previous studies (23, 24). The test comprises 14 items, each requiring the patient to perform a specific activity. A physiotherapist, blinded to the group assignments, scores each item from 0 to 2, which indicates weak, average and normal, respectively. The test takes approximately 10 to 15 minutes to complete (25).
3.1.2. Activities-Specific Balance Confidence Questionnaire
This questionnaire assesses the level of confidence in balance during daily activities and has demonstrated high reliability for stroke patients, as confirmed in prior studies (26, 27). The ABC questionnaire can be completed by the individual or by others and includes 16 items. For each item, the individual rates their self-confidence in performing the activity without losing balance, on a scale from 0% (no self-confidence) to 100% (full confidence).
3.1.3. Treatment Protocol
Following the initial evaluation, participants in all three groups underwent treatment for 12 sessions over 4 weeks (3 sessions per week, on alternate days) (18). Each treatment session for the control group lasted 35 minutes, comprising 5 minutes of warm-up, 25 minutes of common balance exercises, and 5 minutes of cool-down. For the two experimental groups, sessions lasted 60 minutes, including 5 minutes of warm-up, 25 minutes of common balance exercises, 25 minutes of specific balance exercises (reactive or proactive), and 5 minutes of cool-down at the end. Five types of exercises were designated for each group, with 5 minutes allocated to each exercise, repeated 2 to 5 times within the 5-minute period.
Conventional physical therapy, as outlined in previous studies, included lower limb range of motion exercises, weight-bearing on the affected side, walking in parallel bars forward, backward, and sideways, hip bridging exercises, and stretching exercises (28). All balance exercises were conducted under the direct supervision of a physiotherapist. Reactive exercises included perturbation while sitting, perturbation while standing, pushing and releasing the person, standing on an unstable surface, and performing the cowboy exercise using a physical therapy ball. Proactive exercises included catching and throwing a ball, spinning, reaching, standing on one leg, and tandem walking.
3.1.4. Data Analysis Method
All statistical analyses of the collected data were performed using IBM SPSS statistics version 20. The Shapiro-Wilk test was used to assess data distribution. One-way ANOVA and repeated measures tests were applied to normally distributed data, while non-normally distributed data were analyzed using the Kruskal-Wallis test. A P-value of less than 0.05 was considered statistically significant.
4. Results
The mean and standard deviation of background variables and quantitative control for all three treatment groups are presented in Table 1. According to the ANOVA test, there were no statistically significant differences between the three groups in terms of age and Body Mass Index (BMI) (P > 0.05). Similarly, the Kruskal-Wallis test indicated no statistically significant difference in stroke duration among the groups (P > 0.05).
| Variables | Proactive Group (n = 10) | Reactive Group (n = 10) | Control Group (n = 10) | 95% CI for Mean | P-Value | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Age (y) | 57.90 ± 8.47 | 10.64 ± 63.20 | 33.10 ± 90 .52 | 54.10 | 61.90 | 0.083 |
| BMI (kg/m2) | 54.25 ± 37.3 | 40.2 ± 22.73 | 3.57 ± 54.25 | 23.36 | 25.85 | 0.090 |
| Post stroke duration (mo) | 26.5 ± 17.03 | 14.32 ± 14.70 | 22.79 ± 25.90 | 15.43 | 29.31 | 0.288 |
Abbreviation: BMI, Body Mass Index.
a Values are expressed as mean ± SD.
The number and frequency of qualitative background variables, including gender, involved side, type of stroke, use of an assistive device, and spasticity score, are reported in Table 2. According to the Kruskal-Wallis test, there were no statistically significant differences between the three groups regarding the frequency of these qualitative variables (P > 0.05).
