1. Background
Health systems (HSs) worldwide face mounting challenges in meeting the growing demand for high-quality healthcare services (1). Although health outcomes have improved in many low- and middle-income countries (LMICs), evolving population needs and rising public expectations require higher standards of care. These demands are compounded by ambitious health goals that necessitate innovative approaches to navigate an increasingly complex healthcare landscape (2). One of the most critical challenges is demographic aging, which is expected to accelerate in the coming years. An aging population is associated with a surge in chronic conditions, escalating healthcare costs, and placing greater demands on health services. HSs must adapt to meet the evolving needs of an aging population while simultaneously managing the financial pressures associated with increased demand for care (3). To address these pressures, HSs must systematically assess their structures and processes to ensure they remain aligned with population needs (4, 5). Performance variations further highlight the necessity of effective management in areas such as stewardship, financing, and service delivery (6).
HSs are inherently complex, integrating diverse professional roles and operating in nonlinear, adaptive environments and self-organization (7). To remain responsive to evolving community needs, they require robust, evidence-informed evaluations. The Balanced Scorecard (BSC) framework offers a structured approach to assess performance across key dimensions: Financial sustainability, internal processes, learning and growth, and client/patient outcomes. It serves as a valuable tool for evaluating both internal operations and external impacts (8). Building on the BSC framework (8) and the core functions of the HSs (9), a monitoring and evaluation model can be structured around four dimensions: Population health, service delivery, financing, and growth and infrastructure development (10). These dimensions help elucidate the relationships and factors that shape effective health service delivery and ensure alignment with societal expectations.
To improve performance, HSs must adopt strategic, system-oriented approaches that incorporate evidence-based analysis and frameworks like the BSC. In LMICs, where resources are often constrained, expanding the application of systems thinking is essential to achieving sustainable health gains (11). In this context, system dynamics offers a powerful methodology for analyzing HS behavior. Originating from Jay W. Forrester's work in the 1950s, system dynamics has grown into a robust field, particularly in HSs research. The establishment of the International Society for System Dynamics underscores the growing significance of this methodology in addressing complex issues (12). System dynamics facilitates a deeper understanding of interrelationships among various actors and components, enabling the identification and resolution of multifaceted challenges (11, 13). Through the use of causal loop diagrams and simulation models, decision-makers can visualize and anticipate the behavior of intricate systems (14), offering valuable insights for stakeholders and supporting the development of more effective health policies (15).
In Iran, several studies have applied the system dynamics approach to investigate different aspects of the HS. These investigations include analyses of the relationships between lifestyle factors and health outcomes (16), the structure and performance of the pharmaceutical sector (17), and productivity in human resources for health (18). Additional research has addressed safety management (19), challenges in the insurance industry (20), and the rising costs of chronic diseases (21, 22), all of which emphasize the complex interdependencies within the HS. Despite the valuable insights offered by previous studies, a significant gap persists in the literature: No research has comprehensively examined all dimensions of the HS through a dynamic causal network. This absence of a holistic analysis hinders a full understanding of how various components of the HS interact and influence one another. Most existing studies have focused on isolated factors, overlooking the broader systemic interdependencies essential to informed decision-making.
2. Objectives
To address this gap, the present study adopts the BSC framework to identify key components of the HS and examine their interconnections. By developing detailed stock-and-flow diagrams, the study aims to present a more integrated and dynamic view of the HS. This approach is expected to support the formulation of more effective strategies for addressing health-related challenges and to advance the understanding of systemic issues, ultimately contributing to improved health outcomes in Iran.
3. Methods
3.1. Study Design and Participants
This study is the fourth phase of a broader research project entitled "Developing HS Scenarios for Iran Using a System Thinking Approach." The overall project consists of four phases: Identification of key variables and components of the HS; identification of key drivers and uncertainties within Iran's HS; development of possible and desirable future scenarios for the system; and finally, modeling the dynamics of Iran's HS from 2021 to 2031 (presented in this study). The current phase employs mathematical modeling to examine system behaviors influenced by multiple interacting factors. Using system dynamics tools, the study investigates key structural elements of the HS, including feedback loops, interactions, and time delays, which are critical to understanding system behavior.
3.2. Model Structure
The model structure, comprising stock and flow diagrams and system dynamics modeling, was developed based on:
- Previous phases of the project, including the scoping review of HS components (23), and the analysis of drivers, uncertainties, and scenarios in Iran’s HS (24);
- Indicators and variables identified within the dimensions of the BSC framework;
- Development priorities specified in the economic, social, and cultural development program of the Islamic Republic of Iran in the health sector.
Stock and flow diagrams were used as the foundational modeling technique. Stocks (or levels) represent accumulations within the system, while flows (or rates) indicate how these stocks change over time. These diagrams go beyond causal loop diagrams by providing quantitative structures necessary for simulation modeling.
