1. Context
Chronic medical conditions (CMCs) are the leading contributors to morbidity and mortality worldwide (1-3). These conditions are projected to create an economic burden of 47 trillion dollars globally by the year 2030 (1, 4, 5). The World Health Organization (WHO) states that chronic conditions, such as cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes mellitus, represent 74% of all global deaths, with 41 million individuals succumbing to these conditions each year. Notably, 77% of these deaths occur in low and middle-income countries. Early diagnosis, effective screening, and appropriate treatment of chronic diseases are essential strategies for addressing these health issues (6).
Managing chronic diseases involves a complicated process that necessitates the joint effort of healthcare providers and patients concerning long-term treatment, lifestyle modifications, and the monitoring of disease symptoms and signs (7-12). Implementing self-care strategies as a cost-effective approach could enhance the outcomes of chronic diseases by fostering patient adherence to treatment plans, overseeing symptoms, and reacting to disease manifestations (10, 13-15).
Advances in health information technology enable the adoption of various self-care strategies for individuals with chronic conditions through the use of innovative tools such as mHealth (16) and artificial intelligence (AI) (11, 12, 17). Conversational agents (CAs), representing a cutting-edge AI-driven and human-computer interaction (HCI) model, can enhance the management of chronic diseases (18-20). This technology is described as a software application meant to simulate conversations with human users, particularly online (21, 22). It is characterized as a software application designed to simulate conversations with human users, especially in online contexts. It finds application in various facets of human life by utilizing natural language processing (NLP) and sentiment analysis, facilitating text and speech dialogues that resemble human interactions (21, 23).
The CAs offer benefits such as enhanced timely access resulting from the widespread availability of smartphones with Internet connectivity (24, 25), the capability to customize care (25, 26), their cost efficiency (25, 27, 28), and the enhancement of health-related quality of life (29), positioning them as a promising option for the management of chronic illnesses. Kurniawan et al. (20) conducted a systematic review of CAs interventions for chronic conditions, specifically targeting randomized controlled trial (RCT) studies. To the best of our knowledge, there have been three systematic reviews regarding the utilization of CAs in chronic disease management (30-32).
2. Objectives
There are limited studies that align with the objectives of this research. Consequently, this study intended to explore the various types of CAs utilized in the management of chronic diseases, the evaluation metrics for CAs, the AI techniques employed, and to analyze their clinical and technical perspectives to assist in advancing research in this area.
3. Methods
3.1. Study Design
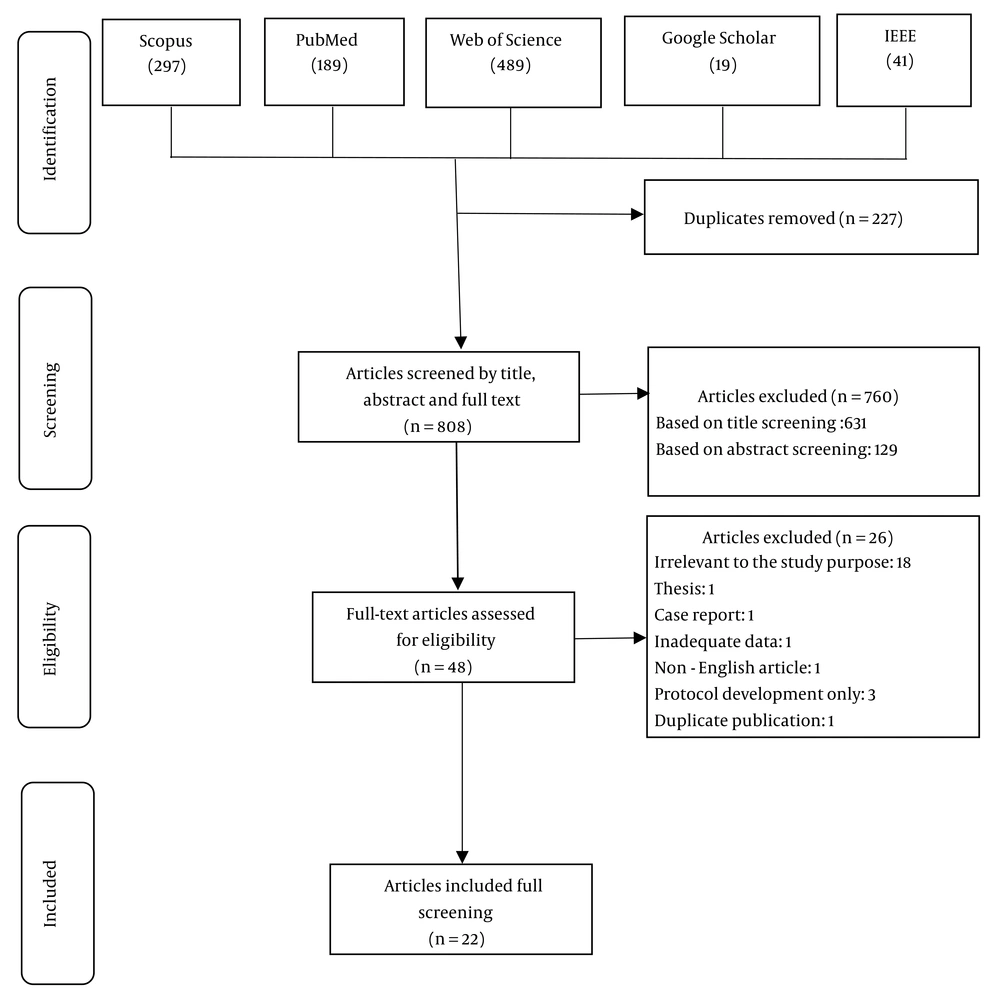
To effectively address the proposed PICO, a thorough systematic review of the available scientific literature was conducted. The PICO for the research question “What are the clinical and technical insights of CAs in managing chronic diseases?” is as follows: Population (P) (people who have chronic diseases), intervention (I) CAs, comparison (C) (is not considered in this study), and outcome (O) (clinical and technical insights of CAs). This review was conducted in accordance with the principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (33) (Figure 1).
