1. Context
Non-suicidal self-injury (NSSI) involves behaviors like cutting, burning, and self-hitting, often linked to alcohol/substance use, childhood trauma, poor emotional regulation, and co-occurring disorders such as borderline personality and eating disorders. Recognized as a distinct disorder (1, 2), NSSI affects 15 - 30% of school-aged youth, especially those aged 12 - 14 (1, 3-5). While it may temporarily relieve anger or distress, it often leads to guilt, shame, and recurring negative emotions (6, 7). The NSSI is a significant mental health concern due to its psychological and social impacts, concealment, and role as a coping mechanism for life stressors (8). It is a strong predictor of suicide, highlighting the need for prevention and intervention (9). Adolescents with NSSI vary in injury types, frequency, and causes (10). Those engaging solely in NSSI often have greater self-functioning impairments than those with additional problem behaviors (11). Repeated NSSI in adolescence signals significant emotional issues and increased suicide risk (12-14). The NSSI differs from suicidal self-harm and non-injurious behaviors like problematic eating or social isolation (15). Here, NSSI refers to intentional self-harm without suicidal intent, while "self-harm" includes a broader range of behaviors, including suicidal actions.
To address the need for three-tiered preventive interventions in school-age children (16), recent research highlights the importance of improving school environments to tackle NSSI and enhance student mental health. This approach emphasizes the roles of teachers, school nurses, and staff (3, 17-24). Given the significant amount of time students spend in schools (25, 26) and the high prevalence of NSSI in this age group, schools are uniquely positioned to identify and support youth struggling with NSSI (27, 28). Adolescents often avoid seeking help for NSSI (29). Prevention requires non-judgmental support and educating teachers, peers, and parents (30, 31). Reducing mental health stigma in schools is vital (32). Staff must actively detect and respond to NSSI to encourage help-seeking (33-35). Barriers include NSSI invisibility, negative attitudes, over-reliance on referrals, and school issues like bullying and poor teacher-student relationships (36, 37), perpetuating NSSI in schools.
Efforts to address NSSI in schools, distinct from suicidal behaviors, began in the 1990s, but systematic reviews are lacking. Current interventions for school staff need improvements in effectiveness, acceptability, and feasibility (35). Universal school-based programs have been ineffective in addressing risk behaviors, with none targeting NSSI (18), revealing a research gap. To our knowledge, no similar systematic review with the same criteria was available globally.
2. Objectives
This review is performed to evaluate school-based NSSI interventions, providing insights and future directions.
3. Methods
This systematic review employed a narrative synthesis method to evaluate school-based interventional programs (SBIPs) targeting NSSI in students. Narrative synthesis was chosen for several reasons. First, SBIPs are often context-specific and creatively designed, resulting in heterogeneous interventions with shared and unique features. Additionally, this approach allows for an effective examination of both the effectiveness and implementation strategies of SBIPs, with a focus on the context rather than solely the function of the interventions.
3.1. Data Sources
Potential articles were identified through a systematic search strategy across three major databases: Web of Science, Medline/PubMed, and Scopus. The search focused on titles, abstracts, keywords, and MeSH terms, using a sensitive PICO-based strategy tailored for each database. Studies published between 1990 and April 2022, and only those in English, were included.
