1. Background
Insecticides are considered to be a powerful weapon or silver bullet in developing countries, used to enhance agriculture productivity and to appreciably improve major public health indices (1). Malaria vector control programs rely mainly on either indoor residual insecticide sprays or insecticide-impregnated bed nets (ITNs) (2). Historically, vector control has had a significant impact on malaria control and even today it remains as a corner stone, due to the lack of a reliable vaccine, emergence of drug resistance, and unaffordable potent antimalarial (3).
Indoor residual spraying (IRS) has a long and distinguished history in malaria control. It is thought to operate both through repelling mosquitoes from entering the houses and by killing any female mosquitoes that are resting inside the houses after having taken a meal of blood. Spraying is usually carried out between one and three times per year depending on the insecticide and the seasonality of transmission in a given setting. IRS has the advantage of being able to make use of a much wider range of insecticide products in comparison with ITNs, for which pyrethroids are the only class of insecticide currently used (4).
Approximately 75% of Ethiopia’s landmass is endemic for malaria, with malaria primarily related to altitude and rainfall, and malaria is also characterized by widespread epidemics occurring every five to eight years (5). Despite the availability of effective interventions, malaria remains one of the most important causes of maternal and childhood morbidity and mortality (6). In addition, the health impact is also an issue for food-security and the environment, as the peak transmission season coincides with the major cultivating and harvesting season of the year and this in turn has a tremendous impact on the socioeconomic development of the country (7). IRS has a long history in Ethiopia, and it remains a key component of the national malaria control strategy. In the 2010 fiscal year, 646 619 structures were sprayed and more than 2.1 million residents were protected with IRS. These IRS operations have now been implemented in communities targeted for spraying within each district. It is believed that epidemics may be triggered when focalized Anopheles arabiensis breed in temporary rain pools and An. Pharoensis that breed in lake margins and river beds, spread with the onset of the rains (8).
Knowledge, attitude and practice (KAP) questionnaires have been found to provide insights about pesticide handling practices and pesticide exposure and they have also been used to identify a lack of appropriate knowledge (9, 10), belief and practice. In Ethiopia, insecticide-based vector control interventions serve as the mainstay to minimize the malaria burden. An. arabiensis acts as a primary vector, while An. funestus, An. pharoensis and An. nili are secondary vectors. From this perspective, spray-workers play a key role in the minimization and prevention of malaria transmission, through the application of insecticides. However, frequent insecticide exposure is a matter of grave concern and this can impair workers' health, as well as their occupational competence.
2. Objectives
There have been numerous studies carried out in Ethiopia and in the rest of world, regarding the safe use of pesticide among agricultural-workers. Nonetheless, only a few researches have so far been conducted on IRS spray-worker’s knowledge and practices concerning the safe use of insecticides. Therefore, this study aimed to assess spray-workers' management of insecticide risk indicators and occupational insecticidal poisoning (OIP). The outcomes of the present survey could pave the way to develop and implement health policies as well as improve day-to-day pesticide management practices in the country.
3. Materials and Methods
3.1. Description of the Study Setting, Design and Participants
The study area Omo-Nada woreda (district) is located approximately 285 km south-west of the capital, Addis Ababa in Oromia Regional State, Ethiopia. It is located in the eastern part of the Jimma Zone, between 7°17’and 7°49’N and 37°00’ and 37°28’E, and the mean annual temperature ranges between 25 °C and 33 °C. The estimated population is 254 417, of whom 127 625 are male and 126 792 are women; 12 958 or 5.09% of its population are urban dwellers based on the 2006 statistics (11). Malaria is one of the leading causes of morbidity and mortality in the study area. Because of prolonged periods of exposure to malaria, the residents have adequate awareness about malaria and the importance of malaria prevention and control strategies, in particular IRS. A cross-sectional descriptive study was carried out to assess the spray-workers' knowledge, attitude and practices, with reference to the safe use of insecticides. In the present survey, male respondents constituted 95.3% of the participants and females 4.7%. The age of the respondents ranged from 18 to 45 years and the majority of respondents were 25-34 years old. Nearly 12.3% of the respondents were illiterate, and the remainder were categorized into 1-5th grade, 6-10th grade, 10-12th grade and higher education (45.7%), (18.1%), (17.2%), and (6.6%), respectively. The study participants were professional public health spray-workers only, and they were not involved in spraying on farms. They had been actively engaged in the IRS spraying of the national malaria control program.