3.2.1. Population and Population Health Dimension
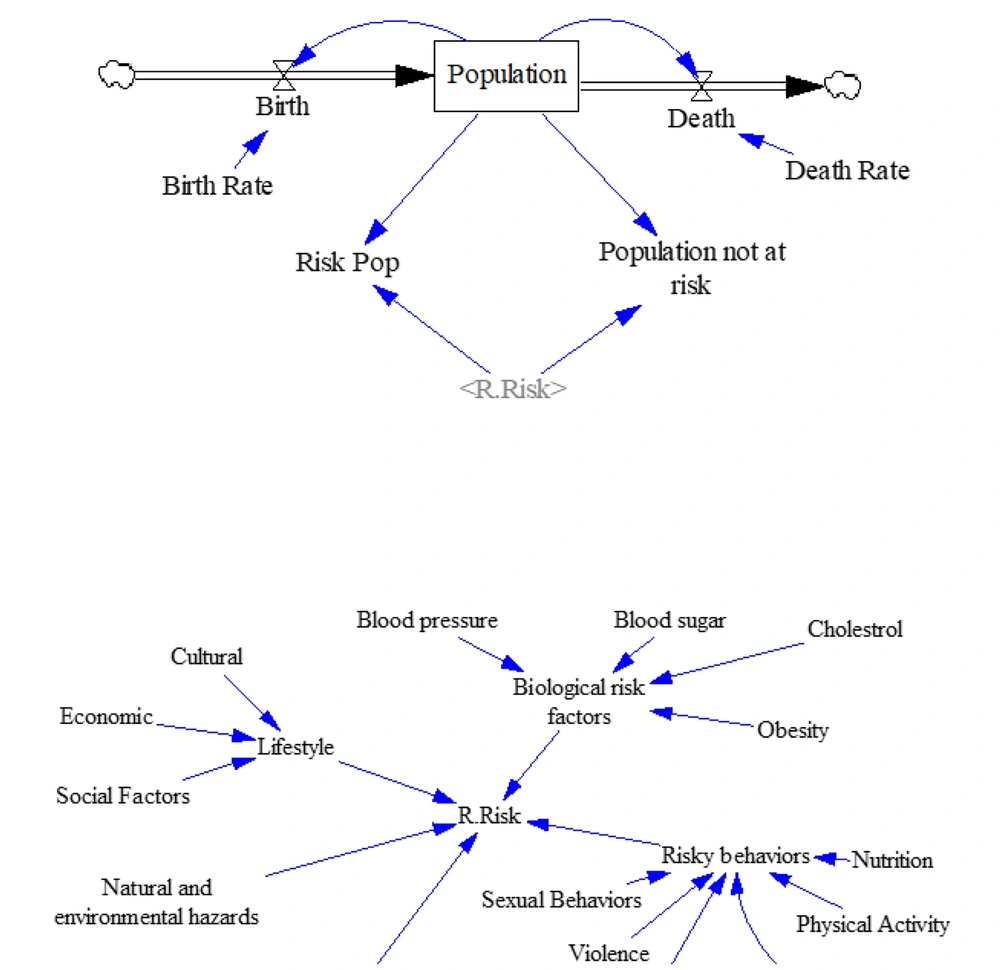
Population dynamics, particularly birth and death rates, substantially affect health outcomes. A balancing feedback loop was observed: While higher birth rates increase population size and can reinforce further births, increased mortality has the opposite effect, creating a stabilizing dynamic (Figure 1). In 2021, Iran’s birth and death rates were estimated at 0.013 and 0.0064, respectively (25), enabling population projections through 2031 (Appendix 1 in Supplementary File). The population was categorized into at-risk and non-at-risk groups based on exposure to health risk factors. This classification is vital for identifying targeted intervention needs.
Risk factors considered include behavioral, biological, lifestyle-related elements, environmental hazards, and the effectiveness of HS itself (Figure 1). Influence coefficients quantifying their impacts were derived from national data (Appendix 2 in Supplementary File).
3.2.2. Service Delivery Dimension
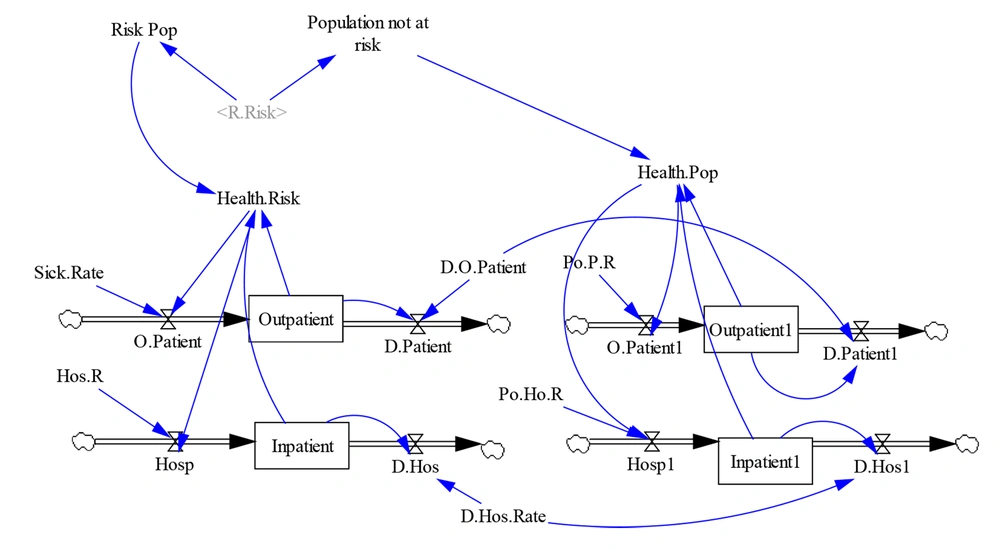
The model reveals a notable disparity in health service utilization between at-risk and non-at-risk populations. Specifically, outpatient visit rates were 0.33 for the at-risk population versus 0.06 for the non-at-risk group (Appendix 3 in Supplementary File). The model adjusts these rates based on mortality trends to accurately capture healthcare demand.
This approach enables better preparation and allocation of healthcare resources, enhancing responsiveness and service planning for various population groups (Figure 2).
