1. Background
Nowadays, in Iran, we are witnessing fundamental changes and transformations in the main structures of society, such as the economic, social, cultural, and political structures. These changes include improvements in public health, increased literacy levels, and their impact on society, particularly the status of women in these indicators, changes in family structures and lifestyle patterns, and the trend toward urbanization and modernization. Among the widespread changes that exist in societies, the most significant one that has had a significant impact and multiplied its importance has been the downward trend and continuous decline in the fertility rate in the population. For example, this indicator decreased from 7 in 1980 to about 6.3 in 1986, and the total fertility rate was estimated at 1.8 and 1.6 for the years 2006 and 2011, respectively (1). A decrease in the fertility rate in a society means a change in the population structure. This point will increase the proportion of elderly people in the population over time. Since the elderly need more medical services and healthcare, this will lead to a greater demand for specialized services. Therefore, a decrease in the fertility rate along with an increase in life expectancy directly affects the consumption of medical services by the elderly, which creates a serious challenge in various areas. Declining fertility coupled with increasing life expectancy has led to an increase in the proportion of older people in the population, which is a sign of population aging. These societies emerge when low fertility is accompanied by increasing life expectancy, ultimately changing the structure of the population and creating new fundamental challenges for social and care systems (2-4). The nature of old age necessitates special needs due to the decline in physical abilities, and healthcare and treatment services are among the most essential needs of this group. This has made the elderly the primary consumers of healthcare services. On the other hand, most of the treatment needs of the elderly involve expensive services (5-9)
Therefore, the elderly population and the aging population structure in societies represent not just a change in population structure, but also a fundamental social, health, and economic challenge. As the elderly population increases, the likelihood of households with elderly members facing catastrophic healthcare expenditures also rises. Furthermore, healthcare services consume a large and growing portion of the income of countries. Currently, healthcare services consume, on average, up to one-tenth of the GDP of wealthy countries (5, 6, 8, 10). One of the most critical aspects to be considered in the health sector is the cost of elderly care, which can include outpatient treatments, hospitalization, medications, diagnostic tests, and home care or nursing home care. Financial, physical, and human resources planning and policy-making are fundamental principles in healthcare management, which should also be considered in the context of aging, taking into account demographic, epidemiological changes, and technological developments (6, 11-14).
All of the demographic and economic indicators mentioned above highlight the urgent need for appropriate preventive planning as a vital issue. The emergence of the aging population phenomenon in the future and the increase in healthcare costs serve as a warning for policymakers and health system managers in the country. It is crucial that before the population ages further, appropriate policies and solutions are adopted based on existing strategies, and attention is paid to the impact of current policies. Currently, one of the main and most important policies implemented in Iran is the health transformation plan (HTP), a plan that was planned and implemented in 2014 with the aim of fundamental reforms to increase equity in access to healthcare, improve the quality of services, and reduce out-of-pocket payments. Given the increasing needs of the elderly population in using healthcare and the financial vulnerability of the elderly population, it is of great importance to evaluate and examine the effects of this plan on services that are commonly used by the elderly. Since there has been no separate financial policy for the healthcare of the elderly so far, we will examine the impact of one of the major healthcare projects, the HTP, on the most common services used by the elderly (15-20).
2. Objectives
The aim of this study was to evaluate changes in healthcare utilization trends among elderly patients in five major disease groups in Tabriz before and after the implementation of the HTP. The outcome variables included the number of healthcare visits, service costs, and frequency of service use during the five years before and five years after the plan's implementation. Additionally, we sought to understand the broader implications of these changes on elderly patients' access to related healthcare services. Using a discontinuous time series approach, this study focused on examining the effects of the HTP implementation and its impact on the health system, with particular emphasis on service use among the elderly in Tabriz.
3. Methods
This study is a longitudinal and quasi-experimental (quasi-experiment) study conducted using data from 2009 to 2018. To evaluate the policies and programs implemented by the health system, a time-series method is used to assess the effectiveness of large-scale health and treatment interventions. The time-series method shows the changes of a phenomenon over time. Additionally, time-series analysis, using data from past events of a phenomenon, predicts that phenomenon in the future. The changes of the phenomenon under study in the time-series model can be examined in a continuous manner (Continuous time-series method) or for discrete times (Interrupted time-series method).
The data used in this study consisted of administrative records of all visits by elderly patients in Tabriz, obtained from the Ministry of Health’s Health Information System (HIS). This dataset includes records from all public healthcare centers across Tabriz; private centers were not included. Data were collected monthly through mandatory reporting to the HIS. Therefore, no sampling was performed, and the data represent a census of service utilization.
The following regression model was used in the analysis:
Here, Yt represents the number of admissions in month t. Tt is the time trend variable, which ranges from 1 (first observation) to 40 (last observation). Xt is a binary variable indicating the status of visits before and after the policy implementation Xt = 0 for before the policy and Xt = 1 for after the policy). Xt Tt is coded as 0 for the period before the policy implementation and assigned a value of 1 for the period after the policy implementation.
β0 represents the starting level (intercept) of the outcome variable. β1 represents the slope of the outcome variable before the policy implementation, indicating the pre-existing trend. β2 represents the change in the outcome variable immediately after the policy implementation (compared to the counterfactual). β3 is the variable that represents the difference between the slope before and after the policy implementation.
The inclusion of Tt (time trend), Xt (intervention), and the interaction term Xt Tt allows the model to estimate both the immediate effect of the intervention and changes in trends over time. This specification helps distinguish the impact of the HTP from underlying time trends. Since there are different methods to examine the effect of a variable over time, in this study, we used the interrupted time series (ITS) method to evaluate the impact of the HTP on the use of health services among the elderly in Tabriz. The ITS is appropriate for assessing interventions implemented at a specific time point, allowing estimation of immediate and trend effects.