3.2. Description of Interview
The interview was carried out by involving all of the 105 IRS spray-workers, serving in the woreda. To improve the quality of the data, pre-testing of the questionnaire was carried out, prior to the actual data collection. It was tested on ten respondents by interviewers, in an area different from the study area, but with a similar socio-demographic pattern. The interview was conducted on the participants' knowledge, attitude and practices concerning the safe use of insecticides, using a pre-tested questionnaire specifically designed for this purpose. Male and female respondents from all age-groups were included. To minimize the possibility of obtaining biased information and variables, the questionnaire which was prepared in the English language, was translated into the local native languages, Oromifa or Amharic, to make it easy to understand and administer for both interviewers and interviewees.
3.3. Description of Data Collection on Safe Insecticides Management
The survey instrument was comprised of a range of questions relating to the spray-workers' knowledge, beliefs and practices of safe insecticide management. The survey was carried out from January 2011 to April 2011, by a team of well-trained and closely supervised local interviewers. The interviewers collected socio-demographic information and the safe use of insecticide data. They were asked to give their knowledge about pesticide usage, customs and practices, in relation to safe insecticide management. The main questions focused on; (1) insecticide poisoning awareness, (2) knowledge about pesticide application, (3) knowledge of the importance of personal protective equipment (PPE), (4) impact of insecticides on human health and environment, (5) attitudes towards PPE usage, (6) practices pre- and post-application of insecticides, (7) self-reported toxicity signs and symptoms, and (8) empty insecticide container disposal practices.
3.4. Measures and Analysis (Karunamoorthi et al., 2011)12
For each of the surveyed members, various measures were created in order to assess the spray-workers' knowledge, attitudes, and practices, towards the safe use of insecticide management, role of insects in disease transmission, importance of insecticides for vector control, adverse impact of pesticides on human health and the environment, appropriate use of PPE, and disposal of empty pesticide containers. Participants whose questionnaire responses indicated a good understanding of the role of insects in disease transmission, the importance of pesticide for vector control, the safe storage of dedicated insecticide containers separate from the family’s regular food, and the adverse effects of insecticides on health and the environment were considered to have a 'good knowledge' of safe insecticide management. Sprayers who reported never bringing empty pesticide containers home from the sprayed sites, who applied insecticides by knapsack sprayer with protective clothing, and who buried empty pesticide containers on the farm, received a 'safe' behavioral score. Spray-workers who reported applying insecticides with appropriate applicators and using suitable PPE received an 'appropriate' score. Respondents who reported showering within 15 minutes of returning home after work received a 'safe' score for that behavior. Frequencies and percentages of each variable were calculated (12).
3.5. Ethical Considerations
The study was approved by the Ethical Clearance Committee of the Jimma University, Jimma, Ethiopia. Before the commencement of the survey, meetings were held with community health workers, community leaders and members of neighborhood associations in which the objectives of the survey were clearly explained. Written consent was obtained from each study participant. Each participant was assured that they could withdraw from the interview at any time if they wish to do so. However, all informants were actively involved and no one declined to finish the interview.
3.6. Description of Statistical Analysis
All statistical analyses were performed using SPSS v Inc., 233 South Wacker Drive, 11th Floor, Chicago, IL 60606-6412.19.0. Range and means were analyzed and appropriate tables, graphs and percentage are displayed. Level of significance was also determined by using 95% of confidence intervals and P-values. A two-sided Fisher's exact test was performed to determine significant associations between safe insecticide practices and the study participant’s characteristics (gender, age, educational status and years of work experience).