3.2.3. Infrastructure Dimension: Hospital Beds, Medical Equipment, and Human Resources
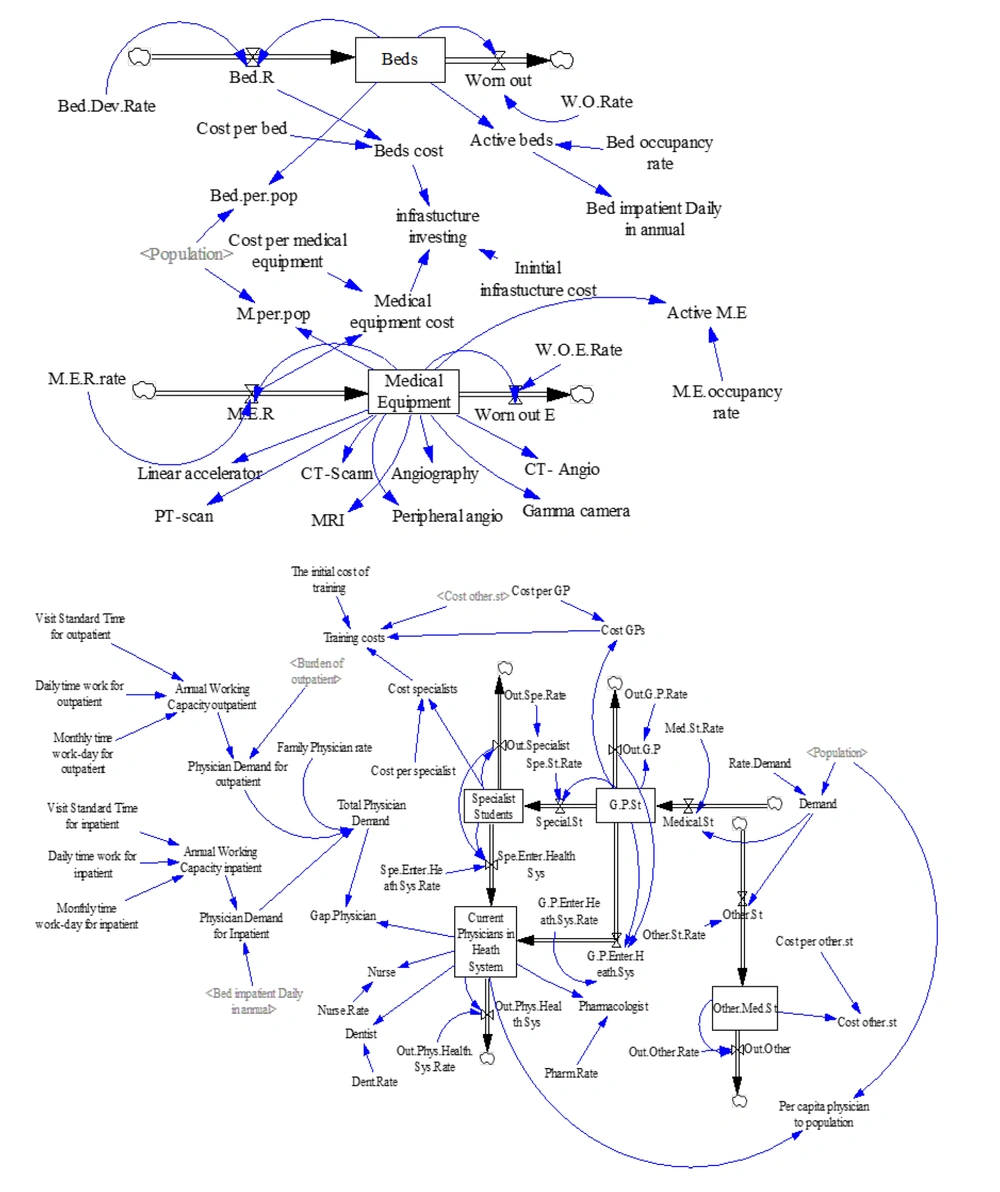
This study highlights the critical role of hospital bed capacity and medical equipment in effective patient care management. The availability of hospital beds is influenced by both development and attrition rates, necessitating increased investments for infrastructure expansion. Additionally, the HS's heavy reliance on imported medical equipment, such as MRI machines, CT scanners, and Gamma cameras, ties the efficiency of diagnostic services to budget allocations and inflationary pressures. These factors underscore the importance of strategic planning in healthcare resource management.
Medical equipment, particularly in diagnostic services, plays an essential role in patient care, with a considerable share being imported. The development and renewal of such equipment are closely tied to budgetary decisions and inflation rates, while the existing inventory is affected by depreciation and obsolescence. This study emphasizes high-impact diagnostic tools such as MRI machines, CT scanners, and Gamma cameras, highlighting their centrality to clinical decision-making and timely treatment. Planning and decision-making within the HS are strongly influenced by the estimation of active hospital beds and functioning medical equipment, both of which depend on utilization rates and real-time inventories. These calculations support more accurate budgeting and may prompt outsourcing certain services to the private sector (Figure 3). Moreover, infrastructure costs associated with hospital beds and diagnostic equipment must be considered for comprehensive financial planning.
This study presents key infrastructure indicators, including an annual bed growth rate of 0.052 (26) and a bed occupancy rate of 0.9 (27), alongside a medical equipment growth rate of 0.0741 (28) and an equipment utilization rate of 0.4 (29). These figures provide insight into the current operational capacity of the HS and guide future resource allocation and strategic planning (Appendix 4 in Supplementary File).
