1. Background
Pain has been defined as “an unpleasant sensory and emotional experience associated with actual and potential tissue damage, or described in terms of such damage” (1). Recently, it has been gradually acknowledged that pain is a major community health problem and a source of personal and family suffering (2).
According to definition, chronic pain is “pain that has lasted 3 months or longer, is ongoing on a daily basis, is due to non-life-threatening causes, has not responded to currently available treatment methods, and may continue for the remainder of the patient’s life” (3). Both physical health and psychological wellbeing can be affected by chronic pain. An intrusive role can be played by chronic pain in all aspects of an individual’s living, ranging from home and work to leisure and social relationships. Furthermore, chronic pain has implications for medical care usage and the appropriation of health resources (4) and is related to the worst quality of life in contrast to other chronic condition such as chronic lung or cardiovascular disease (5).
The prevalence of chronic pain in adult populations has been estimated 2 - 40% (6) and is rising based on the findings of population-based studies (7). In addition, chronic pain imposes both direct and indirect costs on individuals and society (8).
The epidemiological study of chronic pain is essential in order to plan for health budgets, prevention, intervention and modification of risk factors by policy makers. According to our knowledge so far, no extensive research has been conducted on the prevalence of chronic pain in Iran.
2. Objectives
This study aimed to provide epidemiological data of chronic pain and to identify its related risk factors in Tehran, capital of Iran.
3. Patients and Methods
3.1. Data Source
A cross-sectional study titled as the second round of “Urban HEART” project was conducted in Tehran in October 2011. This study was sponsored by the municipality of Tehran and in total, 37000 households in 22 municipal districts and 368 neighborhoods were covered in this population-based observational survey. One of the objectives of this study was to assess the prevalence of pain in 22 municipal districts of Tehran. Related data were analyzed in this paper.
3.2. Sampling Design
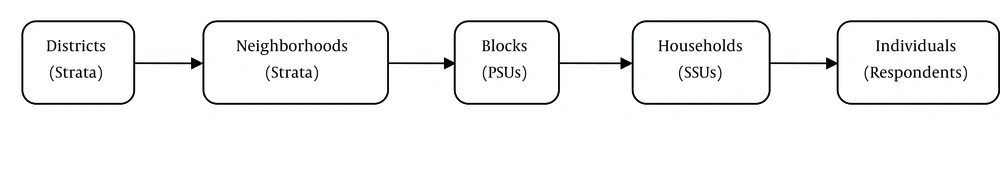
Tehran is the capital of Iran and has a population of around 8.5 million and divided into 22 municipal districts. Each district is composed of a number of neighborhoods and each neighborhood is composed of a number of blocks. To collect data in this study, a multistage sampling was used (Figure 1).
Selection strategy of sampling units, including the following:
- To cover 100% of Tehran’s population, the comprehensive map of Tehran in 2011 was used as the sampling frame.
- In both of the first and second stages, a stratified sampling was used and 22 municipal districts and 368 neighborhoods were regarded as stratum, respectively.
- In the third stage, a cluster sampling was used and each block was regarded as primary sampling units (PSU) which was selected in each neighborhood systematically with two-dimensional using a GIS (geographic information system) map.
- Each household was considered as a Secondary Sampling Unit (SSU) and 8 households in each block were selected systematically.
- To select households in each block, all rings were counted by questioners at first. Then the total number of rings divided by eight and the “gap number” determined.
- In order to complete individual questionnaires (e.g., pain questionnaire) and avoid intracluster correlation (household), one person from each household was interviewed. For this purpose, a statistical domain based on four age groups (15 - 24, 25 - 44, 45 - 64 and 65+) and both male and female sexes, a table of eight cells, was considered. Then, sampling was performed in such a way that one person would be selected in all age-sex groups (in each cell) in each block.
3.3. Sample Size Calculation
Using the formula, n=z2pqd2 the sample size for each district based on variables with a prevalence of 10% or more and considering a confidence interval of 95% and a margin of error of 0.015, was determined as 1535 households which expanded to 1600 households due to the potential loss amount. Also, the sample size for each district was calculated using the probability proportional to size method within each district (strata).
3.4. Participants
The eligible participants had to satisfy the inclusion criteria. The inclusion criteria were as follows: (1) Being Iranian; (2) 15 years of age or older; and (3) be consent to participate in the study.
3.5. Survey Questionnaire
In this multipurpose project, there were several questionnaires. To collect data on pain, a self-administered questionnaire was used, which had been designed to provide information about the prevalence of pain in different areas of the body by experts. The questionnaire had a good internal consistency coefficient (Cronbach’s alpha coefficient = 0.87). Patients with pain and chronic pain were identified by affirmative answer to two questions, respectively. “Do you have any pain now?” and “Does this pain have lasted more than three months?” (1). Based on this questionnaire the data of 23457 people were obtained (The response rate was 87%).