| Variables | Proactive Group (n = 10) | Reactive Group (n = 10) | Control Group (n = 10) | P-Value |
|---|---|---|---|---|
| Gender | 0.517 | |||
| Female | 2 | 4 | 2 | |
| Male | 8 | 6 | 8 | |
| Affected side | 0.631 | |||
| Left | 6 | 8 | 7 | |
| Right | 4 | 2 | 3 | |
| Stroke type | 0.404 | |||
| Ischemic | 5 | 7 | 4 | |
| Hemorrhagic | 5 | 3 | 6 | |
| Assistive device | 0.592 | |||
| Yes | 5 | 5 | 7 | |
| No | 5 | 5 | 3 | |
| Spasticity score | 0.857 | |||
| 1 | 0 | 2 | 2 | |
| 2 | 7 | 3 | 5 | |
| 3 | 3 | 5 | 3 | |
| 4 | 0 | 0 | 4 |
4.1. Analytical Statistics of Study Outcomes
4.1.1. Intra-group Comparison of Balance
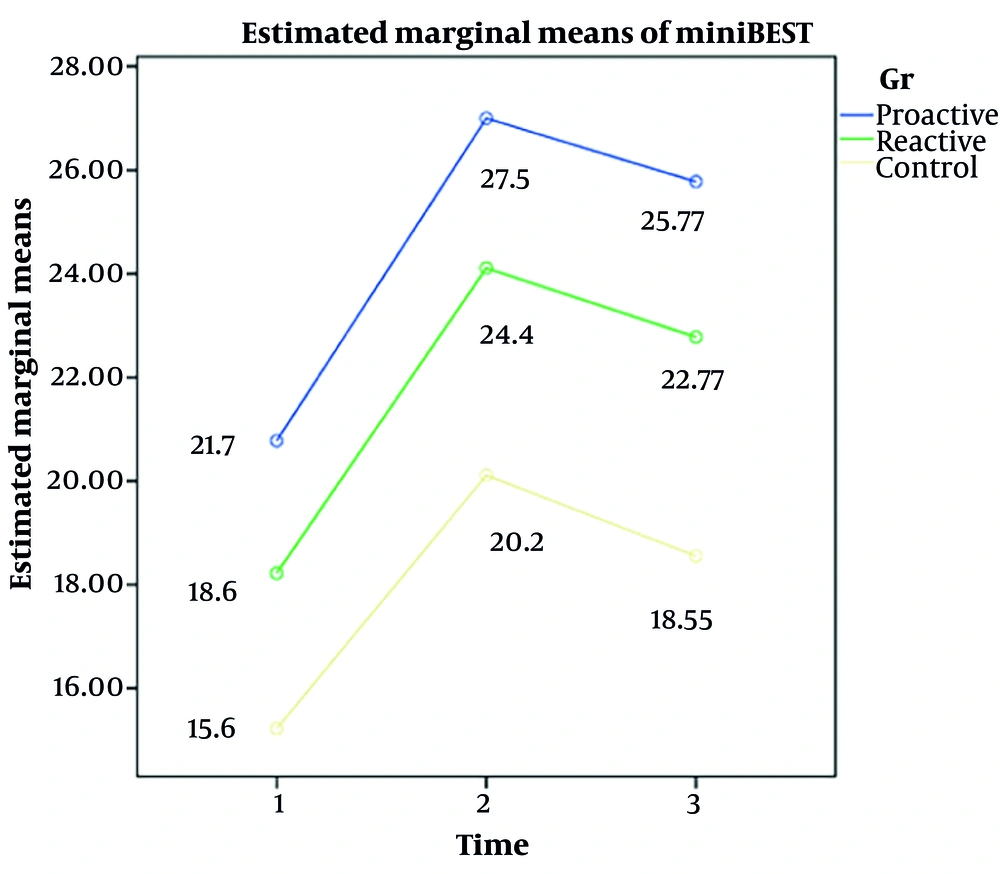
The results indicated that the level of balance increased significantly in all three groups—proactive, reactive, and control—when comparing pre- and post-treatment periods (P < 0.05) (Figure 2).
4.1.2. Between-Group Comparisons of Balance
The results showed a statistically significant difference among the proactive, reactive, and control groups (F = 64.694; P < 0.001; ηp2 = 0.729). However, the interaction between time and group was not statistically significant (F = 0.516; P = 0.724; ηp2 = 0.041). Additionally, the difference between the groups was not statistically significant (F = 1.874; P = 0.175; ηp2 = 0.135) (Table 3).
| Variables | Time Effect | Time × Group Effect | Group Effect |
|---|---|---|---|
| Balance confidence | df = 2, F = 76.002, P = 0.00 | df = 4, F = 0.348, P = 0.844 | df = 2, F = 1.269, P = 0.299 |
| Balance | df = 2, F = 64.694, P = 0.00 | df = 4, F = 0.516, P = 0.724 | df = 2, F = 1.874, P = 0.175 |
The statistical results suggest that all three methods improved balance in stroke patients, but there is no statistically significant difference among the three methods.