3.2. Study Selection
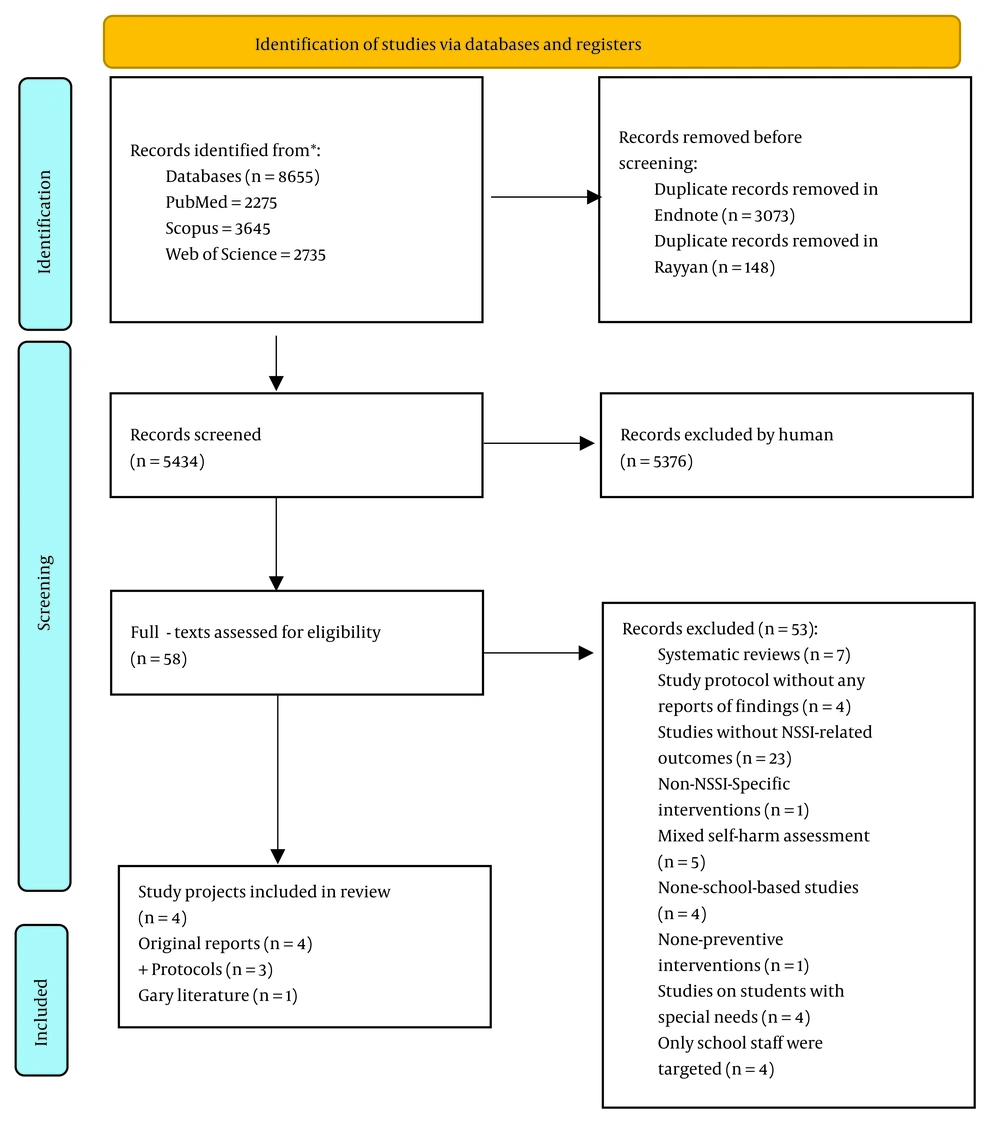
Articles were included if they: (A) targeted school students with preventive interventions delivered in school settings (curriculum-based or after-school), (B) considered NSSI as a primary or secondary outcome, alongside other relevant outcomes, and (C) used quasi-experimental or randomized control trial designs. Exclusions applied if: (A) interventions were non-preventive or not school-based, (B) non-suicidality was not clearly defined in self-harm assessments or mixed outcomes were reported, (C) systematic reviews, (D) study protocols without any reports of findings, (E) mixed self-harm assessments, (F) studies on students with special needs, and (G) only school staff were targeted. For data extraction, two reviewers independently screened articles using Endnote and RAYYAN Web applications (38), resolving inconsistencies through discussion. Titles and abstracts were screened for relevance, excluding irrelevant papers at this stage. Relevant articles underwent full-text review. Additional sources, such as gray literature, were identified through manual searches on Google Scholar, reference lists, and related reviews.