The PRISMA checklist defines a framework to direct the creation of a systematic literature review and meta-analysis. This framework is outlined as a series of steps that encompass the review procedure from identification, selection, and appraisal, to the synthesized studies.
3.2. Search Strategy
We explored databases such as PubMed, Scopus, Web of Science (Clarivate Analytics), and IEEE Xplore for related studies up to June 17, 2025. We performed a hand search on Google Scholar to obtain articles that were not included in these databases. The reference lists of the studies included and relevant systematic reviews were also examined, but no new articles were added. Keywords were established by examining the Medical Subject Headings (MeSH) term section of PubMed, professional insights, along with an evaluation of pertinent primary research and reviews. We used two categories of keywords related to CA and chronic disease and selected the search filter ‘‘Title, Abstract, and Keyword’’. The search strategy with the details of the databases to be searched can be seen in Appendix 1 in Supplementary File. Two experts familiar with literature searches were consulted to enhance the comprehensiveness of the studies included and to strengthen the validity of the search strategy employed. The search strategy was subsequently adjusted based on their recommendations for refining the keywords and overall search framework.
3.3. Eligibility Criteria
We incorporated studies that fulfilled the subsequent criteria: (1) All studies, both quantitative and qualitative, that have been published in English; (2) for which the full text is accessible; (3) included a text-based CA in the context of chronic illness management; and (4) articles that are in line with our goal and related to the research question ‘‘Can CAs be a beneficial tool in managing chronic illnesses?’’. The exclusion criteria were (1) studies unrelated to the research question; (2) studies that focus solely on the technical assessment of designed CAs and do not address the usefulness and efficacy of these CAs concerning chronic diseases; (3) review studies, editorials, conferences, brief reports, study protocols, letters, and dissertations; (4) full-text papers that were not accessible; and (5) duplicate publications.
3.4. Study Selection
The findings from all the database searches and other resources were entered into an EndNote 21 library, and duplicates were removed. In the screening stage, the titles and abstracts of all papers were reviewed independently by two authors based on the eligibility criteria. In the next stage, the full text of the papers was independently reviewed by the same two authors to find the relevant studies based on the inclusion and exclusion criteria. Throughout the entire study selection process, the reviewers adopted a cautious approach in dismissing studies based on the eligibility requirements. Additionally, any disagreements were settled through dialogues and mutual agreement between the two researchers. We also reviewed the references of the included studies, and no articles were added at this stage.
3.5. Quality Appraisal of Studies
Following the examination of the studies, two authors engaged in a discussion and reached a consensus on the evaluation of the quality of each study. Due to the variety of articles and existing methods, Mixed Methods Appraisal Tool (MMAT) version 2018 (34) was utilized to evaluate each study. Therefore, the MMAT checklist was used to evaluate the articles. The quality score for each study was determined by dividing the total points obtained by the total points possible. Each study was categorized as low (≤ 59%), moderate (60% to 79%), or high (≥ 80%) based on its quality.