The study also explores the structure of medical education and the demand for healthcare professionals within the HS. Admission to general medical doctorate programs is driven by both societal needs and educational capacity, with students often responsible for covering training-related expenses. A portion of health education funding is also allocated to training students in other medical and allied health fields. The research outlines the possible pathways for medical students, including exiting the educational pipeline, joining the healthcare workforce, or pursuing postgraduate specialization. These transitions, along with retirement rates, directly affect the available pool of physicians within the HS. Understanding these dynamics is essential to maintaining a balanced supply of general practitioners and specialists capable of meeting evolving healthcare needs. Furthermore, the study examines physician work capacity, revealing discrepancies between the supply of healthcare professionals and the fluctuating demand for their services (Figure 3). It also assesses the financial aspects of medical education, including the costs associated with training and deploying healthcare personnel (Appendix 5 in Supplementary File).
3.2.4. Financing Dimension
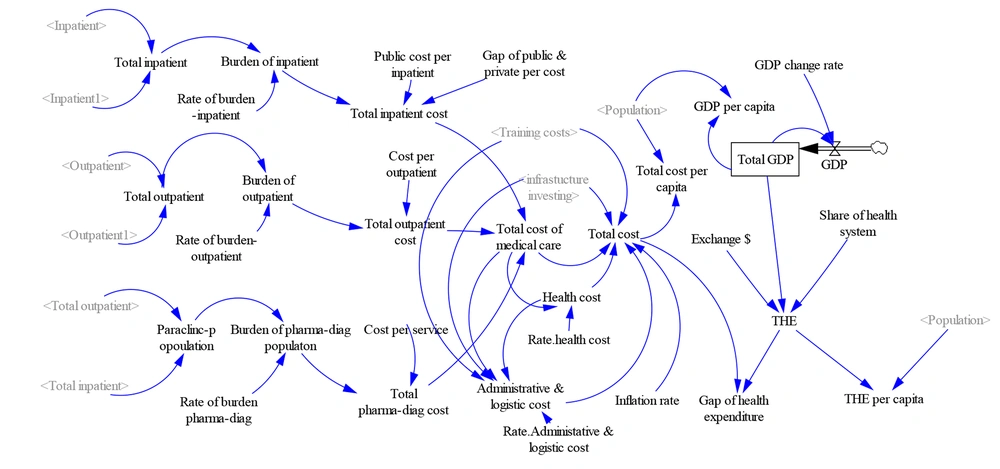
The model provides a detailed analysis of the financial architecture of Iran’s HS, particularly focusing on how gross domestic product (GDP) is allocated to healthcare expenditures. Gross domestic product, as the monetary value of all final goods and services produced in a country during a specific period, serves as the foundation for health budget allocations. The model incorporates key economic variables, including inflation, exchange rates, and the demand for healthcare services. It encompasses both inpatient and outpatient expenditures, as well as costs related to pharmaceuticals, paraclinical services, and infrastructure development.
Moreover, it emphasizes the financial implications of primary healthcare, the training of healthcare personnel, and overhead costs, providing a comprehensive understanding of the sector's fiscal demands. The annual inflation rate specific to the health sector is also integrated into the cost projections, underscoring the sector’s financial vulnerabilities. The analysis reveals a substantial gap between the financial resources required and the actual funding available, indicating recurring patterns of deficit or, less frequently, surplus over time (Figure 4). These findings, derived from reliable sources, present a holistic view of Iran's healthcare financing status as of 2021 (Appendix 6 in Supplementary File).
3.3. Model Validation
The study employs the BSC framework to categorize key parameters across six dimensions. Each dimension is informed by historical data from 2021, allowing for a comprehensive analysis of the HS's performance and requirements. Population-related parameters were extracted from reports by the Statistical Center of Iran (25), while coefficients related to population health were sourced from national surveys and studies (30). Service delivery indicators were derived from statistical reports published by the Iranian Health Insurance Organization and the Social Security Organization (31, 32). In addition, data on hospital beds and medical equipment were obtained from various national reports and studies (26, 28). Human resources parameters were sourced from the National Medical System Organization and expert opinions (33), while financial coefficients were based on national health accounts and official treatment service tariffs (34-36). This multi-source, data-driven approach ensures the model is grounded in valid and contextually relevant evidence, enhancing the robustness of the findings.
Following the dynamic modeling and simulation of Iran's HS, the model's outputs and trend graphs for each parameter were compared with historical data from 2017 to 2021. The trends were found to be consistent and plausible. Furthermore, the results of the sub-models were evaluated through focus group discussions (FGDs) involving eight key experts in healthcare decision-making and policy. These discussions not only confirmed the structural integrity of the model but also validated its accuracy by comparing the outputs with known historical trends in the system.
3.4. Model Sensitivity Analysis
In a related study by Emami et al., key drivers and scenario-generating factors within the Iranian HS were identified (24). As part of that study, a FGD involving six experts with over ten years of academic and executive experience at both national and provincial levels was conducted. Through this process, key HS indicators were identified. Based on contextual feasibility and findings from national survey studies, the experts defined incremental and decremental coefficients for these parameters. These coefficients were then calibrated under three distinct scenarios: Desirable, intermediate, and undesirable. The primary aim of the current study was to evaluate variations in healthcare costs under these scenarios. By forecasting the states of various components in each scenario, the model provides policymakers with a strategic tool for future planning and decision-making.