3.3. Data Extraction
Data extraction was conducted by two author-reviewers who collaboratively designed a data extraction sheet to capture essential information for synthesis. The sheet was reviewed by the remaining authors, who supervised the process and provided critical feedback. The final extraction sheet comprised three sections: (1) Participant demographics, (2) methodological details of included studies, and (3) outcomes, including NSSI and related results. This ensured a comprehensive and systematic approach to data collection and analysis.
The quality evaluation was conducted using critical appraisal tools from the Joanna Briggs Institute (JBI), specifically the checklist for quasi-experimental research with 9 items (non-randomized experimental research) and the checklist for randomized controlled trials with 13 items (39). Studies lacking a control group were considered low quality, as their prospective results would not be comparable to a random error. The narrative synthesis approach was used to capture the depth of included articles and highlight diversities in methodologies, theories, and implementation procedures (40). It relies on textual descriptions, rather than quantitative data, to aggregate findings from studies with heterogeneous methods addressing the same research question. Two broad categories — effects and implementation of interventions — were identified as primary steps to evaluate the included studies. A preliminary synthesis was conducted to determine the main themes for in-depth analysis. Techniques such as tabulation, grouping studies, and thematic analysis were used to present the findings. To ensure robustness, critical reflection was integrated into the synthesis process, where authors challenged each other’s suggestions to ensure a thorough examination of the reviewed papers.
4. Results
A total of 8,655 entries were initially identified. After removing duplicates, 5,434 entries were screened. Ultimately, four studies met the selection criteria, including three original articles (41-43) and one dissertation as gray literature (44). Additionally, three study protocols and manuals related to the interventions (45-47) were included in the synthesis. Figure 1 illustrates the PRISMA flow diagram of the screening process. Table 1 summarizes adolescent participants across studies, totaling 1,063 (679 intervention, 348 control). Mean ages were 14.12 ± 0.90 for intervention and 12.86 ± 0.60 for control groups, with signs of self-Injury (SOSI) study participants (n = 274) having the highest mean age of 16.07 ± 1.32. Interventions included 485 males (16 controls) and 503 females (21 controls), with Happyles excluding NSSI (43). Mean age by gender was not calculable.
| Study Projects/ Location | First Author, Year (Reference) | Male (N) | Female (N) | Total Sample (N) | Mean Age (SD) |
|---|---|---|---|---|---|
| SOSI/USA | Muehlenkamp, 2010 (41) | 133 in intervention group only | 141 in intervention group only | 274 in intervention group only | 16.07 (1.32) |
| DA/UK | Rowe, 2018 (42) | Four DA, five controls | Six DA, eight controls | 10 DA, 13 control | 14.2 DA, 13.77 control |
| SBISY/Mexico | Byrum, 2019 (44) | 25 intervention, 11 controls | 30 intervention, 13 control | 55 Intervention, 24 control | 12.27 (0.45) intervention at follow-up, 12.54 (0.72) at follow-up |
| HappylesPLUS/Belgium | Baetens, 2020 (43) | 323 in both intervention groups | 326 in both intervention groups | 651 total sample, with 311 pupils receiving general mental health Happyles intervention, and 340 pupils receiving NSSI-added HappylesPLUS intervention | 12.85 (0.77) for total 651 pupils |
| Total | - | 485 male students receiving any intervention, 16 male controls with no intervention | 503 female students receiving any intervention, 21 controls with no intervention | 1063 participants, including 679 intervention groups and 348 controls | 14.12 (0.90) for intervention groups and 12.86 (0.60) for controls |
Study Reports and Samples Demographic Characteristics
The SOSI study, a universal preventive program (41), involved five high schools (33.3% of 15 targeted schools) in a pilot study, with eight student dropouts (Table 1). Conducted in spring 2008, it included both at-risk and non-at-risk students. Participants were primarily Caucasian (72.96%), Hispanic/Latino (6.30%), African-American (5.56%), Asian-Pacific (3.70%), and other (11.48%).