4. Results
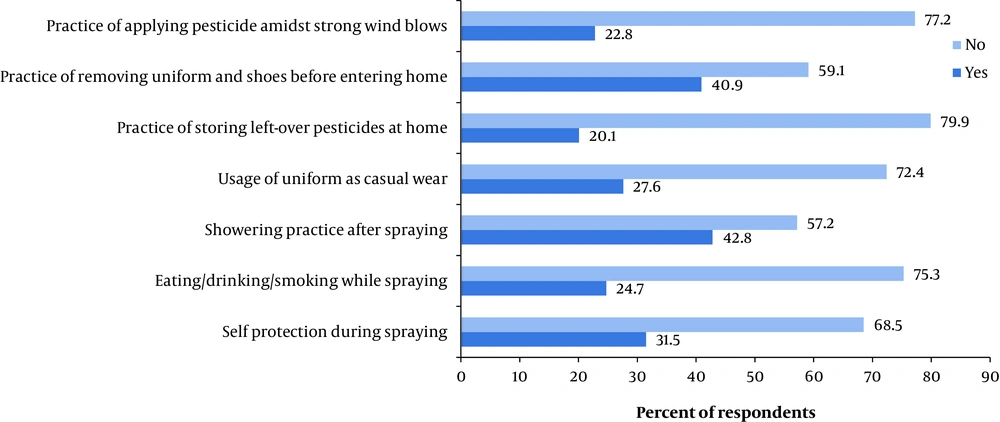
Approximately 52.4% of the study participants were aware of the usage of PPE and 41.9% were able to understand the instructions printed on the label. Nearly 80.9% of the IRS spray-workers admitted that insecticides are hazardous to humans and other organisms ( Table 1 ). Nearly 54.2% of the spray-workers believed that insecticide is the only option to control vectors, and 71.4% that respirators and other PPE are important for spraying safety. Only, 28.5% of the respondents believed that insecticides are harmful to the environment and non-target organisms, while 45.7% perceived that insecticides are harmful to humans, while 47.6% and 6.7% disagree or are uncertain, respectively ( Table 1 ). Overall, 68.5% and 75.3% of the IRS spray-workers pointed out that they never protect themselves during spraying and never smoke, respectively. A total of 72.4% of the respondents mentioned that they did not wear their uniform at the time of spraying. Similarly, 59.1% of the study participants did not change their professional uniform after they came back to their residence ( Figure 1 ).
| Variables | Yes, No. (%) | No, No. (%) | |
|---|---|---|---|
| Do you have any awareness about personal protective equipment (PPE)? | 62 (59.1) | 43 (40.9) | |
| Do you know how to use PPE during insecticide spraying? | 55 (52.4) | 50 (47.6) | |
| Are you able to understand the instructions printed on the label? | 44 (41.9) | 61 (58.1) | |
| Have you ever been informed of the hazardous nature of insecticides? | 84 (80.1) | 21 (19.9) | |
| Do you know that insecticides could have an adverse health impact on human beings and other living things? | 85 (80.9) | 20 (19.1) | |