3.6. Data Extraction
According to our protocol, we created a data extraction template using Microsoft Excel (2019). We gathered information on the following aspects: An overview of the studies that are included, clinical insights of CAs, and technical insights of CAs. General information such as the initial author, publication year, research site, and research methodology was collected. Clinical data included chronic disease, applications, measured outcomes, measured tools, key findings, and effectiveness measurement methods. Technical data included CA name, platform, CA languages, response generation, dialogue initiative, input modality, output modality, Chatbot design software, integration with specific external sources, evaluation of CAs, ethics or privacy discussion, and study limitations.
4. Results
4.1. Study Selection
The systematic review of the included databases yielded 1,035 articles, out of which 227 articles were duplicates and excluded. Of the 808 remaining papers, 631 articles were excluded based on titles, and an additional 129 based on abstracts. The screening of the full text of the 48 remaining articles was applied, and 26 articles were excluded according to the established inclusion and exclusion criteria. Ultimately, 22 articles were deemed eligible for the review (Figure 1).
4.2. Quality Appraisal
The quality evaluation of the articles indicated that all were suitable according to the MMAT scores, which ranged from 60 (moderate, n = 4, 18.2%) to 100 (high, n = 18, 81.8%). Given the various study designs in the included studies, we employed the MMAT tool to evaluate their quality. The research questions in all studies were clearly stated, and the data collected provided the opportunity to answer these questions. Qualitative studies had high coherence in terms of data sources, methods of data collection, analysis, and interpretation, ensuring that the findings were sufficiently supported by the data. Of course, some limitations and ambiguities have also been identified in the studies. For example, in quantitative studies (especially RCTs), uncertainty has been observed in the implementation of randomization and blinding of outcome assessors. In three mixed studies, there are also ambiguities in the integration of qualitative and quantitative analyses. Further information can be found in Appendix 2 in Supplementary File.
4.3. Study Characteristics
Among the included articles, the mixed-method was the most frequent study design (n = 10, 45.5%), followed by quantitative descriptive (n = 7), RCT (n = 4), and qualitative (n = 1). Two articles were published in each of the countries of Australia, Switzerland, Greece, Singapore, USA, Portugal, and the Netherlands, and one article was published in each of the other countries, including Taiwan, South Africa, China (Hong Kong), France, Canada, Ecuador, Ireland, UK, and Spain. Article publication dates ranged from 2017 to 2025. Two, four, five, three, and four articles were published in 2025, 2024, 2023, 2022, and 2021, respectively, and only one article was published in each of the years 2017 - 2020, which is summarized in Appendix 3 in Supplementary File.
4.4. Health Care Characteristics and Evaluation Measures
Diabetes mellitus (n = 9, 41%) was the most frequent type of chronic disease in the included studies. Self-care management (n = 13, 59%) was the most frequent application of the CAs in the included studies. Furthermore, usability measurement was the most frequently evaluated outcome, with the System Usability Scale (SUS) being the most frequent tool, and the statistical method was the most frequent effectiveness measurement method in the included studies. The included studies revealed key findings such as improving clinical outcomes across different patient populations, enhancing user satisfaction, and usability of CAs. For example, in the study by Lobo et al. (2017) (35) that focused on patients with heart failure, participants expressed the simplicity of the system, the quality of information, and its user-friendly interaction, which overall increased user satisfaction, improved home monitoring, reduced healthcare costs associated with re-hospitalization, and the effectiveness of treatment as summarized in Appendix 3 in Supplementary File.
4.5. Characteristics of Conversational Agents
Seven studies did not have a CA with a specific name, and the rest of the studies used CAs with different names. The CAs were focused on a variety of populations and chronic conditions such as heart failure (35-37), atrial fibrillation (38, 39), chronic obstructive pulmonary disease (COPD) (36, 40), diabetes mellitus (29, 41-48), cancer (49, 50), asthma (51), chronic kidney disease (CKD) (24), depressive disorder (41), headaches (52), dementia (25), and haemophilia (53). Most of the studies used the Android platform or a combination of Android and iOS for the implementation of CAs. English was the most popular language used in the CAs (n = 14, 63.6%). The AI was used in the majority of CAs for generating responses, and in most of the included studies (n = 14, 63.6%), the CA initiated the dialogue (n = 12, 54.6%). The most frequently used input modality was text, and the output modality was text and voice. Various software was used to design CAs. Most of the designed CAs were not integrated with external sources (such as information systems). In most of the included studies, the usability of the designed CA was measured, and in addition, most of the studies obtained ethical approval and participants' consent. The small sample size was reported as the most frequently mentioned limitation in the reviewed studies. More details are summarized in Appendix 4 in Supplementary File. Due to heterogeneity in outcomes and methods of the included articles, as well as the insufficiency of available data, a meta-analysis was not performed on the data of the articles.