For this study, we used ten years of data, including two five-year periods: Five years before the intervention, from 2009 to 2013, and five years after the intervention, from 2014 to 2018, to examine the impact of financing policies. The dependent variable in our study was the number of visits to centers for the elderly in the disease groups identified in the study. Disease groups were classified according to ICD-10 codes, focusing on the primary diagnosis recorded at each visit. The data were obtained from monthly reports submitted by health centers to the Ministry of Health’s HIS in Tabriz. These included administrative records of outpatient visits and healthcare costs, categorized by disease group.
Before analysis, the dataset was examined for missing values and outliers. Records with missing values for key variables (e.g., date, diagnosis group, or number of visits) were excluded after confirming their exclusion would not introduce systematic bias. Outliers were identified using the interquartile range (IQR) method and assessed for validity; implausible values were removed from the dataset, while extreme but plausible values were retained. We also used a model to examine the impact of policies on the use of the most common services. The conditions of this model were as follows: A regression model with a time trend variable and an intervention variable was used. The time variable indicates the normal use of services over time, and the intervention variable indicates the time of intervention. In our study, the intervention variable began at the beginning of 2014.
The analysis also included seasonal adjustments to account for seasonal fluctuations in healthcare utilization. We used the Durbin-Watson test to examine the autocorrelation of the data. Given the importance of the issue of normality of the residuals, we also used the Shapiro-Wilk test. We also used the Levene test to examine the stationarity of variances, which is necessary and essential for examining the models. Data analysis was performed using SPSS version 16.
4. Results
After analyzing the obtained data based on disease group classifications, the results are presented in Table 1, which shows the distribution of visit loads across different groups over the ten-year period. As seen in Table 1, the top five disease groups account for 62% of the total visit load during the study period.
| ICD Code Group | Disease Category Description | Total Number of Visits (Service Usage) |
|---|---|---|
| I | Diseases of the circulatory system | 162,749 |
| N | Diseases of the genitourinary system | 92,848 |
| S | Injuries, poisonings, and other external causes | 78,192 |
| Z | Factors affecting health status and utilization of health services | 74,685 |
| M | Diseases of the musculoskeletal system and connective tissue | 56,752 |
| K | Diseases of the digestive system | 47,286 |
| R | Symptoms and abnormal clinical findings, not elsewhere classified | 43,981 |
| T | Injuries, burns, and drug poisoning | 33,084 |
| E | Endocrine, nutritional, and metabolic diseases | 32,766 |
| C | Neoplasms | 29,928 |
| J | Diseases of the respiratory system | 24,658 |
| G | Diseases of the nervous system | 19,466 |
| D | Diseases of the blood and blood-forming organs, and immune system disorders | 17,977 |
| A-B | Certain infectious and parasitic diseases | 15,439 |
| L | Diseases of the skin and subcutaneous tissue | 7,014 |
| W | External causes of injury, non-intentional | 4,165 |
| F | Mental and behavioral disorders | 2,002 |
| V | Vehicle accidents | 1,681 |
| Y | External causes of disease and mortality | 1,371 |
| H | Diseases of the eye and adnexa | 1,332 |
| Q | Congenital anomalies, deformations, and chromosomal abnormalities | 939 |
| X | X | 185 |
| O | Pregnancy, childbirth, and the puerperium | 115 |
| P | Newborn conditions originating in the prenatal period | 44 |
| U | SARS | 23 |
Grouping of Disease Categories and the Corresponding Burden of Healthcare Visits
Table 2 displays the visit load across all groups during the study years, as well as the percentage increase in visit load compared to the previous year and in relation to the intervention (the implementation of the HTP).
| Intervention | Period of Intervention (Before) | Period of Intervention (After) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year of service usage | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
| Total Number of services used (y) | 52,808 | 53,760 | 64,125 | 68,068 | 70,648 | 83,130 | 93,164 | 84,320 | 96,759 | 81,900 |
| Annual percentage change in service usage (%) | 1.80 | 19.28 | 6.15 | 3.79 | 17.67 | 12.07 | (9.49) | 14.75 | (15.36) | |
| Total (before and after intervention) | 309,409 | 439,273 | ||||||||
| Percentage change; before vs after (%) | - | 42 | ||||||||
Annual Service Usage Statistics Before and After the Intervention (2009 - 2018), Including Yearly Changes and Overall Impact
By examining the ten-year data collected for disease groups, it was found that five groups of diseases had the highest costs, accounting for 62 percent of the total costs. Among these groups, the circulatory system diseases group had the highest costs on the health system in Tabriz, followed by injuries, poisonings, and other external factors, and the musculoskeletal and connective tissue disorders group. These findings also showed that there is a need to prioritize diseases in order to better manage healthcare resources, given the increase in costs in the health sector, and to examine their consumption trends in terms of the impact of different policies. By examining the average costs of disease groups over the ten years, it was found that the infectious and parasitic diseases group had the highest average costs.