| Do you know what the purpose of insecticide spraying is? | 90 (85.7) | 15 (14.3) | |
| Agree, No. (%) | Disagree, No. (%) | Uncertain, No. (%) | |
| Do you think that the use of insecticide is the only option to control insect vector of diseases? | 57 (54.2) | 40 (38.1) | 08 (07.7) |
| Do you believe that the respirator and other PPE are important during insecticide spraying? | 75 (71.4) | 25 (23.8) | 05 (04.8) |
| Is it advisable to spray insecticides using untrained personnel? | 22 (20.9) | 71 (67.6) | 12 (11.5) |
| Do you think that insecticides are harmful to the environment and non-target organisms? | 30 (28.5) | 69 (65.8) | 06 (05.7) |
| Do you think insecticides are harmful to human beings? | 48 (45.7) | 50 (47.6) | 07 (06.7) |
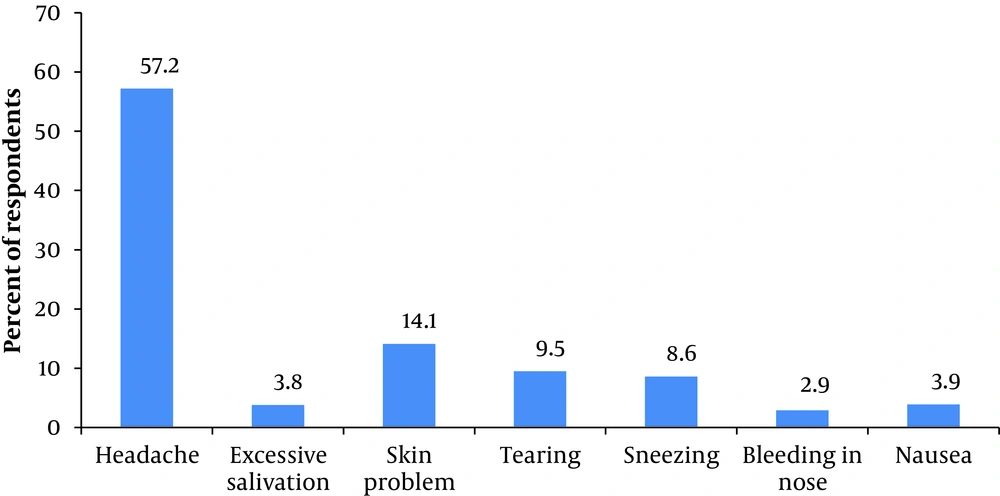
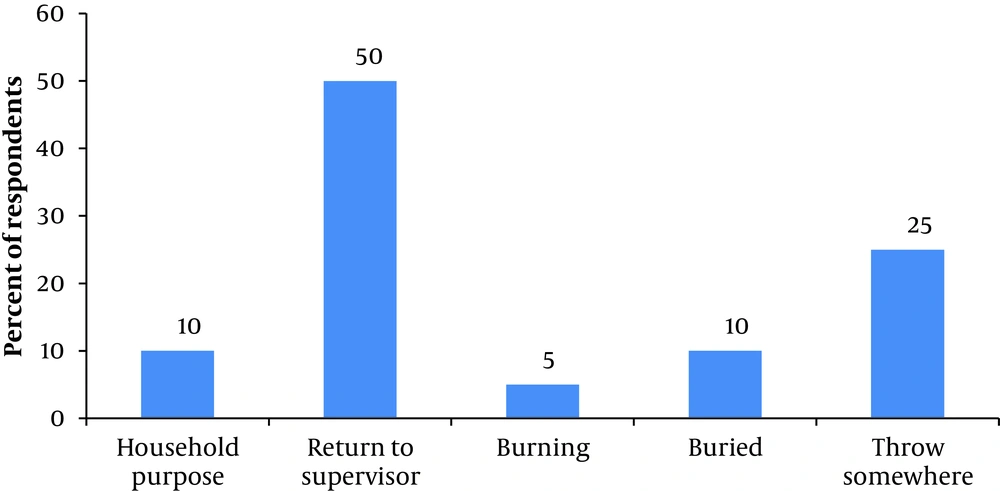
Overall, 57.2% of the spray-workers indicated headaches, and 14.1% skin problems, as self-reported toxicity signs and symptoms during and post application of public health insecticides, respectively ( Figure 2 ). Nearly 50% of the study participants returned surplus insecticide and empty pesticide containers to their immediate supervisor and 25% throw them somewhere. However, 10% use empty insecticide containers for various household needs such as storage of food stuffs and drinking purposes ( Figure 3 ). There was a significant association between a respondent’s safe use of insecticide management with their educational status, gender, age and work experience, and this was determined by a two-sided Fisher's exact test. Results are given in Table 2.