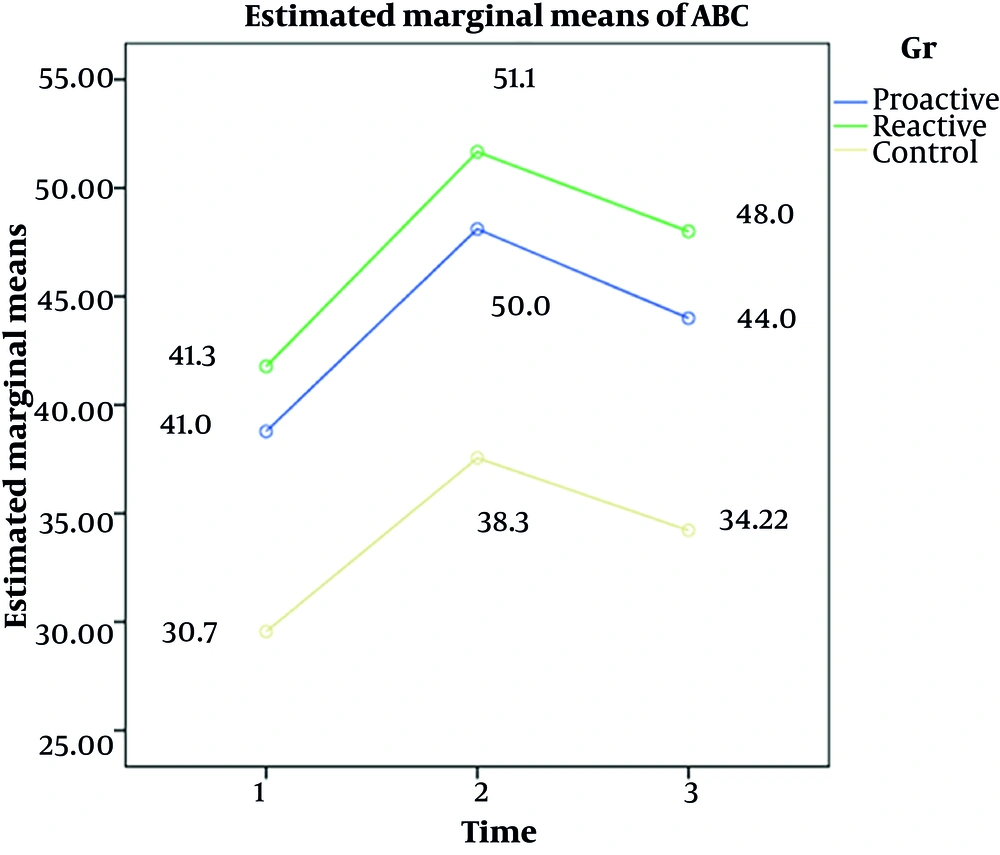
4.1.3. Intra-group Comparison of Balance Confidence
The analysis revealed that balance confidence significantly increased in all three groups—proactive, reactive, and control—following the treatment period (P < 0.05) (Figure 3).
4.1.4. Between-Group Comparisons of Balance Confidence
The results demonstrated a statistically significant difference across the proactive, reactive, and control groups (F = 76.002; P < 0.001; ηp2 = 0.760). However, the interaction between time and group was not statistically significant (F = 0.348; P = 0.844; ηp2 = 0.028). Additionally, the difference between the groups was not statistically significant (F = 1.269; P = 0.299; ηp2 = 0.096) (Table 3).
The statistical results suggest that all three methods effectively improved balance confidence in stroke patients, although no statistically significant difference was observed among the methods.
5. Discussion
The results of this study indicate that reactive and proactive balance exercises, as well as conventional exercises, lead to significant improvements in balance and balance confidence in stroke patients. At the conclusion of the treatment, balance performance in the proactive group was superior to that in the reactive group, while balance confidence was higher in the reactive group compared to the proactive group; however, these differences were not statistically significant.
In stroke patients, the locomotor pathways that control balance, walking, and proprioception are often impaired (29). Balance disorder is the most common physical impairment during the chronic stage of stroke (30). A systematic review by van Duijnhoven et al. reported that walking training, weight transfer, and balance exercises are effective treatment methods for improving balance capacity in the chronic stage of stroke (17). Balance disorders in these individuals are associated with decreased balance confidence (31).
Studies have shown that in the sub-acute stage of stroke, the relationship between reactive balance control and the fear of falling (as measured by the ABC questionnaire score) is weak (12). At this stage, patients may not accurately assess their ability to recover balance in unexpected situations, as they have not been sufficiently exposed to various obstacles and conditions to control reactive balance. In the chronic stage, stroke patients have more real-life experiences with balance reactions (12). During this stage, individuals who fear falling exhibit lower balance abilities compared to those who do not fear falling (12).