The DAs program, titled My Self-Help Tool, targeted English-speaking adolescents aged 12 - 18 (primarily 12 - 15) in a London secondary school with a history of self-injury in the past 12 months (44, 48). From 1,167 approached pupils, 208 (17.87%) obtained parental consent, with 170 (81.7%) recruited over 10 months (October 2015 - July 2016). The final sample included 23 participants (10 intervention, 13 controls) with no attrition or missing data. A four-week follow-up was conducted. All intervention participants were white, while two controls identified as mixed or other (not of British Asian, Caribbean, or African descent) (42).
The school-based intervention stress youth (SBISY) study focused on middle school-aged students in Juventino Rosas, Mexico. A convenience sample of 97 sixth-grade students from a primary school was recruited in June 2017, with 63 followed up in seventh grade across four secondary schools in June 2018. A non-equivalent control group of 25 was assessed only at follow-up. No participants were excluded due to lack of consent, but eight from the intervention group and one control dropped out, leaving 79 eligible participants. Approximately 90% reported having at least one immediate family member who migrated to the USA.
The HappylesPlus study included 651 pupils (11 - 15 years, 86.7% response rate) from six Belgian secondary schools selected for prior NSSI incidence. Participants, with equal gender distribution, were randomized into Happyles (n = 311, suicide prevention) and HappylesPlus (n = 340, with NSSI module). Both programs ran simultaneously over six weeks (February - March 2017), with follow-up interviews six weeks later. Declines were due to educational and iatrogenic concerns. Only age and gender data were reported (43).
The suicide prevention program, previously effective in school settings (45), evaluated feasibility and effectiveness among high school students. It aimed to enhance NSSI knowledge, referral capabilities, help-seeking behaviors, and reduce one-month NSSI incidence (41). A two-week pilot study informed schools and participants about procedures and obtained consent before implementation (41).
The DAs study, a selective preventive program, was a parallel-arm, single-blind RCT with a four-week follow-up. Using multi-criteria decision analysis (MCDA) (46), it assessed data completeness, randomization acceptability, recruitment/attrition rates, school-based sampling feasibility, study power, preliminary effectiveness, and stakeholder perceptions (42). Of 1,167 approached pupils, 208 (17.87%) consented. Participants were screened using the SMFQ and self-reported NSSI engagement (42). Outcomes included a 1 - 6 Decision Stage Scale, GHSQ for disclosure willingness, QUAD for stigma experiences, and Decisional Conflict Scale subscales for decision-making difficulties (46).
The SBISY study, a universal prevention program, used a pre-test-post-test design with a one-year follow-up and a non-equivalent comparison group assessed only at follow-up (44). Of 97 participants, 55 completed the intervention, and 24 comparisons were added later. It aimed to improve stress management and coping skills to reduce self-harm, measured via self-cutting, alcohol, and drug use, alongside the Stress in Children (SiC) scale (44).
The HappylesPlus study used a pre-test-post-test design with an active control group (Happyles, excluding NSSI psychoeducation). Randomization allocated groups, with HappylesPlus nested within Happyles, a universal program targeting mental health, emotion regulation, coping, help-seeking, positive psychology, and destigmatization. The pilot evaluated the NSSI module’s effectiveness, iatrogenic effects, and NSSI outcomes (e.g., onset, urges, and frequency). Validated tools included BNSSI-AT, YOQ-SR, PMHSS, ATSPPH-SF, and DERS. No quantitative follow-up was conducted, but 15-minute qualitative interviews were held six weeks post-implementation (43).
The SOSI intervention (45) involved a 50-minute session with an introduction, an 18-minute video, a 20 - 25 minute discussion, and a self-assessment including a Help-Seeking Index, led by a trained counselor. Feasibility interviews with conductors were held post-follow-up.
The DAs study utilized an online program, My Self-Help Tool, on Annalisa© and Elicia© platforms (46). Based on subjective utility analysis, the Tool assists decision-makers by providing data and alternatives aligned with their preferences. It offers scenarios to help youth choose support sources (family, peers, teachers, professionals). Piloted for usability and language appropriateness (46), the Tool also included feasibility interviews with participants, parents, and teachers.