5. Discussion
This systematic literature review examined AI-driven CAs used in managing chronic diseases within the healthcare sector. In terms of clinical impact, the findings revealed improvements in clinical outcomes, users’ satisfaction, and the usability of CAs. In this study, an analysis of the included studies underscores the substantial potential of CAs in facilitating chronic disease management. These digital interventions have demonstrated efficacy across a spectrum of health conditions, from cardiac to respiratory ailments, and from metabolic disorders to cancer. To our knowledge, there have been three systematic reviews on the use of CAs for managing chronic disease (30-32). One of these studies did not include voice-based CAs in their study (30). The researchers revealed that voice-based CAs provide a different user experience than text-based CAs in chronic diseases, particularly for mental health conditions such as depression or substance use. In another study (31), a small number of articles were identified, and most of the studies reviewed were conference abstracts, which are usually excluded from review studies due to eligibility criteria. The review conducted by Bin Sawad et al. (32), which aligns with our findings, did not assess the quality of the articles included. Consequently, it is possible that some lower-quality articles were part of their evaluation. We also report more technical details than in their study, such as the name of the CA, the CA language, the CA design software, etc.
The articles included in the present study show that the key to the success of these technologies is their capacity to increase patient participation in order to promote self-management. In studies related to cardiac care, Lobo et al. (35) and Cardona et al. (37) emphasize in their studies the importance of system simplicity, information quality, and user participation in optimizing the benefits of CAs, especially in end-of-life care and heart failure management. Also, Bickmore et al. (38) and (39), focusing on patients with chronic heart disease (atrial fibrillation), reported that the use of these virtual agents to support chronic disease management leads to significant improvements in self-reported quality of life. In research focused on diabetes mellitus, Gong et al. (29) demonstrated that these interventions can enhance clinical outcomes and, in turn, improve patients' quality of life by empowering them to take an active role in their healthcare.
Another critical factor in the success of AI-based tools is their acceptance and positive user experience. For example, using buttons instead of text can make the technology easier for users to interact with, thereby improving patient acceptance. Cardona et al. (37) focused on the management of patients with heart failure and found that physicians, patients, and caregivers found the content and format to be easy to use and generally accepted it. Roca et al. (41) focused on the management of chronic diseases such as diabetes and depression and reported that the experience of using CAs was very positive, with almost 70% of patients in their study requesting to use CAs after completing the study. Kouroubali et al. (54) and Tsai and Bizy (55) highlight the positive reception of CAs among patients with diabetes and cancer, respectively. These studies demonstrate the potential of these tools to provide an accessible and engaging platform for symptom reporting and ongoing support to patients.
The adaptability of CAs to different healthcare contexts is evident in this research. Roca et al. (41) show the positive impact of CAs on depression and glycemic control in patients with comorbid type 2 diabetes mellitus and depressive disorder, while Kowatsch et al. (51) emphasize the importance of a strong patient-agent relationship in boosting cognitive skills (such as knowledge about asthma) and behavioral skills (like inhalation technique) in children aged 10 - 15 with asthma, along with support from healthcare professionals and family members. More notably, Ter Stal et al. (36) show the stability of patient perceptions of agent quality over time, indicating the robustness of these interventions. Mash et al. (24) also show the great potential of CAs to enhance conventional healthcare methods for individuals with diabetes and to assist in delivering more thorough patient education. Therefore, the use of CAs may be useful in resolving healthcare-related problems more quickly by allowing for error reporting and requesting assistance. In this case, these systems will require more regular monitoring.