Finally, by examining the burden of visits and the total cost of disease groups, we selected five groups of diseases for further study, which included diseases of the circulatory system, diseases of the genitourinary system, injuries and poisonings, other external causes, factors affecting health status and use of health services, and diseases of the musculoskeletal system and connective tissue. These data are presented based on the interrupted time series method from the 21st period (Appendix 1 in Supplementary File) related to the start of the implementation of the HTP. As shown in Table 3, the percentage change in the burden of visits before and after the intervention can be seen, with disease group Z showing the highest percentage change.
| Groups | Disease Group Description | Number of Consultations Before Intervention | Number of Consultations After Intervention | Total Number of Consultations | Percentage Change in Consultation Burden |
|---|---|---|---|---|---|
| I | Diseases of the circulatory system | 76,221 | 86,528 | 162,749 | 13.52 |
| M | Diseases of the musculoskeletal system and connective tissue | 22,938 | 33,814 | 56,752 | 47.41 |
| N | Diseases of the genitourinary system | 42,770 | 50,078 | 92,848 | 17.09 |
| S | Injuries, poisonings, and other external causes | 35,603 | 42,589 | 78,192 | 19.62 |
| Z | Factors affecting health status and utilization of health services | 13,843 | 60,842 | 74,685 | 339.51 |
Consultation Burden Before and After Intervention Across Different Disease Groups
To assess the normality of the data, five groups were tested using the Shapiro-Wilk test. As shown in Table 4 (P > 0.05), all the data follow a normal distribution. Therefore, we employed a linear regression model to evaluate the effect of the intervention on the patients' visit trends. No sensitivity analysis was performed in our study, which should be considered a limitation of the study, and we recommend that future research use it to better evaluate and verify the reliability of the results.
| Tests of Normality | Levene (P-Value) | Shapiro-Wilk Statistic | Degrees of Freedom (df) | P-Value |
|---|---|---|---|---|
| Disease Group | ||||
| Diseases of the circulatory system | 0.788 | |||
| Spring | 0.942 | 10 | 0.572 | |
| Summer | 0.888 | 10 | 0.161 | |
| Autumn | 0.873 | 10 | 0.107 | |
| Winter | 0.953 | 10 | 0.706 | |
| Diseases of the musculoskeletal system and connective tissue | 0.337 | |||
| Spring | 0.972 | 10 | 0.906 | |
| Summer | 0.989 | 10 | 0.996 | |
| Autumn | 0.935 | 10 | 0.5 | |
| Winter | 0.907 | 10 | 0.259 | |
| Diseases of the genitourinary system | 0.264 | |||
| Spring | 0.922 | 10 | 0.374 | |
| Summer | 0.941 | 10 | 0.563 | |
| Autumn | 0.917 | 10 | 0.337 | |
| Winter | 0.986 | 10 | 0.988 | |
| Injuries and poisonings and other external consequences | 0.391 | |||
| Spring | 0.939 | 10 | 0.541 | |
| Summer | 0.864 | 10 | 0.084 | |
| Autumn | 0.913 | 10 | 0.3 | |
| Winter | 0.917 | 10 | 0.332 | |
| Factors affecting health status and use From health services | 0.000 | |||
| Spring | 0.862 | 10 | 0.08 | |
| Summer | 0.863 | 10 | 0.083 | |
| Autumn | 0.871 | 10 | 0.102 | |
| Winter | 0.858 | 10 | 0.073 |
Shapiro-Wilk Normality Test Results for Disease Categories by Season
According to Levene's test, only in the group of "factors affecting health status and use of health services", heterogeneity of variance was observed between the two periods before and after the intervention (P < 0.000). This indicates that the variability of the data in this group varied significantly depending on the intervention, and the stationarity of variance was not established.
4.1. Diseases of the Circulatory System
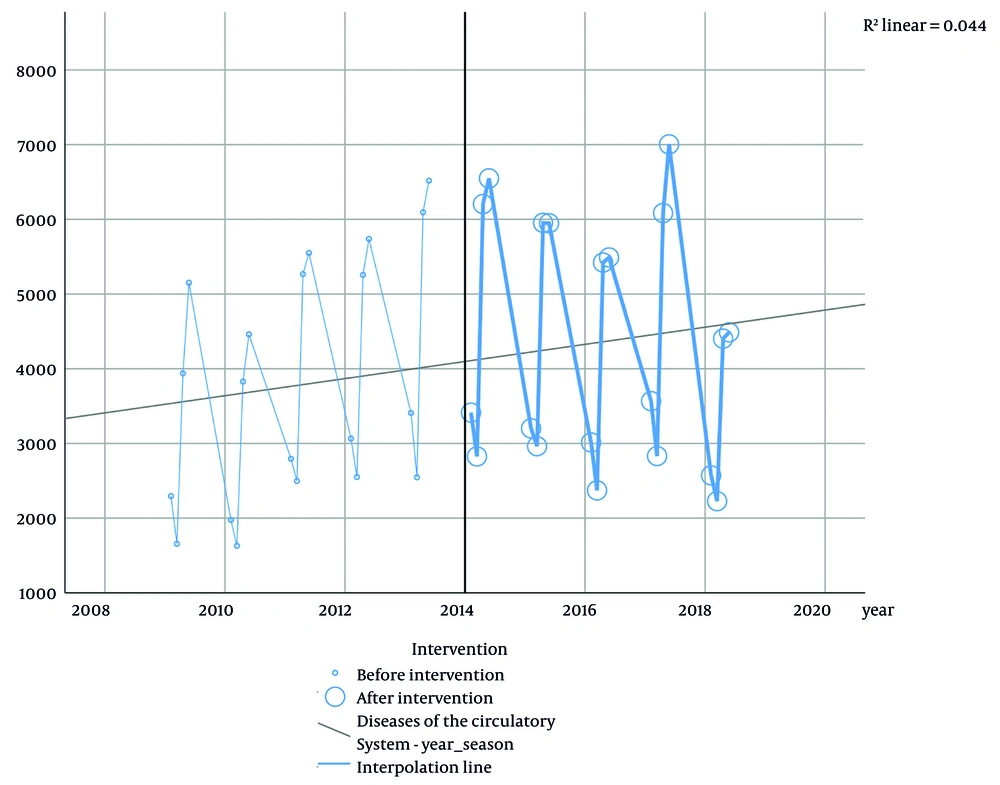
The fixed effect in this disease group was statistically significant (β0 = 2380.121, P = 0.002), indicating that before the intervention, the burden of visits among the elderly in Tabriz had been increasing significantly. Additionally, the effect of time on the burden of visits was found to be significant (P = 0.027), with each unit increase in time leading to a rise of 136 visits. Regarding the effect of the intervention, the obtained coefficient indicated an increase in the burden of visits after the intervention; however, this increase was not statistically significant (P = 0.24). Furthermore, the interaction effect between time and intervention suggested that the increasing trend of the burden of visits had slowed down. However, this change did not reach statistical significance at the 0.05 level (P = 0.082) (Table 5). Figure 1 shows the course of the disease over 10 years before and after the intervention.