The SBISY study delivered a three-session preventive intervention using DBT and CBT-based stress psychoeducation. Each 90-minute session included icebreakers, relaxation, and topics like stress coping (session 1), active listening and peer support (session 2), and automatic thinking/mindfulness (session 3). Group discussions, exercises, and materials (e.g., sticky notes, flip charts, and dolls) were used. No feasibility interviews or pilot studies were conducted (44).
HappylesPlus, nested within Happyles, added a classroom psychoeducation session on NSSI. Participants received general mental health psychoeducation in two interactive classroom lessons and two 50-minute e-health lessons on positive psychology (happiness) and problem-solving. The HappylesPlus session included an introduction, a documentary on hope and support, discussions on self-care, help-seeking, NSSI prevention, contagion, and social media concerns, and a relaxation exercise. The intervention addressed positive emotions, coping skills, cognitive distortions, help-seeking, and destigmatization (43).
Using the JBI Critical Appraisal Checklist, the HappylesPlus study (43) scored high quality (11/11) for quasi-experimental research, while the DAs study (42, 46) scored moderate quality (10/13) for CRTs. The SOSI study (41) was rated low quality due to the lack of a control group, reducing internal validity. Similarly, the SBISY study (44) was rated low quality as it used a grade-matched control group assessed only at follow-up, compromising study design.
Table 2 summarizes intervention effects on NSSI outcomes. The SOSI study observed a potential decline in NSSI acts over the following month (28 vs. 14 incidences, P = 0.079), but found no significant changes in NSSI-related thoughts, frequency, or internet use (41). This could be a potential signal warranting larger trials. In the SBISY study, NSSI assessment via self-cutting, drug, and alcohol use (stress-relief behaviors) showed that self-cutting doubled in the intervention group (n = 6 at baseline, n = 12 at follow-up). This may be due to iatrogenic effects as a potential outcome. Alcohol use decreased (n = 5 at baseline, n = 2 at follow-up), while drug use remained unchanged (n = 1 at both baseline and follow-up) (44).
| Author (y) Location | Study Nature | Study Protocols | Study Setting | Study Design | Intervention | Experiment Group | Control Group | Measures | Pre-test NSSI Rate | Post-test NSSI Rate | Follow-up NSSI Rate | Preventive Practice | Overall Results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SOSI (Muehlenkamp et al., 2010), Wisconsin, USA (41) | Universal | Jacobs, 2009 | Five US high schools | Pre-test/post-test without control group | One 50-min session presented at Health classes, with introducing the topic, showing video components (approximately 18 minutes), and facilitating in class discussions using the discussion guide (approximately 20 - 25 minutes) in addition to 4 - 6 weeks post-implementation sessions | 214 students from five high schools in 2007 - 2008 academic year | N/A | Self -injurious Thoughts and Behaviors Inventory (56), some NSSI-related items were adopted from Evaluative Survey of the Signs of Suicide Program (73). including whether anyone knew about their self-injury (e.g., friend, parent, counsellor, sibling, teacher, doctor); knowing friends purposefully hurt themselves (as well as numbers and group self-injurie); NSSI-specific use of internet | Thought of NSSI n = 49, with mean frequency of 3.50 (1.92) and mean intensity of 3.11 (1.08); acts of NSSI n = 28, with mean frequency of 1.50 (1.15) | Thought of NSSI n = 34, with mean frequency of 3.22 (1.59) and mean intensity of 3.22 (0.81); acts of NSSI n = 14, with mean frequency of 1.44 (1.15) | N/A | N/A | Non-significant group differences showing no risk of iatrogenic effect |