Integrating CAs into existing healthcare systems further enhances their potential to complement traditional models of care. As demonstrated in a study by Babington-Ashaye et al. (53), a culturally appropriate digital CA was used by patients with hemophilia in Senegal and their families to enhance education and self-management of hemophilia. Maia et al. (25) also reported that among the benefits of the GECA platform is the ability to communicate and interact with other healthcare systems, and the use of the fast healthcare interoperability resources (FHIR) standard in communications enables seamless adjustment to emerging healthcare information sources. The FHIR facilitates smooth communication among various healthcare applications by providing a standardized framework, ensuring that patient data remains accessible and actionable across different platforms. By using these technologies, healthcare professionals can improve patient care, enhance health outcomes, and optimize resource utilization. Ultimately, the broader implementation of such standards is crucial for unlocking the full potential of digital health technologies.
Our findings from the included studies provide compelling evidence for the efficacy and acceptability of CAs in chronic disease management. Continued research and development are essential to fully realize the potential of these AI-based tools and to address emerging challenges, such as ensuring equitable access, protecting patient privacy, and optimizing algorithm performance. While some studies have explored integration, further research is needed to understand the challenges and benefits of seamlessly integrating CAs into existing systems. Ensuring patient privacy and data security is paramount when using CAs in healthcare. Research should address ethical guidelines and best practices to protect sensitive patient information. Acknowledging and addressing the limitations of CAs, such as technical issues, user barriers, and potential biases, are essential for their effective implementation. By focusing on these areas, future research can contribute to the development of more robust and equitable CAs for chronic disease management.
5.1. Conclusions
This review comprehensively examines the clinical and technical insights of CAs in managing chronic diseases. Findings highlight the pivotal role of effective communication between healthcare providers and patients in improving patient outcomes. Key findings include the significant role of effective communication in enhancing patient satisfaction, treatment adherence, and reducing disease recurrence. This review emphasizes the ability of CAs to transform the management of chronic diseases by improving communication, increasing patient involvement, and enabling personalized care.
The utilization of various techniques such as motivational interviewing and collaborative communication can foster stronger patient-provider relationships and boost patient motivation for adhering to treatment plans. These techniques not only raise patient satisfaction levels but also greatly enhance adherence to treatment. Digital tools, including health apps, telemedicine, and medication reminders, have shown promise in improving chronic disease management and enhancing patient access to care. Additionally, the application of AI and machine learning algorithms can enable predictive modeling and personalized treatment, further improving patient outcomes. Despite these advancements, challenges such as privacy concerns, data security, and technological accessibility persist, necessitating the development of appropriate solutions.
This review is among the first to thoroughly assess both the clinical and technical aspects of CA utilization in chronic disease management and highlights the potential of CAs to revolutionize chronic disease management by improving communication, enhancing patient engagement, and facilitating personalized care. Future studies and advancements should concentrate on overcoming challenges and maximizing the advantages of these technologies, including natural language comprehension, emotion detection, and integration with wearable technology.
5.2. Strengths
This systematic review provides a thorough summary of the literature on the role of communication in the management of chronic illnesses, including 16 studies. The examination of various chronic illnesses and communication modalities, identification of research trends, challenges, and technologies, and evaluation of the overall efficacy of communication therapies are among its strong points. A key aspect of this review is its analysis of the foundational technologies that drive CAs. By delving into areas such as NLP, machine learning, and AI, this review provides an understanding of how CAs function and their capabilities. This understanding is pivotal for developing CAs with enhanced performance and more sophisticated features.
Furthermore, this review scrutinizes the algorithms employed within CAs. By focusing on the intricacies of these algorithms, researchers have gained a more profound comprehension of how CAs process natural language, extract information from text, and generate intelligent responses. These advancements contribute to improving the quality of human-machine interactions and delivering more accurate and valuable information to patients. Beyond the technical aspects, this review evaluates the performance of CAs in real-world settings and their interactions with patients. By investigating the challenges and opportunities of utilizing CAs in clinical environments, researchers have gained a better understanding of patient needs and how to align CAs with these requirements. These findings will facilitate the development of CAs that are more adaptable and responsive to patient needs.
5.3. Limitations
There are a few limitations to take into account, though. The overall results could have been impacted by heterogeneity in the factors, small sample size (cited in six studies), and research approach. Further limiting the generalizability of the data is the absence of a consensus definition for communication treatments and chronic illnesses. Furthermore, the results of this systematic review might have been influenced by the inherent limitations of the primary studies, including small sample sizes, a lack of randomization, or selection bias. To address the issues mentioned earlier in future studies, we recommend utilizing RCTs, increasing sample sizes, and tackling publication bias.