| Groups | Estimated Coefficients | Std. Error (Newey-West) | P-Value | 95% Confidence Interval (Lower) | 95% Confidence Interval (Upper) |
|---|---|---|---|---|---|
| I | |||||
| (Constant) β0 | 2380.121 | 708.044 | 0.002 | 944.141 | 3816.101 |
| Time β1 | 136.279 | 59.106 | 0.027 | 16.406 | 256.152 |
| Intervention β2 | 2347.182 | 1966.564 | 0.240 | -1641.195 | 6335.559 |
| Time intervention β3 | -149.423 | 83.589 | 0.082 | -318.950 | 20.103 |
| M | |||||
| (Constant) β0 | 1533.995 | 272.951 | 0.000 | 980.423 | 2087.566 |
| Time β1 | -36.866 | 22.786 | 0.114 | -83.077 | 9.345 |
| Intervention β2 | -446.782 | 758.112 | 0.559 | -1984.304 | 1090.740 |
| Time intervention β3 | 56.653 | 32.224 | 0.087 | -8.700 | 122.005 |
| N | |||||
| (Constant) β0 | 1712.563 | 392.781 | 0.000 | 915.967 | 2509.159 |
| Time β1 | 40.565 | 32.789 | 0.224 | -25.933 | 107.064 |
| Intervention β2 | 595.953 | 1090.933 | 0.588 | -1616.561 | 2808.467 |
| Time intervention β3 | -34.159 | 46.370 | 0.466 | -128.203 | 59.884 |
| S | |||||
| (Constant) β0 | 1434.668 | 343.608 | 0.000 | 737.799 | 2131.538 |
| Time β1 | 32.903 | 28.684 | 0.259 | -25.271 | 91.077 |
| Intervention β2 | -562.300 | 954.358 | 0.559 | -2497.828 | 1373.228 |
| Time intervention β3 | 8.313 | 40.565 | 0.839 | -73.957 | 90.583 |
| Z | |||||
| (Constant) β0 | 727.037 | 353.786 | 0.047 | 9.526 | 1444.547 |
| Time β1 | -3.323 | 29.533 | 0.911 | -63.219 | 56.574 |
| Intervention β2 | -2633.000 | 982.625 | 0.011 | -4625.857 | -640.143 |
| Time intervention β3 | 165.554 | 41.767 | 0.000 | 80.848 | 250.261 |
Estimated Coefficients and Statistical Parameters of the Segmented Regression Model by Group
In examining the fit of the models, we evaluated and calculated the desired criteria. These criteria showed that our models had an acceptable fit for the five disease groups. Also, in examining the random distribution of the residuals, the results for the disease groups showed that they were randomly distributed. Furthermore, regarding the correlation, no clear correlation was observed, which indicated that the model had the necessary adequacy.
4.2. Diseases of the Musculoskeletal System and Connective Tissue
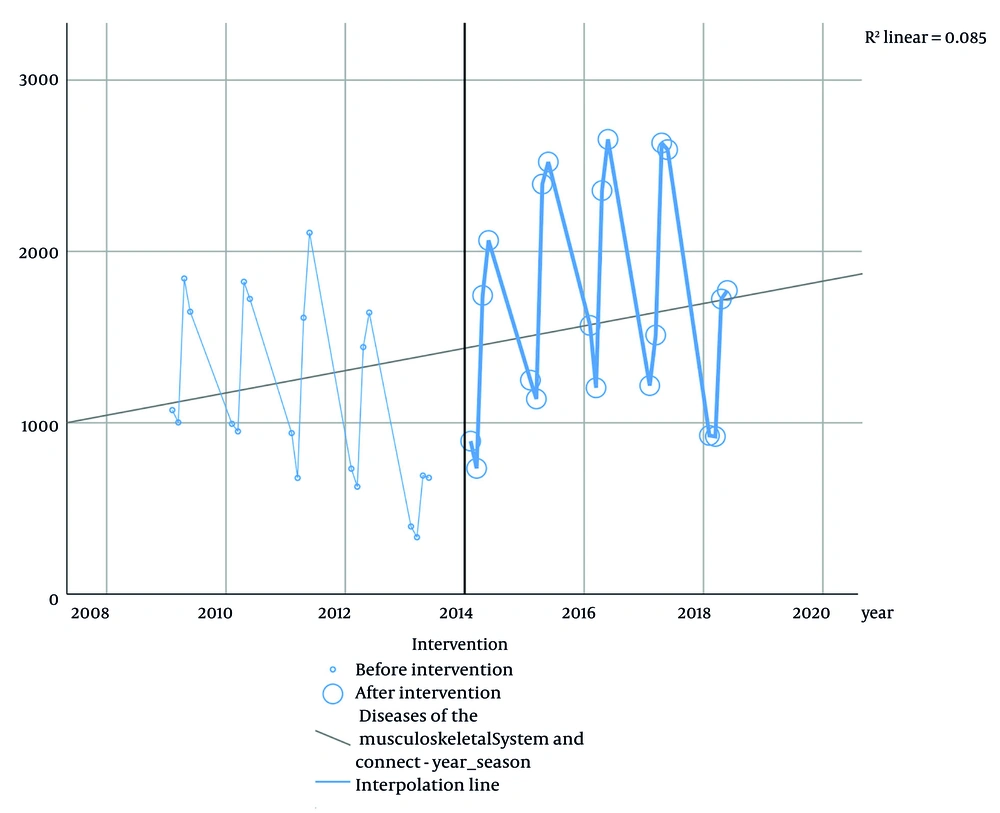
In the second group of diseases, the fixed effect is also significant [β0 = 1533.995, P = 0.000 (P < 0.05)], and it can be concluded that the burden of visits in the disease group increased before the intervention, and the increase in the trend of elderly visits was significant. Regarding the effect of time on the burden of visits, visits decreased, but this decrease was not statistically significant (P = 0.114), and for each unit of increase in time, the burden of visits decreased by -36 units. In examining the effect of the intervention, the coefficient obtained indicated a decrease in the burden of visits after the intervention, but this decrease in visits was also not statistically significant (P = 0.559). In examining the interaction effect between time and intervention, the interaction coefficient obtained for the increasing trend of the burden of visits for this disease group was equal to 56, and in terms of the P-value coefficient, which was equal to 0.087, it showed that this change was also not statistically significant (Table 5). Figure 2 shows the disease trend of Diseases of the Musculoskeletal System and Connective Tissue over the years studied.