To assess the model's sensitivity, several influential parameters were systematically varied. These included the physician-to-population ratio, bed-to-population ratio, medical equipment-to-population ratio, inflation rate in the health sector, exchange rate, health’s share in GDP, GDP growth rate, management and support cost rates in the HS, population change factor, and the level of exposure to risk factors. These simulations demonstrated the potential long-term effects of each scenario over a ten-year horizon (2021 - 2031) (Appendix 7 in Supplementary File). One variable of particular importance was "exposure to risk factors," which was reported at 0.35 in 2021 (30). Based on expert consensus, the target values for this indicator were set at 0.2 for the desirable scenario and 0.45 for the undesirable scenario. Achieving these benchmarks would require targeted interventions addressing sub-components of this variable. The study proposed a comprehensive policy package to guide such transformations, serving as a strategic blueprint for future health sector planning (Appendix 8 in Supplementary File).
4. Results
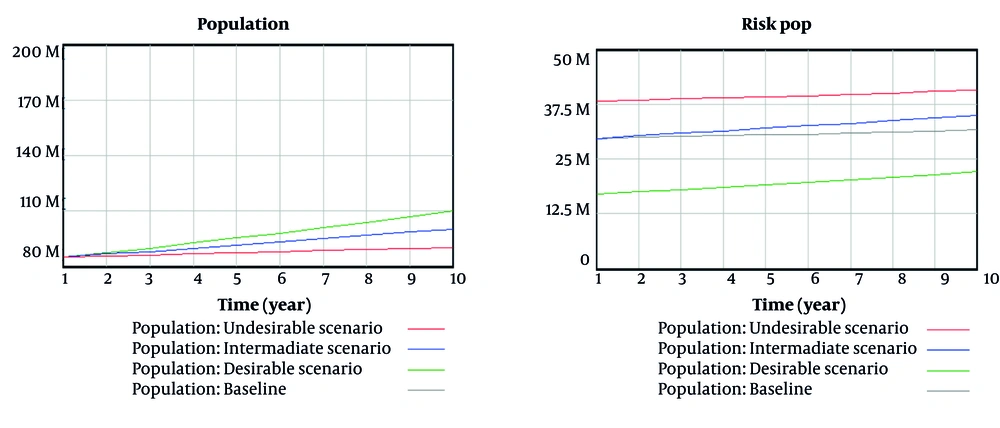
4.1. Population and Population Health
The baseline projection, based on historical trends and data up to 2021, estimated that Iran’s population would reach 90 million by 2031. However, following expert consultations in FGDs, a more aspirational target was outlined in the desirable scenario, aiming for a population of 110 million by 2031. Achieving this goal would require increasing the birth rate from 0.013 to 0.0356. Simultaneously, the desirable scenario targets a reduction in the population’s risk exposure rate from 0.35 to 0.2. This shift would lower the number of individuals at risk from 32 million (as projected in the base model) to 22 million. Conversely, the number of individuals not exposed to health risk factors would rise from 59 million in the baseline to 88 million under the desirable scenario (Figure 5).
The baseline risk exposure level of 0.35 underscores the urgent need for strategic interventions targeting nutrition, physical activity, and obesity (see Appendix 8 in Supplementary File). These areas are expected to require approximately a decade to demonstrate measurable outcomes, during which risk variable levels are assumed to remain relatively stable. Focusing on these specific determinants is essential for sustainably reducing health risks across the population.
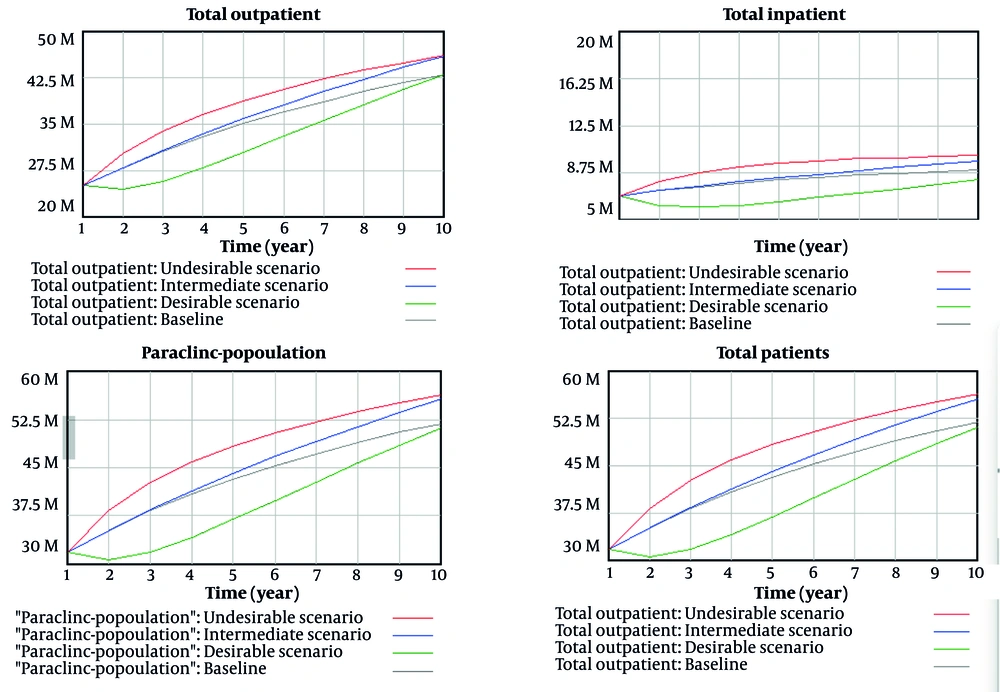
4.2. Service Delivery
The desirable scenario anticipates a 20% reduction in exposure to risk factors, which is projected to result in a tangible decrease in healthcare service utilization. The number of outpatient visits is expected to decline from 46 million to 43 million annually. Similarly, inpatient hospitalizations are projected to decrease from 10 million to 8 million. Pharmaceutical and diagnostic service usage is also expected to fall from 56 million to 51 million (Figure 6), indicating a broader shift in healthcare demand patterns.