| Socio-Demographic Characteristics | Respondents (n = 105), No (%) | Insecticide Management | FET | |
|---|---|---|---|---|
| Safe (n = 55) | Unsafe (n = 60) | |||
| Gender | ||||
| Male | 100 (95.3) | 52 (52.4) | 48 (47.6) | P = 0.332 |
| Female | 5 (4.7) | 3 (2.6) | 2 (2.4) | |
| Age, y | ||||
| < 18 | 70 (06.6) | 4 (3.6) | 3 (3.3) | P = 0.001 |
| 18-24 | 24 (22.9) | 13 (12.5 | 11 (11.4) | |
| 25-34 | 31 (29.5) | 17 (16.2) | 14 (14.7) | |
| 35-44 | 24 (22.8) | 14 (12.5) | 10 (11.4) | |
| > | 19 (18.1) | 7 (10) | 12 (9) | |
| Educational Status | ||||
| Illiterate | 13 (12.3) | 3 (6.81) | 10 (6.19) | P = 0.001 |
| 1 -5 | 48 (45.7) | 24 (25.14) | 24 (23) | |
| 6-10 | 19 (18.1) | 9 (10) | 10 (9) | |
| 10-12 | 18 (17.2) | 15 (14.3) | 8 (7.6) | |
| 12+ | 07 (6.6) | 4 (3.6) | 3 (3.3) | |
| Work Experience, y | ||||
| < 5 | 51 (48.5) | 20 (26.7) | 31 (24.3) | P = 0.001 |
| 5-10 | 42 (40.1) | 29 (22) | 13 (24.3) | |
| > 10 | 12 (11.4) | 6 (6.3) | 6 (5.7) | |
5. Discussion
Vector-borne diseases including; dengue, yellow fever, Japanese encephalitis, malaria, leishmaniasis, and filariasis, remain severe public health problems in most of the countries in which they are endemic. Insecticides continue to be the primary control tool, in the majority of vector and pest control programs, throughout the world. Almost all malaria vector control programs rely on either indoor residual insecticide sprays or insecticide-impregnated bed nets. Though much effort has been made to introduce alternative environmental, biological, and immunological methods of control, chemical insecticides are still essential for most vector-borne disease control programs, especially where no alternate means of preventing disease transmission are available (2). However, they also have certain undesirable effects on human health and the environment which cannot be ignored (12).
The present study revealed that approximately 59.1% of the spray-workers have an awareness of PPE and 52.4% use PPE ( Table 1 ). While spraying pesticides, the use of PPE could reduce their direct contact with skin, and inhalation of pesticides, thereby, potentially reducing acute and chronic health hazards of pesticides for the sprayers (13). These results are quite consistent with previous studies conducted in Ethiopia and they have also shown that; the handling and storage of chemical pesticides, personal hygiene and the proper use of personal protective equipment by farm-workers are below standard (13, 14). A recent study also found that only a few workers use some sort of PPE, and most do not take a shower after pesticide application (12). The proper use of PPE reduces the worker’s exposure to insecticides and safe insecticide management practices reduce the risk to workers, the public, and the environment.
Provision of PPE to the spray-workers was lacking and where it had been provided it was often not adequate. Proper usage of PPE is one of the key factors in avoiding insecticide poisoning. Being provided with face masks was also found to be a significant risk factor. This might mean that the type of PPE used was either inappropriate or was not being used properly (15). Literacy and inadequate awareness may be a part of the problem, as the majority of the study participants had limited education. The minimal use of PPE is also due to a lack of awareness and affordability. Creating increased awareness and providing PPE free of charge or at low cost may be a possible remedy to the current situation. Farmers usually mix insecticides in large barrels without using gloves, resulting in considerable dermal exposure (16). An educated individual may know the health and environmental impacts due to insecticide use, but may not wear protective clothing due to either poor economic conditions or a hot climate (17), as some sprayers are reluctant to wear gloves in hot weather. Such unsafe practices have also been reported among pesticide sprayers in the Mississippi Delta (18).