4.3. Diseases of the Genitourinary System
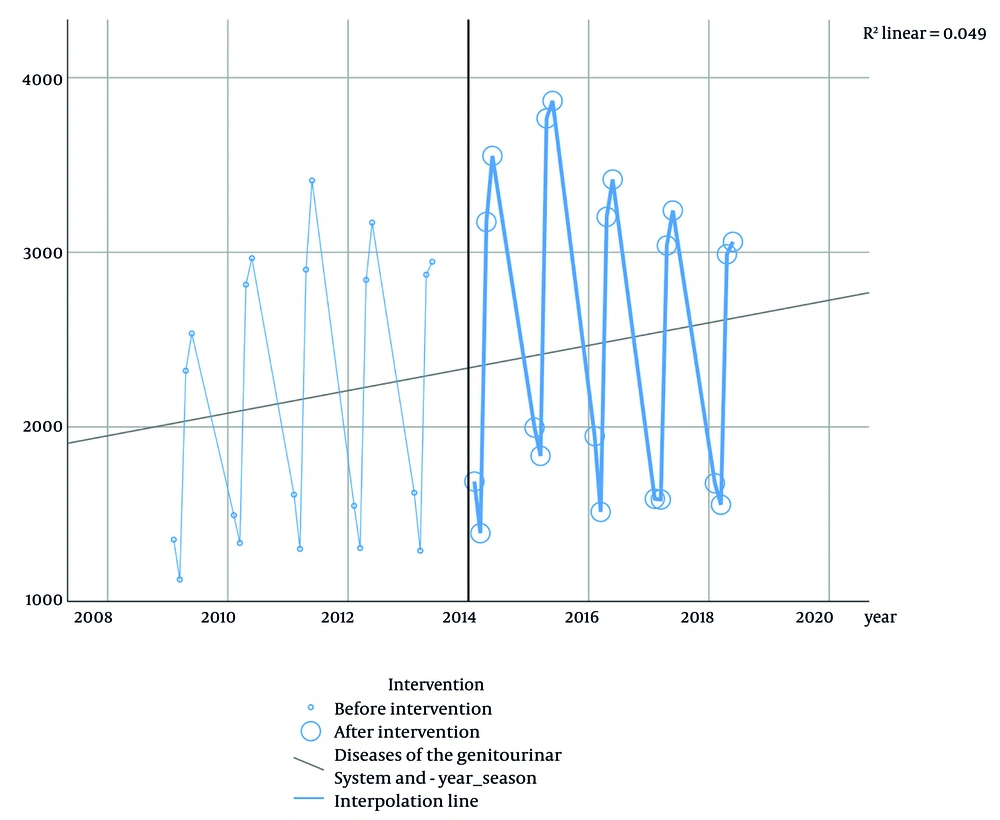
The third group of diseases had a fixed effect coefficient of 1712.563 [β0 = 1712.563, P = 0.000 (P < 0.05)], which is statistically significant. As a result, it can be said that the burden of visits in the disease group increased before the intervention, and the increase in the trend of elderly visits was significant. Regarding the effect of time on the burden of visits, visits increased, but this increase was not statistically significant (P = 0.224), and for each unit of increase in time, the burden of visits increased by 40 units. In examining the effect of the intervention, the coefficient obtained indicated an increase in the burden of visits after the intervention, but this increase in visits was also not statistically significant (P = 0.588). In examining the interaction between time and intervention, the obtained interaction coefficient showed a decreasing trend in the burden of visits for this disease group equal to -34, and in terms of the P-value coefficient, which was equal to 0.466, it showed that this change was also not statistically significant (Table 5). In the third study group, the disease trend is shown with a constant trend as depicted in Figure 3.