| Decision ads (Rowe et al., 2018), UK (42) | Selective | Rowe et al., 2016 | Young people aged 12 to 18 years at a secondary school in London, England | RCT | Subjective utility analysis was utilized as theoretical foundation (75,76). Annalisa© and Elicia© software was used to create the *Self-Help Tool* in which young people can look at their help-seeking options for self-harm (e.g. family, GP, helplines) | Ten randomized students with at least one episode of 12-month NSSI | Thirteen randomized students with at least one episode of 12-month NSSI General emotional information was given to them with past year NSSI via the ChildLine website (http://www.childline.org.uk/ Explore/FeelngsEmotions/ Pags/FeelingsEmotions.aspx). | Participation was assessed using tools such as the *Self-Harming Behaviors Inventory*, *General Help-Seeking Questionnaire* (74) Questionnaire on anticipated discrimination (77); Discrimination and Stigma Scale (78); Decisional Conflict Scale (79); questions on the DA (web-based personalized decision aid). | Not reported | Not reported | None | A post-intervention survey was completed reporting that all 10 intervention participants followed the DA advice, and described improved help seeking behaviors and would recommend the DA for use by others. One and two did not report any adverse events. | |
| SBISY (Byrum, 2019), Mexico (44) | Universal | N/A | Sixth-grade learners at a single elementary school in Juventino Rosas, Mexico, and as the participants changed the grade, the one-year follow-up was taken place in four pre-defined secondary schools. | Non-randomized pre-test/post-test control group with one-year follow-up | Based on Edelblute (80), including three 90-minute sessions introducing practices based on cognitive behavior therapy and dialectical behavior therapy | 63 sixth grade students (eight dropped out, leaving 55 valid data) from three identified classes, who were followed-up 12-month later in four seventh grade schools | 25 seventh grade schoolers (one dropped out, leaving 24 valid data) who did not partake in the previous year intervention. | Negative stress-relieving (self-harming) behavior questions, including cutting, alcohol and drug use in addition to Stress in Children Scale (81), and non-validated scale of confidence which is unique to this intervention. | Students with cutting in intervention group n = 6 (10.91%), No assessment for controls | N/R | Students with cutting in intervention group n = 12 (21.82%), in controls n = 3 (12.50%) | No Significant changes in stress-relieving behavior | Participants in intervention group reported to self-harm to manage stress at twice the rate of the control group however, results indicated that participants who self-reported self-harm experienced a significant decrease in perceived stress levels post-intervention. |
| HappylesPLUS (Baetens, 2020), Belgium (43) | Universal | N/A | Six secondary schools in Belgium | Mixed-methods, including a pre-test/post-test design and a follow-up quantitative evaluation | Based on Happyles program (49) designed for improvement of mental health + NSSI-specific module, including four 50-minute in-classroom psychoeducational classes introducing preventive curricula incorporating interactive classroom discussions, engaging assignments and supplementary e-health modules | 340 Pupils in HappylesPLUS Group | 311 Pupils in Happyles Group | Youth Outcome Questionnaire (82), The Brief NSSI assessment test (BNSSI-AT, 83), Difficulties in Emotion Regulation Scale (84), The Attitudes Toward Seeking Professional Psychological Help Scale — short form (85) | HappylesPlus:18.1%, Happyles:11.4% P = 0.019 | HappylesPlus:4.7%, Happyles: 7.3% P 0.259 | N/A | No iatrogenic effect was observed | NSSI-specific modules To can be incorporated into evidence-based school prevention programs that, while promoting help seeking behaviors, also lessened engagement in future NSSI after general prevention programs (with or without the NSSI modules) was observed; help-seeking behaviors were promoted. |
General and Methodological Information of Reviewed Articles (Non-suicidal Self-injury-Focused Results)
The HappylesPlus program reported new NSSI incidences, showing no significant difference compared to its parent program (4.7% vs. 7.3%, P = 0.259). Participants with prior NSSI in HappylesPlus had higher, but nonsignificant, engagement days than controls [3.58 (6.52) vs. 2.11 (4.93), P = 0.317]. Both groups reported similar NSSI urges [3.53 (3.40) vs. 3.39 (3.14)]. The perceived likelihood of NSSI increased within both groups (P < 0.001), with no between-group difference (P = 0.458), suggesting global mental health psychoeducation was equally effective on NSSI outcomes.
The DAs study did not formally evaluate NSSI ratings at posttest or follow-up, as participants were active NSSI engagers requiring improved help-seeking decision-making (44, 48). The SOSI study showed high effect sizes for reduced NSSI-related avoidance (ɳ² = 0.15) and discomfort (ɳ² = 0.12), moderate for increased knowledge (ɳ² = 0.064), and low for approach/helping desire (ɳ² = 0.05), with no significant change in help-seeking (ɳ² = 0.005) (41).