This present study also stated that nearly 58.1% of the respondents were unable to understand the instructions printed on the label. In Ethiopia, only a limited numbers of insecticides have instructions for its application in Amharic (native local language), whereas on most other insecticides the instructions and warnings are printed only in English. Since the majority of the farmers are illiterate and a considerable number of them have not obtained any formal education, they may not understand the instructions. In addition, a few farmers have complained that these instructions are too technical. The importance of this issue has also been pointed out by Miller (2004) (19), and labeling pesticides with systems that could be read by the applicator would be an important step in the development of pesticide application practices. Anecdotally, there has been a report that even if able to read, some farm workers are quite reluctant to read the manufacturer’s labels (20). Therefore, concerned authorities must act immediately to label the instructions in the native local language with simplified pictorial representations. Moreover, a special orientation should be launched at the kebele (village) level to make them aware of the safe use of pesticide management to resolve this crisis (1).
Almost, 80.9% of the study participants had awareness that insecticides may cause adverse health impacts on humans and other living things ( Table 1 ). The level of awareness about pesticide poisoning is considerably higher when compared with a very recent study conducted in Ethiopia, which found that on average 58.8% of the farmers have self-reported toxicity symptoms related to pesticides, with headaches being the most common one and similarly, 67 (38.2%) farmers also indicated salivation and vomiting symptoms (1). This difference could possibly be explained due to the fact that spray-workers are highly professional and apply insecticides more frequently than farmers.
It has been observed that pesticides cause serious public health hazards and environmental pollution due to the haphazard usage of pesticides (1). Table 1 indicates that 54.2% of the respondents believe that insecticides are the only option to control vectors and 28.5% that insecticides are harmful to the environment and non-target organisms. The results accord with a study conducted in Ethiopia where the majority of the farmers surveyed agreed that pesticides are harmful, and that they cause environmental pollution and kill non-target organisms as well (1). Similar studies have reported that the majority of agricultural workers consider pesticides to be harmful to the environment, particularly to rivers, air and soil (21). Pesticide problems have also been identified as a major environmental health problem in the Gaza Strip (22). Papworth and Paharia (1978) (23) stated that pesticides by their very nature are toxic and can be hazardous to users if not handled properly. Most of the spray-workers (57.2%) do not have a shower after spraying, and 59.1% of them are not in the habit of changing their uniform and shoes prior to entering their home ( Figure 1 ). These findings are comparable with an earlier study, conducted in Nepal, which reported that half of the respondents do not take a shower after spraying and one-third of them wear the same clothes used during spraying continuously (17). About 24.7% of the spray-workers eat, drink and smoke during pesticide handling ( Figure 1 ). Avoiding eating, drinking or smoking during spray application is one of the most desirable practices that can be done in order to considerably reduce the risk of pesticide poisoning. These results are supported by earlier studies conducted in Nepal in which almost all of the males and female respondents did not eat, drink or smoke, during pesticide application and in Lebanon the vast proportion of the respondents stored pesticides away from food and did not eat during application. Overall, 77.2% of respondents did not spray insecticides when it was windy or stormy ( Figure 1 ). This is quite a desirable practice and the results accord with a study in Lebanon that reported that a significant proportion of spray-workers were applying pesticides in the direction of the wind (24), whereas a study in Nepal showed that some of the participants did not account for the wind direction (17).
More than half of the study participants (57.2%) mentioned; headaches, excessive salivation, skin itching, tearing, sneezing and other toxicity signs due to insecticide exposure ( Figure 2 ). Several researchers observed a similar finding in their studies (24, 25). Long-term pesticide exposure led to a feeling of dizziness and dryness of skin. (26). The prevention and management of pesticide poisoning, enhanced surveillance, and training, are extremely important issues and they must be carried out by the appropriate authorities. In addition, providing training for healthcare providers and local clinic staff on first aid measures and recognition of poisoning cases, are extremely important in order to avoid pesticide poisoning related morbidity and mortality (1).