4.4. Injuries and Poisonings and Other External Causes
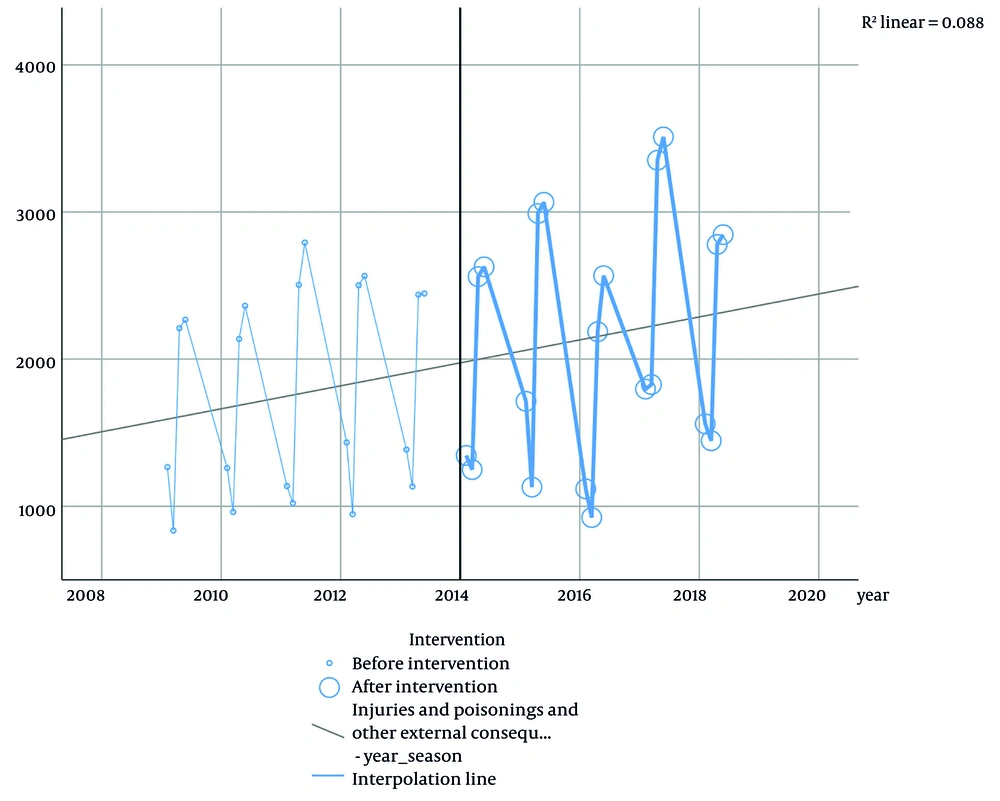
In the group of diseases of injuries and poisonings and other external causes, the fixed effect coefficient was 1434.668 [β0 = 1434.668, P = 0.000 (P < 0.05)]. The fixed effect in this group is statistically significant, and as a result, it can be said that the burden of visits in this disease group increased before the intervention, and the increase in the trend of elderly visits was also significant. Regarding the effect of time on the burden of visits, visits increased, but this increase was not statistically significant (P = 0.259), and for each unit of increase in time, the burden of visits increased by 33 units. In examining the effect of the intervention, the coefficient obtained indicated a decrease in the burden of visits after the intervention, but this decrease in visits was also not statistically significant, indicating no change due to the intervention (P = 0.588). In examining the interaction effect between time and intervention, the obtained interaction coefficient showed a slight increase in the burden of referrals after the intervention β3 = 8.313), and in terms of the P-value coefficient, which was equal to 0.839, it showed that this change was also not statistically significant (Table 5). Figure 4 shows the trend of injuries and poisonings and other external causes during the 10 years before and after the intervention.
4.5. Factors Affecting Health Status and Use of Health Services
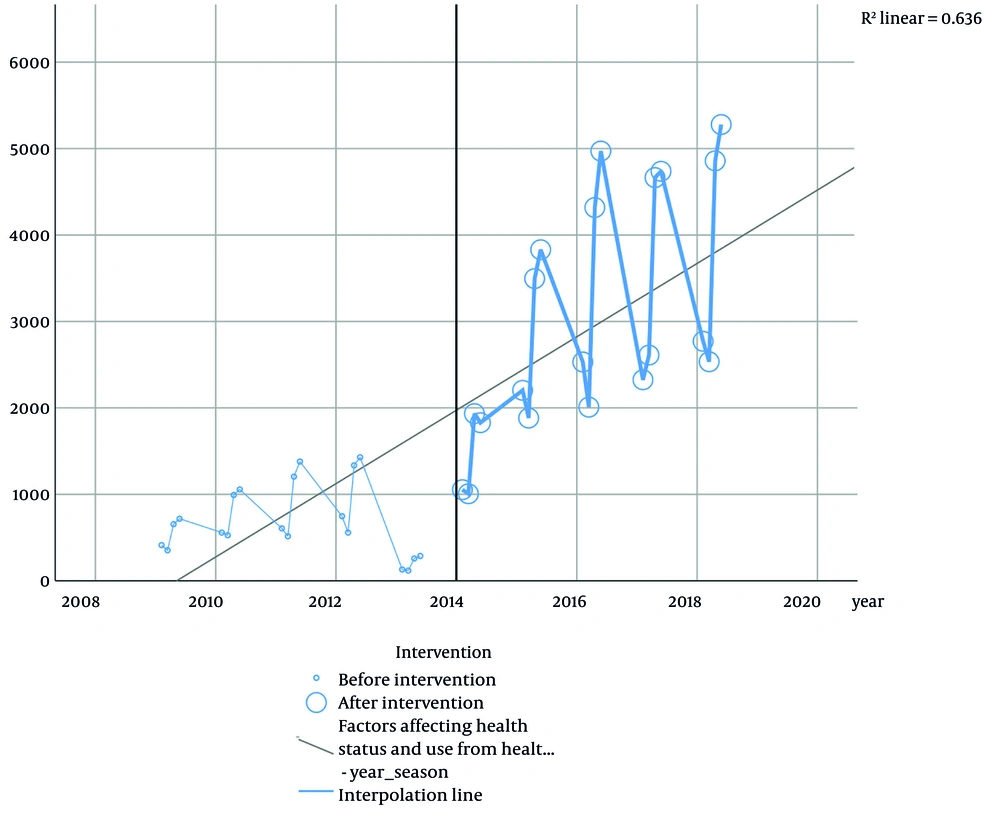
In the last group of diseases studied in this study, the fixed effect coefficient was 727.037 [β0 = 727.037, P = 0.047 (P < 0.05)]. The fixed effect in this group is statistically significant, and as a result, it can be said that the burden of visits in this disease group increased before the intervention, and the increase in the trend of elderly visits was also significant. Regarding the effect of time on the burden of visits, the trend of visits faced a slight decrease, and this decrease was not statistically significant (P = 0.911). In examining the effect of the intervention, the coefficient obtained also indicated a decrease in the burden of visits after the intervention. This decrease in visits was statistically significant (P = 0.011), which indicates a decrease in the burden of visits due to the intervention. The interaction between time and intervention showed a trend of increase in the number of visits after the intervention (β3 = 165.554), and the P-value coefficient, which was equal to 0.000, showed that this change was statistically significant and had an effect on the number of visits (Table 5). In the last group of diseases studied, the disease trend is also visible with a steep slope in Figure 5.