The SBISY study noted a stress reduction trend (2.17-point difference, P = 0.35) in participants using self-cutting for stress relief, indicating promising results for the intervention group with higher baseline NSSI (44).
The HappylesPlus program and its parent program showed no significant differences in overall psychological distress or subscales, except for reduced somatic symptoms. However, HappylesPlus participants reported significantly higher conduct problems at posttest (P = 0.028), with a similar trend in the parent program (P = 0.069). Emotional awareness improved significantly in both conditions (P < 0.001), slightly higher in HappylesPlus (P = 0.087). No changes were observed in impulse control difficulties or openness to seeking emotional treatment.
No significant changes were seen in impulse control, treatment openness, or stigma measures in both groups. However, girls improved in stigma agreement, and high pret-est scorers improved in both stigma subscales. The DAs study lacked the power to detect significant changes in decision-related outcomes across all assessment stages (42).
Some studies (41) assessed feasibility and iatrogenic effects. Post-intervention interviews with counselors from five high schools found the SOSI program easy to deliver, well-organized, and user-friendly. Counselors felt prepared, and students engaged well, especially with video materials (41).
The DAs study interviewed 14 students (9 trial participants: Eight intervention, 1 control; 5 without self-harm), 3 school staff, and 5 parents/caregivers. Key facilitators included social support and financial incentives, while barriers included stigma and fear of disclosure. Group dynamics promoting self-disclosure and help-seeking emerged as central. The DA Tool’s ease and speed were praised, but staff suggested improving its language and interactivity. While the intervention group found sessions useful, adherence to DA suggestions was mixed. Most participants appreciated the straightforward survey, recruitment, and follow-up process, though some staff raised concerns about self-harm “contagion” and parental consent challenges (42).
Content analysis of HappylesPlus participants’ experiences six weeks post-implementation revealed cognitive and emotional reactions. Participants valued increased NSSI knowledge, including its distinction from suicidality, consequences, and referral information, and found the documentary trustworthy due to real stories. They appreciated NSSI destigmatization and learning how to help peers, though some felt the information was familiar. Emotionally, some found the module shocking and painful, with one student leaving due to distress. Few participants found the documentary useful for connecting with peers, while others remained unaffected or negative.
No post-intervention measures were reported for the SBISY study (44). No iatrogenic effects were reported in the SOSI study (41), DAs study (42), or HappylesPlus (43). However, the SBISY study noted a doubled NSSI incidence despite a reducing trend among Mexican adolescent participants (44).
5. Discussion
"Self-harm" encompasses intentional self-injury (e.g., cutting) or self-poisoning (e.g., overdoses), regardless of suicidal intent (48). It includes acts with suicidal intent ("attempted suicide"), non-suicidal motives (e.g., distress relief), and mixed motivations (49). However, this categorization is often viewed as artificial (50). Key differences between suicide attempts and NSSI include method lethality, frequency, and attitudes toward life and death (51-53). The DSM-5 distinguishes "Suicidal Behavior Disorder" (SBD) from "Non-Suicidal Self-Injury" (NSSI) to highlight these differences (54).
These findings emphasize the need for early interventions and public health efforts targeting NSSI in school-aged children and adolescents. However, only four studies in this review focused on pure NSSI without suicidal intent. A recent review by Matthews et al. found that 8 out of 16 studies failed to distinguish between suicide and NSSI, underscoring the importance of clearly differentiating NSSI from suicidal behavior in future programs. Consistent with the literature (24), there is no standardized platform for NSSI identification and assessment, resulting in varied risk classification, decision-making on assessors, settings (school/emergency services), and tools. These differences are seen in screening methods, sample selection, and intervention tools, as highlighted in both the literature and this review.