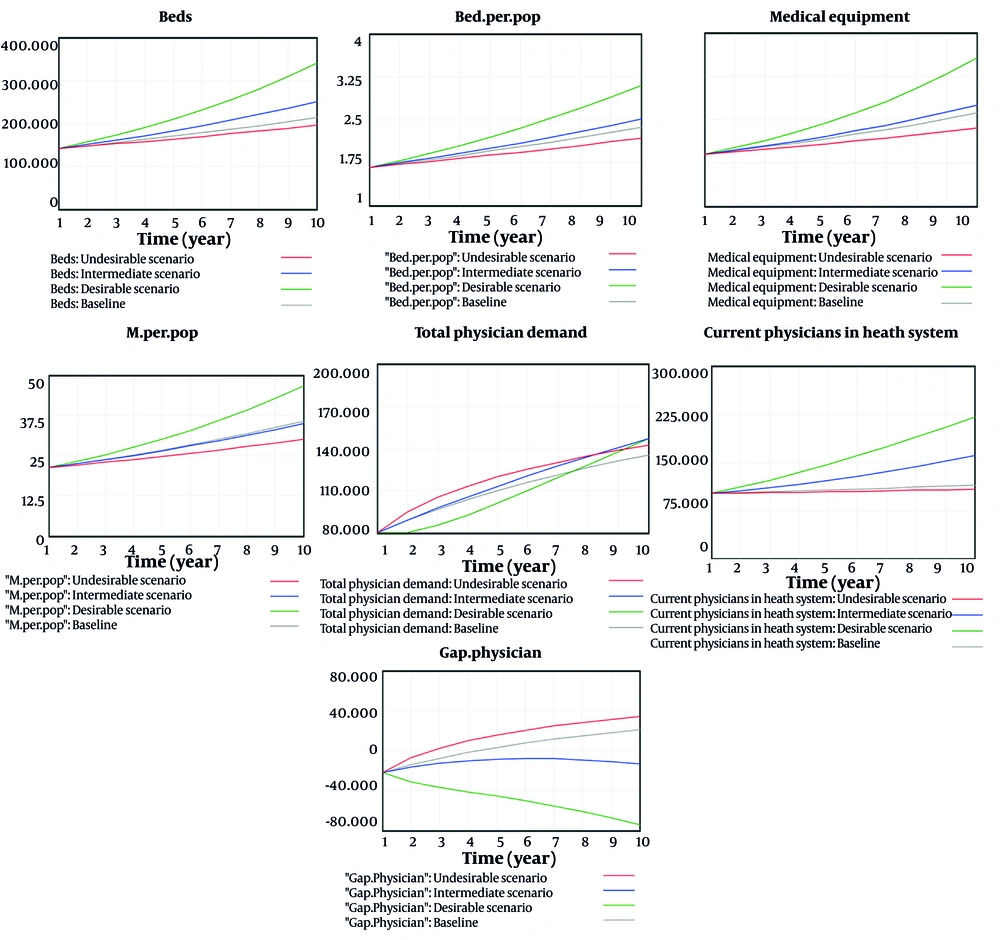
4.3. Growth and Development/Infrastructures
To meet the needs of a growing population, the desirable scenario calls for substantial investment in healthcare infrastructure. Based on a target of three hospital beds per 1,000 population, the number of hospital beds would increase from 214,000 in 2021 to 341,000 by 2031. Likewise, the number of capital medical equipment units is expected to grow from 3,224 to 5,138. The desirable scenario also prioritizes scaling up the health workforce by expanding medical education and recruitment. Consequently, the number of physicians is projected to rise from 114,600 to 220,800, and the number of nurses from 171,900 to 331,200. Similar growth is anticipated in the number of dentists and pharmacists, ensuring optimal provider-to-population ratios and enhancing accessibility to care.
While overall demand for physicians is projected to grow from 135,500 to 146,900, a persistent supply-demand gap remains a concern, particularly in the base and pessimistic scenarios. However, in the intermediate and desirable scenarios, targeted workforce policies are projected to close this gap — potentially even creating a surplus. This could lead to improved service quality and reduced provider workload (Figure 7).