Alayat et al., in a systematic review of seven clinical trial studies, suggested that perturbation-based training (PBT) significantly improves reactive balance in stroke patients but does not have a significant effect on improving balance confidence (11). The lack of significant results in enhancing balance confidence may be attributed to the limited number of studies and small sample sizes for statistical analysis (11). Research has shown that improvements in balance and physical performance enhance the quality of life for these patients (32). A primary goal of rehabilitation treatment for stroke patients is to improve balance (17). Exercise therapy is an effective and accessible method that does not require expensive equipment or incur exorbitant treatment costs. In the present study, all three treatment groups received conventional exercises.
Balance control encompasses both proactive and reactive control (33), with past studies indicating a moderate correlation between them (12). Patients with low reactive balance abilities also exhibited lower levels of proactive balance control (12). Kannan et al.'s study found that conventional exercises do not significantly affect reactive balance control. They noted that although reactive and proactive balance control share some neurophysiological and biomechanical components, reactive balance control may not improve significantly against large disturbances due to its specific performance with exercises based on voluntary movements (1).
The ability to maintain balance and prevent falls is facilitated by balance reactions (11). These balance reactions are often impaired in individuals with stroke, increasing their risk of falling (12). A study by Schinkel-Ivy et al. demonstrated that PBT is effective in improving reactive stepping in stroke patients (22). In reactive exercises based on disturbances, individuals are repeatedly exposed to unpredictable external disturbances, either manually by the therapist or through the use of unstable surfaces (11). Previous studies have shown that these exercises improve the control and speed of voluntary movements, enhance quick balance reactions, reduce fall rates, and improve reactive balance in stroke patients (8, 11). Therefore, specific reactive exercises such as PBT, which focus on these aspects, appear to be more effective than other exercises in preventing falls (11). In a study, Mansfield et al. compared reactive PBT exercises with body mass supporters to traditional balance exercises in chronic stroke patients and concluded that reactive exercises are more effective in improving reactive balance control (16).
The effect of PBT in the subacute phase of stroke is greater than in the chronic phase because patients experience significant recovery due to neuroplasticity in the first weeks following a stroke. After approximately three months, the recovery rate plateaus and then decreases significantly, with limited recovery observed after six months. Therefore, it is recommended that these exercises be initiated as soon as possible (11). In the present study, participants were in the chronic stage of stroke (> 6 months).
As expected, the performance of balance and confidence in balance improved significantly in all three groups—conventional exercises, reactive exercises, and proactive exercises—compared to pre-treatment levels. However, the differences between the groups were not statistically significant. The results may have been influenced by uncontrolled confounding factors such as variations in participants' underlying conditions, movement capacity, and differences in their reactive and proactive balance abilities. Additionally, the lack of significant differences between groups might be due to reactive exercises having a greater effect on reactive balance control and proactive exercises having a greater effect on proactive balance control, with the overall balance performance being compared in the evaluation.
In most studies, the outcomes of proactive and voluntary balance control are assessed. Clinical measurements of proactive balance do not fully capture reactive balance performance. It seems more appropriate to evaluate reactive balance control using specific methods alongside balance performance evaluation methods (12). In a limited number of studies, reactive balance was assessed using perturbations of low frequency and amplitude, which may not sufficiently disturb balance and do not represent real-life perturbations (1). Future studies should identify tests that offer more advantages than traditional tests, such as the Berg Balance Scale, for assessing balance and fall risk, and demonstrate a stronger correlation with measures of reactive balance.
In this study, the Mini-BESTest was used to evaluate balance and compare results among the reactive, proactive, and control (conventional exercises) groups. The Mini-BESTest assesses all components of balance, including reactive and proactive balance (33). Due to time constraints, the sample size in this study was relatively small, and the follow-up period was short. A larger sample size would have allowed for separate comparisons of different components of the Mini-BESTest (such as reactive and proactive balance), but in this study, the overall score was compared across groups.
According to the inclusion and exclusion criteria (ability to walk independently for a short distance), participants in this study had good scores in functional balance tests and balance confidence, with a relatively high level of motor function post-stroke. Therefore, this study does not fully reflect the situation of the entire population of stroke survivors. Future studies should include a larger sample size, employ a random recall strategy with less restrictive criteria, and have a longer follow-up period to achieve more accurate results in this area.
5.1. Conclusions
In the present study, both at the end of the treatment period and after the follow-up period, balance and balance confidence showed significant improvement in all three treatment groups compared to pre-treatment levels. We conclude that balance exercises enhance balance in individuals with stroke, and exercise therapy is an essential component of rehabilitation treatment for these patients. Given that intergroup comparisons did not reveal a significant preference for reactive or proactive balance exercises over conventional exercises alone, further high-quality studies are necessary to obtain more definitive results in this area. A more effective method is needed to evaluate and compare the effects of reactive and proactive exercises on different dimensions of balance.