A critical yet overlooked issue in NSSI school-based interventions is context. No studies addressed contextual factors theoretically or practically. Theoretically, schools prioritize academics, potentially resisting psychoeducational programs. Practically, time and space constraints exist. Early collaboration with school administration, students, and teachers is essential for program continuity (55). Integrating programs into the curriculum is crucial, while add-on programs (e.g., after school) are discouraged (55). Prevention programs must align with school perspectives and activities to avoid resistance and wasted resources.
When developing school-based prevention programs, selecting target groups, intervention levels (individual/environmental, involving family, peers, staff), and ensuring participation are crucial. Multilevel interventions are more effective than single-level efforts (55). Programs engaging parents, staff, and youth yield greater impact. This review’s studies focused on youth, with only Muehlenkamp assessing feasibility via counselor interviews. Long-term designs with multiple time points and follow-ups (> 12 months) are essential to sustain benefits. All reviewed studies included follow-ups, supported by research (24, 41, 55).
Prevention efforts must be empirically and theoretically grounded. While the four reviewed studies used elements of CBT, DBT, positive psychology, subjective utility analysis, and coping theory, NSSI-related factors still lack an integrated theoretical framework.
Understanding the potential outcomes of prevention efforts is crucial to avoid harm and improve future programs. A key contribution to NSSI prevention, especially in schools and among adolescents, would be investigating whether and why iatrogenic effects occur. One harmful approach is using explicit materials targeting at-risk individuals, such as graphic images, personal narratives, or videos, which may act as triggers and increase NSSI incidence (56).
Help-seeking is a critical issue in schools and NSSI prevention. There is a decline in young individuals seeking help from family members (24). School mental health professionals are often the first adults whom adolescents turn to, but inadequate training and lack of institutional support leave them feeling unprepared. Prevention programs must prioritize building teams, providing training, and developing policies to empower these professionals (57). Addressing stigma, confidentiality, and offering precise support to all students, especially peers of those who self-harm, is essential (24). Muehlenkamp demonstrated that teaching students how to seek help effectively encourages help-seeking behavior.
A critical yet often overlooked aspect of school-based interventions is the role of cultural factors. While there is some consistency in NSSI prevalence, methods, and associated thoughts, variations exist in functions, gender patterns, and methods across countries (58, 59). For example, in Pakistan, ingesting toxic substances like pesticides is common, especially among females (60). Studies in Hong Kong (61), Indonesia (62), and India (63) highlight interpersonal triggers as significant antecedents for NSSI. Additionally, NSSI prevalence varies among minority groups, including ethnic and sexual/gender minorities. Interventions must adapt to these cultural, contextual, and community differences to be effective.
Data on NSSI interventions is limited compared to suicidal behaviors. The eHealth methods, like mobile apps, are promising, with over five billion mobile subscriptions globally (64). Youth see apps as useful for self-management and crisis prevention (65). Digital tools, as shown in the DAs study (42, 46), can overcome structural barriers in current interventions.
Social contagion is a major NSSI concern, with friends' self-injury linked to adolescents' own NSSI. Girls, more likely to discuss NSSI and exhibit higher rates of such behaviors, are disproportionately affected by contagion (66). School-based programs should address gender differences, though only HappylesPlus explicitly studied these effects (43).
Parental characteristics, such as perceived control and lack of care, can increase NSSI risk among youth (67, 68). Currently, parental involvement in schools regarding NSSI is often limited to post-incident notifications (69). Parent training, a key driver of behavior change (69), could be a vital component of NSSI prevention programs, especially in schools. However, only one study has included parents in such interventions (70). It is suggested that adaptable cultural interventions be explored among families in different societies regarding their involvement with self-harm issues.
This systematic review identified four school-based NSSI prevention interventions, which were limited in quality, design, and effectiveness. However, promising findings emerged regarding iatrogenic effects, feasibility, and secondary outcomes. Future efforts should adopt a multidimensional approach, incorporating eHealth tools, parental involvement, cultural diversity, and NSSI-specific theoretical frameworks to address NSSI and its related factors effectively. Furthermore, we suggest standardization in future works to avoid inconsistencies due to complications in cross-study comparison.