The general information questionnaire of household members was used to obtain socio-demographic data on gender, age, height, weight, educational status, occupational status and marital status. general health questionnaire (GHQ-28) and short form (SF-12) were used to assess the mental health and health-related quality of life, respectively. Satisfaction of household income was assessed by household expenditure questionnaire. Also, smoking status and chronic disease (diabetes and cancer) were identified based on tobacco use and addiction questionnaire and chronic disease questionnaire, respectively. The reader can refer to the previous publications written by Asadi Lari et al. and Vaez Mahdavi et al. for more information on the questionnaires (9, 10).
3.6. Statistical Analysis
The sample characteristics were demonstrated using descriptive statistics. The prevalence of chronic pain was calculated based on the sampling weights. Relationship between chronic pain and independent variables were analyzed using Pearson’s correlation coefficient. Multiple logistic regression models were used to determine risk factors for all types of chronic pain. Odds ratio (OR) and confidence interval (95% CI) for the odds of occurring each type of chronic pain was reported. For all statistical analysis, a significance level of 5% was considered. All analyses were performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA).
4. Results
4.1. Characteristics of Sample
Data of 23,457 individuals were analyzed, which 43.6% (10230) of them were male and 56.4% (13227) were female. The mean age of the respondents was 43.78 years (SD = 16.7; range: 15 - 90). Table 1 represents other characteristics of the sample.
| Variable | Male (n = 10230) | Female (n = 13227) | χ2 | P Value | ||
|---|---|---|---|---|---|---|
| Chronic Pain | Chronic Pain | |||||
| No, (n = 8048) | Yes (n = 2182) | No, (n = 9769) | Yes, (n = 3458) | |||
| Age group, y | 460.2 | < 0.001 | ||||
| 15 - 24 | 1176 (87.3) | 171 (12.7) | 1329 (86.5) | 208 (13.5) | ||
| 25 - 44 | 3086 (81.9) | 681 (18.1) | 4792 (77.3) | 1404 (22.7) | ||
| 45 - 64 | 2494 (75.8) | 795 (24.2) | 2803 (67.5) | 1347 (32.5) | ||
| ≤ 65 | 1292 (70.0) | 535 (29.3) | 845 (62.9) | 499 (37.1) | ||
| Education | 381.2 | < 0.001 | ||||
| Illiterate | 366 (66.3) | 186 (33.7) | 621 (59.7) | 419 (40.3) | ||
| Primary and secondary | 1580 (74.5) | 542 (25.5) | 1976 (68.1) | 927 (31.9) | ||
| High school qualifications | 3404 (79.5) | 877 (20.5) | 4444 (74.8) | 1501 (25.2) | ||
| College education | 2698 (82.4) | 577 (17.6) | 2728 (81.7) | 611 (18.3) | ||
| Occupational status | 346.1 | < 0.001 | ||||
| Unemployed (looking for work) | 792 (79.0) | 211 (21.0) | 416 (82.9) | 86 (17.1) | ||
| Housewife | - | - | 6843 (72.1) | 2644 (27.9) | ||
| Student | 787 (86.4) | 124 (13.6) | 899 (86.0) | 146 (14.0) | ||
| Have income without work | 232 (78.9) | 62 (21.1) | 113 (68.9) | 51 (31.1) | ||