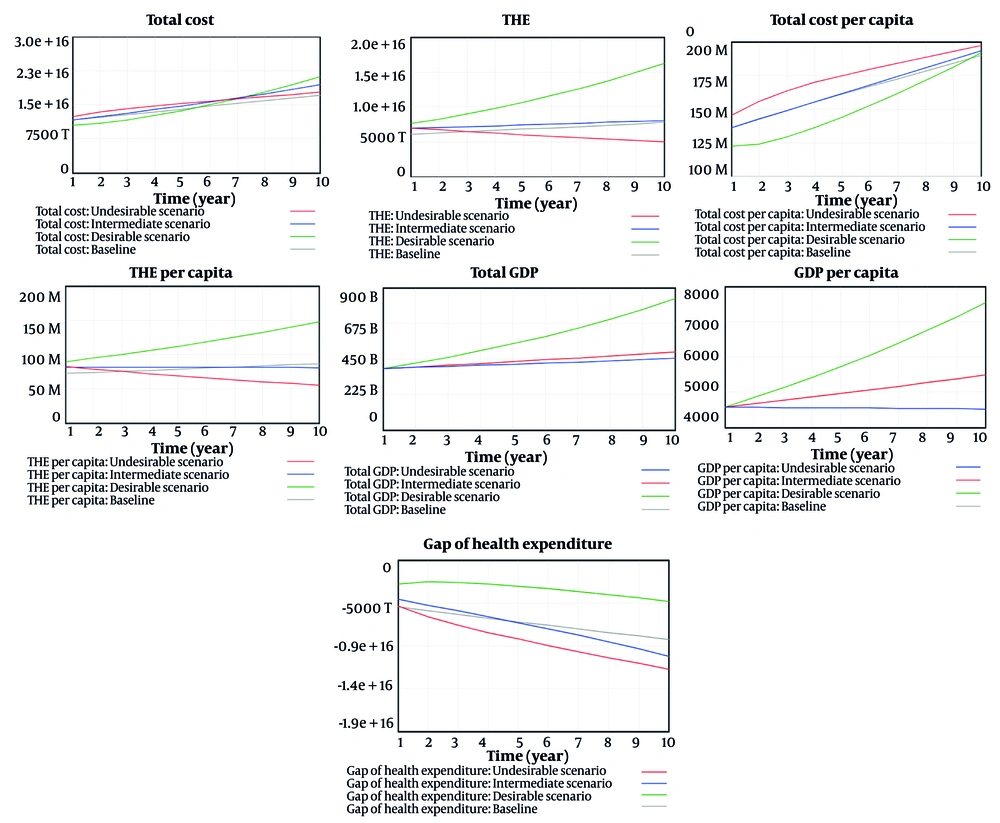
4.4. Health Financing
This study aimed to develop a cost-efficient yet responsive HS scenario capable of meeting future demand. With anticipated population growth, additional investments are required in infrastructure, particularly hospital beds and medical equipment. Total HS costs are expected to increase from 18,000 trillion rials in 2021 to 21,000 trillion rials in 2031. Despite this increase, per capita health expenditure shows a slight decline, suggesting more efficient resource utilization. Total health expenditure (THE) is also projected to rise substantially, from 7,807 trillion rials to 16,000 trillion rials, while per capita THE increases from 87 million rials to 148 million rials. Total health expenditure is expressed as a share of GDP to assess national commitment to health relative to economic capacity.
In the desirable scenario, Iran's GDP is projected to grow significantly, from $494 billion to $830 billion by 2031, the highest growth rate in 15 years. This translates to an increase in per capita GDP from $5,484 to $7,548, providing a more robust economic base for supporting health-related expenditures. Importantly, the report highlights that while health sector costs are presented in trillions of rials, GDP estimates are reported in U.S. dollars to reflect international economic benchmarks and accommodate the effects of exchange rate fluctuations, inflation, and sanctions on the health sector.
Additionally, financial sustainability is expected to improve under the desirable scenario. The gap between total health sector costs and THE is projected to narrow from -9,303 trillion rials to -4,847 trillion rials. This indicates movement toward a more balanced and sustainable budget, driven by strategic investments and better resource alignment (Figure 8).
5. Discussion
This study estimated the foundational model of Iran’s HS for the year 2021, using the BSC framework. Graphical projections suggest that Iran's population will reach approximately 90 million by 2031, indicating a slow population growth rate. Supporting these projections, a 2023 report by Iran’s Ministry of Foreign Affairs and Trade highlighted that 60% of the population is under 30, while only 8% is over 65. Increased access to modern contraceptive methods and widespread government-supported family planning programs have led to a fertility rate below replacement level. As a result, Iran’s population is expected to begin declining by 2050 (37).
Current estimates show a risk exposure level of 0.35%, affecting approximately 32 million individuals (30). At the same time, around 52 million people have accessed health services, suggesting high engagement with the healthcare system and a need for targeted interventions. Non-communicable diseases (NCDs) account for 74.6% of deaths in Iran, according to Mirzaei et al., with an additional burden from road traffic injuries contributing to elevated years lived with disability. These rates exceed both regional and global averages, indicating a pressing public health concern (38). Addressing this requires multi-level prevention strategies focused on modifiable risk factors such as poor diet, physical inactivity, smoking, and dyslipidemia (39).
Iran’s HS infrastructure currently falls short of national standards. While the target is 2.5 inpatient beds per 1,000 population (40), only 2.37 beds are available. Likewise, medical equipment availability stands at 35.8 units per million, below the optimal level of 46.7 (28). Hospital beds are a critical determinant of other health resources, such as workforce and equipment, and their equitable distribution is essential for effective service delivery. Therefore, it is crucial for policymakers to regularly assess and monitor the allocation of these beds to enhance healthcare delivery (41).
Maintaining an optimal physician-to-population ratio is fundamental for effective healthcare delivery. While the ideal benchmark in Iran is 20 physicians per 10,000 population (42), the current rate stands at only 12.73, indicating a substantial shortfall. This gap is further aggravated by population growth, which continues to drive up healthcare demand. The shortage is especially acute in underserved and remote regions, where access to medical services remains limited. A 2023 study emphasized the importance of training and equitably distributing medical specialists as a priority for health policymakers to ensure balanced health outcomes across the country (43).
The COVID-19 pandemic exacerbated existing challenges by intensifying workloads and increasing mental stress among healthcare workers. Instances of violence, suboptimal management, and resource limitations have contributed to burnout and a decline in service quality. Addressing these concerns requires immediate policy actions to improve working conditions, enhance professional support, and safeguard healthcare workers' well-being (44).
The HS responsiveness, particularly in the context of pandemics like COVID-19, is critically influenced by infrastructural capacity. A 2019 study highlighted stark disparities in responsiveness in regions such as Sistan and Baluchestan, where inadequate infrastructure led to poor health outcomes, increased social inequality, and diminished public trust. Enhancing responsiveness calls for systemic reforms including the development of national guidelines and checklists, creation of dedicated oversight offices, professional training for health personnel, and periodic assessments of hospital responsiveness to ensure equity and preparedness (45).