5. Discussion
This study aimed to evaluate the impact of health financing policies under the HTP on the burden of elderly visits to hospitals in Tabriz, affiliated with Tabriz University of Medical Sciences. As observed in the results, there has been an increasing trend in the visit burden since the beginning of the study period, and with the implementation of the HTP, the rate of increase has slightly risen both overall and specifically. In the initial phase of the plan's implementation, there was an average increase of 17.67% across all groups, which reduced to a 12.07% increase in the following year compared to the previous year. In the third year, the trend showed a decline, with a 9.49% decrease compared to the previous year, yet still showing a 19% increase compared to the pre-intervention year.
During the study, it was found that the financing policies of the HTP at the beginning of its implementation increased the burden of referrals for the elderly in Tabriz among five disease groups. The prediction line of referrals was also observed with a constant increasing trend in the data, but over time, the number of referrals stabilized after the implementation of the HTP, and in some periods, a decrease was also observed compared to the same period of the previous year. Changes in referrals were largely limited in the early stages and were not consistent over time. Even in statistical analysis, the changes were not significant for most disease groups.
The HTP sought to support patients with the policies that were considered, and in the main text of those policies included reducing out-of-pocket payments for patients, supporting the persistence of doctors in deprived areas, ensuring the presence of specialist doctors in hospitals, improving the quality of outpatient services, improving hospital accommodation standards, implementing financial support programs for severe and special patients, and promoting natural childbirth. Among these policies, programs related to reducing out-of-pocket payments for people, insurance coverage, and financial support programs were considered as interventions effective in financing.
Over the years, a study of the percentage of out-of-pocket payments by hospitalized patients in 2013 and 2014 showed that in 2013, the average out-of-pocket payment was 15.2 percent of total hospitalization costs, but this figure decreased to 4.7 percent in 2014, which was an indication of the goal of the HTP (21, 22). Since the goal of the HTP was specified in the programs, by examining the average percentage of basic insurance payments in those years, it can be concluded that the implementation of this plan was very successful in the first year, as this average increased from 80.6 percent in 2013 to 86 percent in 2014, indicating that supporting patients was in line with reducing out-of-pocket payments (21).
Despite these promising early outcomes, our findings show that the effect of the HTP on elderly visits was inconsistent. One of the main reasons may lie in the fact that the HTP was a broad, system-wide reform and not explicitly focused on the aging population. While elderly patients benefited from general cost reductions and improved service coverage, the program lacked tailored components specifically addressing geriatric needs. Notably, Iran has developed a national document on aging to guide such policies, but as of this study, its implementation remains limited and fragmented.
Many studies have reached results during their review that reflect the current situation. In a study conducted by Gharibi et al. between the years before the implementation of the HTP in 2011 and 2013, the percentage of out-of-pocket payments was 55 and 59.7 percent, respectively (23, 24), while in other studies, including the study by Amery et al. and Kavosi et al., the out-of-pocket costs in these years were estimated to be 8.3 and 14.2 percent, respectively (25, 26). In another study conducted by Hajizadeh and Nghiem, out-of-pocket payments of over 50 percent in Iran were considered one of the important barriers to access to services (27). Furthermore, a study by Leive and Xu in 15 African countries found that these countries have very weak financial systems to protect families from medical costs (28).
In another study conducted in hospitals under the auspices of Shahid Beheshti University of Medical Sciences in Tehran, during the examination of out-of-pocket payments for hospitalized patients, it was found that the average out-of-pocket payment for patients in these hospitals at the beginning of the HTP was 10.2 percent, and out-of-pocket payments for health and medical services increased to more than 58 percent (1). This figure for hospitalization in government hospitals before the implementation of the HTP was about 37 percent. With the implementation of the HTP, out-of-pocket payments for hospitalized services in these hospitals decreased to below 10 percent (1, 22).
Previous studies have shown that hospitalization increases out-of-pocket payments, leading to catastrophic costs (29). Therefore, one of the primary objectives of the HTP was to reduce direct out-of-pocket payments for hospitalization services and, as a result, lower the risk of catastrophic costs. According to the Health Research Institute's report, although catastrophic costs have decreased by 4.5% among rural households and by 1.8% among urban households after the plan's implementation, the incidence of catastrophic costs still stands at 4.8% (30, 31).
As the results of our study showed, the findings from the Levene test indicated that among the five disease groups, only in the group of "factors affecting health status and use of health services" was the variance of the data during the two different periods different. In fact, this difference in variance may depend on several factors, from access to services to changes in health policies, or the behavior of the clients.