The proper disposal of empty pesticide containers is one of the most important measures that need to be taken for the safe use of pesticide management (1). About, 10% of the spray-workers have been observed using empty pesticide containers for various household purposes, such as the storage of food stuffs and drinking water ( Figure 3 ). This undesirable practice is extremely minimal, when compared with earlier studies in Ethiopia which had reported that nearly 77.2% of the farmers had been using empty pesticide containers for various household purposes (1), and in Nigeria, the majority of farm workers (35.4%) had been using empty insecticide containers to store cooking oil (27). Nearly, 25% of the participants were observed throwing empty containers anywhere and they were not disposed of correctly. These results are also similar to an earlier study conducted by Recena et al. (2006) (26).
Statistical analysis (two-sided Fisher's exact test) confirmed that there was no statistically significant association between safe insecticide practice with gender (P = 0.332), whereas, there were strong correlations found with; age (P = 0.001), educational status (P = 0.001) and years of work experience (P = 0.001). Safe insecticide practice and gender (P = 0.332) was not statistically significant ( Table 2 ), and this finding is contrary to a study conducted by Atreya (2007) (17) in Nepal, which reported that almost all of the respondents were aware of the negative impact of pesticide use on human health and the environment irrespective of gender; however, females were at higher risk due to lower levels of pesticide safety and awareness. It is interesting to note that the earlier study was conducted among farm workers, most of whom were illiterate; on the other hand, the present study participants are professionals therefore gender may possibly not play a crucial role with reference to safe insecticide practice. Perhaps it is now obvious that low levels or limited formal education, age and years of work experience are the major determinants for the safe practice of insecticide handling and practice. An educated individual may be more aware of the health and environmental impacts (17), and therefore there is the possibility of improved safe use of pesticides among them than in those who are illiterate. Educational and awareness activities of insecticide use practices and safety precautions are crucial at different time intervals. Occupational insecticidal poisoning issues will only improve if the population is better educated on the fundamental principles of pesticide use and safety measures (17). Therefore, the authorities concerned must find an appropriate strategy in terms of providing pesticide safety education and orientation training programs in order to reduce the risk of pesticide poisoning in the near future. Moreover, the distribution of posters and leaflets concerning occupational health issues could also be an effective measure. A major factor in pesticide contamination or poisoning in developing countries continues to be the unsafe use or misuse of pesticides (28).
Explosive global economic development, the movement of people, water projects, climate change and increased urbanization, have substantially altered disease biology and transmission dynamics. Malaria is a disease of poverty, inflicting serious negative impacts on health and socioeconomic development in the poorest countries of the world. However, since malaria is both a preventable and curable illness (29), history has shown that this can be achieved through the implementation of sustainable malaria control strategies like IRS. Indeed insecticides are a powerful weapons in the fight against vector-borne diseases, in particular those which combat malaria. Historically, IRS was proved to be effective during the Global Malaria Eradication Campaign (1955-1969) in most hitherto malarial endemic countries, and over the past several decades it has been an important component of the malaria control strategy in Ethiopia. The present study results suggest that although the majority of the spray-workers have adequate awareness about the safe use of insecticides, most of them are reluctant to put this into practice, either due to inadequacy of their PPE or negligence. In addition, a sizable number of workers still have limited knowledge and unsafe practices. Turning knowledge into action is the important task in order to reduce the risk of occupational insecticide poisoning.
To eliminate misunderstandings and undesirable practices regarding the safe practice of insecticide management, this investigation led to the following recommendations;
Training is extremely important in the prevention and management of pesticide poisoning, and for enhanced surveillance, therefore, training must be carried out by concerned authorities.
Provision of an adequate number of PPE for the sprayers may reduce the risk of occupational insecticide poisoning.
Appropriate orientation programs must be organized in order to prevent occupational exposure to insecticides.
Proper maintenance of spray equipment increases the quality of the spraying, which will ultimately reduce program costs and also provide a check on environmental and human health hazards.
Providing training for healthcare providers and local clinic staff on first aid measures and to recognize poisoning cases, are extremely important in order to avoid pesticide poisoning morbidity and mortality.