Financial sustainability remains a critical concern for Iran’s HS. Persistent budget deficits reflect a mismatch between service costs and available resources. Although current conditions are preferable to worst-case projections, a 2022 study noted that Iran’s per capita health expenditure is still relatively low compared to global benchmarks, underscoring the need for structural reforms, increased investment, and greater public awareness to enhance HS responsiveness (46). This study, like other research conducted in Iran (47, 48), highlights the rising health costs in Iran, emphasizing the significance of financial protection indicators such as out-of-pocket payments and catastrophic expenditures. These indicators are critical in understanding the challenges faced in health financing within the country.
As chronic diseases become more prevalent and the population ages, coupled with inflation in the HS, health-related expenses are on the rise. This trend is particularly concerning given the disparities in health costs between urban and rural areas, as well as among different provinces. A key strategy to improve financial sustainability involves expanding and integrating health insurance schemes. Long-term plans should focus on unifying fragmented insurance systems, improving access to essential services, and reducing out-of-pocket payments. Special attention must be given to vulnerable populations through the design of comprehensive benefit packages, particularly for outpatient services and chronic disease medications (49, 50).
Furthermore, a 2017 analysis proposed decentralizing governmental functions within the health sector and prioritizing preventive and primary care, both of which could increase system efficiency and reduce costs (51). Forecasting healthcare costs in Iran is a complex undertaking shaped by both real (e.g., economic growth, budget constraints) and nominal (e.g., oil revenues, financial indices) variables. A systemic policy framework is needed, as reliance solely on demand-side monetary interventions may only address nominal components without fully managing real cost pressures (52).
The impact of economic sanctions on Iran has severely disrupted the HS, particularly the pharmaceutical sector. Sanctions have increased suffering and mortality among vulnerable groups, including women, children, and the elderly. This has also contributed to rising rates of vaccine-preventable diseases and mental health challenges. These outcomes underscore the urgent need for global health actors to adopt evidence-based strategies to support sanctioned nations and protect public health (53).
Against this backdrop, this research proposes a comprehensive strategic scenario for Iran’s HS designed to meet the needs of a projected population of 110 million over the next decade. The scenario targets a 20% reduction in population exposure to key health risk factors, aiming to maintain the health of approximately 88 million people. The strategy focuses on strengthening infrastructure for screening, prevention, treatment, and addressing the social determinants of health (SDH), alongside promoting healthier lifestyles. These investments are expected to reduce long-term service delivery and management costs. By strategically allocating financial resources — particularly in preventive care — the system can balance the expected rise in infrastructure expenditures.
A critical element of this scenario is expanding the healthcare workforce by increasing the number of physicians, nurses, pharmacists, and dentists to reach the national goal of 20 physicians per 10,000 population (42). The intermediate scenario anticipates a population of 100 million within the next decade, increasing demand for outpatient and inpatient services. This will likely raise healthcare expenditures, exacerbating an estimated fiscal deficit of 10,000 trillion rials. Despite this, moderate improvements in hospital bed availability and physician recruitment suggest the potential to overcome current service gaps if investment and policy support are sustained.
In contrast, the undesired scenario presents a critical warning. With a projected population of 90 million, and no effective measures to reduce exposure to health risk factors, a large proportion of the population is expected to develop preventable conditions. This will significantly strain the HS’s capacity, especially as health spending as a share of GDP is projected to decline. This scenario also foresees severe infrastructural deficiencies, including a low bed-to-population ratio and shortages in medical equipment, and an intensified workforce shortage. Without significant investments in infrastructure, human resources, and health promotion, the system will be unable to meet either the quantitative or qualitative demands of healthcare provision.
5.1. Study Limitations
Modeling a dynamic HS presents inherent complexities, including potential disruptions and modeling errors that may hinder research progress. To address these challenges, the research team has actively sought guidance from system dynamics experts and committed to improving their technical competencies through specialized online training. These efforts aim to enhance the accuracy and effectiveness of the modeling process. Moreover, this study endeavors to simulate indicators outlined in the Seventh Economic, Social, and Cultural Development Plan of the Islamic Republic of Iran. While some relevant indicators may not have been fully considered in the original policy framework, the custom-built software serves as a flexible information dashboard. It enables the modification of indicators, their baseline values, and interrelationships to align with evolving policy priorities and contextual requirements.
5.2. Conclusions
Achieving the desirable scenario for Iran’s HS and minimizing both HS costs and population-level demand for services requires a strategic focus on the social determinants of health and risk factor reduction. This approach calls for either increased allocation of financial and organizational resources or a reconfiguration of intervention shares through an integrated, multi-sectoral social strategy. This study offers a comprehensive systems analysis of Iran’s HS, identifying its critical drivers and interdependencies while accounting for national contextual factors and development goals. By leveraging Vensim software for dynamic modeling, the research provides policymakers with a robust analytical tool to evaluate, prioritize, and implement targeted interventions and health policies. Additionally, the integration of a real-time information dashboard enhances the capacity of decision-makers to monitor trends in key health indicators and to assess the projected impacts of alternative policy interventions. This technological feature strengthens the potential for evidence-informed, responsive, and adaptive HS planning. Finally, the study outlines two scenario-based policy packages, representing desirable and intermediate outcomes, to guide future reforms. These policy options not only provide a strategic roadmap for strengthening healthcare delivery but also lay the groundwork for a more resilient and equitable HS in Iran.