5.1. Diseases of the Circulatory System
According to the study of the burden of visits, the effect of time in this disease group was incremental, and with the implementation of the HTP, the burden of visits initially increased, but this increase was not statistically significant. Although the interaction between time and intervention had a negative effect, this effect was also not statistically significant. In this analysis, it can be found that the process of time has played a major role in changes in the burden of visits. Therefore, a more accurate assessment is needed to consider the effects of other external factors, including the state of public health, crises, and economic conditions.
5.2. Diseases of the Musculoskeletal System and Connective Tissue
The lack of a significant effect may suggest that musculoskeletal conditions were not sufficiently targeted by the HTP benefit packages, or that patients with these conditions face non-financial barriers such as cultural norms, limited access to physiotherapy, or low awareness. These patterns, although statistically insignificant, can have policy relevance, especially considering the rising burden of disability in the elderly population. On the other hand, the observed changes were also more influenced by the time factor than the intervention implemented, which could also be due to changes in other factors, such as population growth, seasonal changes, or other variables. Therefore, it is necessary to explore other potential causes for the insignificant effect of the HTP on referral burden. These may include limited inclusion of musculoskeletal/genitourinary services in the HTP benefit package, lower perceived urgency among patients, or continued financial and geographic access barriers specific to these conditions. Future research should investigate whether these disease groups have unique service utilization patterns or unmet needs that were not adequately addressed by HTP interventions.
5.3. Diseases of the Genitourinary System
Similar to musculoskeletal conditions, the absence of a statistically significant effect in genitourinary diseases does not necessarily mean a lack of impact. It is possible that these services were underrepresented in the HTP benefit package, or that social stigma, limited diagnostic access, or gender-specific barriers prevented patients from seeking care. These patterns highlight the importance of reviewing whether the design of the HTP was sufficiently inclusive of elderly patients with urological or kidney-related conditions. Despite statistical insignificance, the real-world implications warrant further investigation. On the other hand, the observed changes were also more influenced by the time factor than the intervention implemented, which could also be due to changes in other factors, such as population growth, seasonal changes, or other variables. Therefore, it is necessary to explore other potential causes for the insignificant effect of the HTP on referral burden. These may include limited inclusion of musculoskeletal/genitourinary services in the HTP benefit package, lower perceived urgency among patients, or continued financial and geographic access barriers specific to these conditions. Future research should investigate whether these disease groups have unique service utilization patterns or unmet needs that were not adequately addressed by HTP interventions.
5.4. Injuries and Poisonings and Other External Consequences
Regarding the fourth disease group, the P-value for the time coefficient and the interactive effect of both factors showed that the changes in the burden of visits were not significant, and these factors could not have significantly affected the changes in the burden of visits to centers to receive services for this group. While the intervention itself did not significantly impact the burden of visits for injuries and poisonings, the high baseline level of referrals suggests a persistent demand for acute and emergency care. This implies that trauma-related conditions may fall outside the financial reach or structural scope of the HTP. The practical implication is that resource allocation for emergency departments and trauma care services needs to be maintained or strengthened, particularly in urban settings where these incidents are more frequent.
5.5. Factors Affecting Health Status and Use of Health Services
For this group of diseases, the P-value for the intervention coefficient and the interaction effect of both factors showed that the changes in the referral burden were significant and that these factors caused the changes in the referral burden, and the observed changes also reflect the effect of these two factors. With the implementation of the HTP, the referral burden decreased, but over time, the referral burden increased, and the referral trend returned to the increasing state before the intervention.
5.6. Conclusions
To improve outcomes and improve the current situation, it is necessary to review the effects of implemented policies so that, in the event of new policymaking, policies can be formulated that identify strengths and weaknesses, opportunities, and threats and that take into account and apply efficiency and effectiveness in allocating resources. Therefore, in order to design interventions more effectively, it is essential to review implemented policies.
In a study that examined the impact of the HTP on the burden of referrals among the elderly in different disease groups, the findings indicated that the impact of this plan on the burden of referrals to medical centers among the elderly group was insignificant, and in only one group out of five disease groups were these changes statistically significant. Even in this group, despite the increase in referral burden in the initial stages of implementation, these changes were not sustainable over the following years. Furthermore, since the HTP did not specifically target a particular group and was implemented as a general plan in the country, considering various aspects from the presence of resident doctors to financing aspects, this may explain its limited and insignificant effectiveness on the burden of referrals in the age group. Although a national document on aging has been developed, it has not yet been fully implemented.
All these points indicate that for the elderly to benefit more effectively from medical and health services, there is a need for health reforms appropriate to their conditions. Regardless of these issues, it is possible that in the future, due to the increase in the proportion of elderly people in the population, the burden of referrals will increase, leading to higher costs for the health system. Given the findings, we recommend that planners and policymakers: (1) Design targeted interventions for high-need disease groups such as circulatory and musculoskeletal conditions among the elderly; (2) expand financial protection mechanisms for elderly patients, especially for services currently underrepresented in benefit packages; (3) ensure the implementation of the National Aging Strategy, with cross-sector cooperation and dedicated funding; (4) improve access to rehabilitation and outpatient services, especially in underserved areas.
Finally, since the HTP initially increased the number of referrals, for sustainable effectiveness, it is necessary to pay targeted attention to age groups in the development of national programs. Future policies should seek to improve health and access to services based on the prioritization of groups.
5.7. Limitations and Suggestions for Future Research
Sensitivity analyses were not conducted in this study. Future research is recommended to include sensitivity analyses to assess the robustness of the findings. Additionally, future research should investigate whether disease groups have unique service utilization patterns or unmet needs that were not adequately addressed by HTP interventions.