| retiree and pensioner | 1882 (71.7) | 741 (28.3) | 634 (66.9) | 313 (33.1) | ||
| Employed | 4355 (80.7) | 1044 (19.3) | 864 (79.9) | 218 (20.1) | ||
| Marital status | 371.2 | < 0.001 | ||||
| Married | 5587 (76.5) | 1717 (23.5) | 7130 (73.2) | 2606 (26.8) | ||
| Widowed | 191 (69.7) | 83 (30.3) | 874 (63.3) | 507 (36.7) | ||
| Divorced | 124 (81.6) | 28 (18.4) | 207 (69.9) | 89 (30.1) | ||
| Single | 2146 (85.8) | 354 (14.2) | 1558 (85.9) | 256 (14.1) | ||
| Depression | 209.1 | < 0.001 | ||||
| No | 5571 (81.9) | 952 (18.1) | 3327 (69.2) | 1480 (30.8) | ||
| Yes | 2477 (72.2) | 1230 (27.8) | 6442 (76.5) | 1978 (23.5) | ||
| Anxiety | 576.6 | < 0.001 | ||||
| No | 2337 (68.5) | 1075 (31.5) | 3429 (66.2) | 1747 (33.8) | ||
| Yes | 5711 (83.8) | 1107 (16.2) | 6340 (78.7) | 1711 (21.3) | ||
| Obesity | 532.2 | < 0.001 | ||||
| No | 7117 (79.0) | 1894 (21.0) | 8077 (75.0) | 2687 (25.0) | ||
| Yes | 931 (76.4) | 288 (23.6) | 1692 (68.7) | 771 (31.3) | ||
| Smoking | 260.1 | < 0.001 | ||||
| No | 6034 (79.5) | 1553 (20.5) | 6550 (73.0) | 2425 (27.0) | ||
| Yes | 2014 (76.2) | 629 (23.8) | 3219 (75.7) | 1033 (24.3) | ||
| Satisfaction of household income | 91.4 | < 0.001 | ||||
| None | 3683 (76.1) | 1154 (23.9) | 4407 (71.0) | 1796 (29.0) | ||
| Somewhat | 3620 (80.5) | 877 (19.5) | 4552 (75.8) | 1451 (24.2) | ||
| Quiet | 745 (83.1) | 151 (16.9) | 810 (79.3) | 211 (20.7) | ||
| Diabetes | 116.2 | < 0.001 | ||||
| No | 7627 (79.2) | 1998 (20.8) | 9286 (74.8) | 3135 (25.2) | ||
| Yes | 421 (69.6) | 184 (30.4) | 483 (59.9) | 323 (40.1) | ||
| Cancer | 11.5 | < 0.001 | ||||
| No | 8017 (78.7) | 2172 (21.3) | 9733 (74.0) | 3427 (26.0) | ||
| Yes | 31 (75.6) | 10 (24.4) | 36 (53.7) | 31 (46.3) | ||
| Exercise | 30.3 | < 0.001 | ||||
| No | 4917 (77.5) | 1431 (22.5) | 6550 (73.0) | 2425 (27.0) | ||
| Yes | 3131 (80.7) | 751 (19.3) | 3219 (75.7) | 1033 (24.3) | ||
a Data are presented as No. (%).
4.2. Prevalence of Chronic Pain
The prevalence of chronic pain was 24.0%. Figure 2 presents the prevalence of chronic pain types. Chronic low back pain and chronic knee pain were the most common complaints (12.4% and 11.2%, respectively).
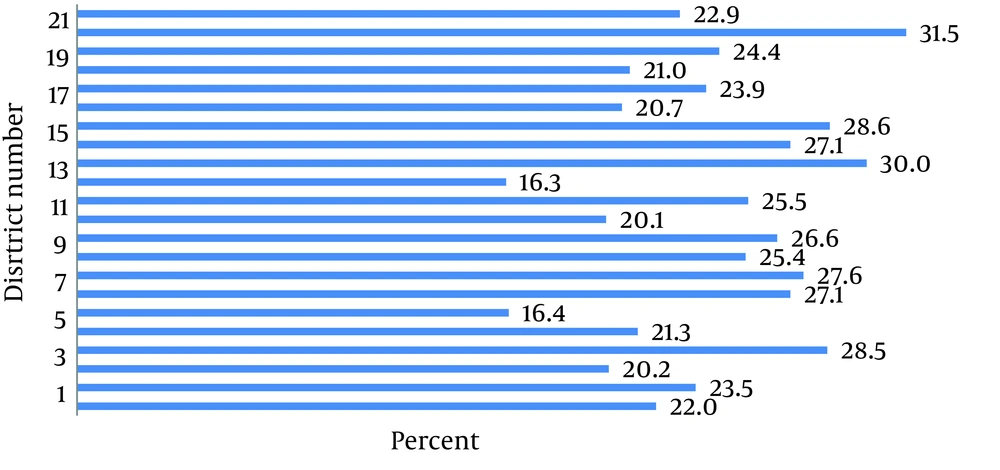
A significant difference was found in the prevalence of chronic pain between districts of Tehran (χ2 = 226.3, P < 0.001). The prevalence of chronic pain in any district of Tehran is presented in Figure 3.
Also, the prevalence of chronic pain types in districts of Tehran is presented in Table 2. District 21 had the first rank related to the prevalence of 5 chronic pain types and district 4 had the first rank related to the prevalence of 2 chronic pain types (the cells which marked with gray color).
| District | Chronic Pain | ||||||
|---|---|---|---|---|---|---|---|
| Low back | Neck | Shoulder | Knee | Upper Limp | Lower Limp | Headache | |
| 1 | 10.2 | 5.0 | 4.3 | 9.7 | 3.1 | 3.8 | 4.8 |
| 2 | 11.6 | 4.8 | 4.7 | 12.5 | 3.2 | 4.2 | 5.5 |
| 3 | 8.1 | 3.7 | 3.0 | 8.6 | 2.0 | 2.2 | 6.8 |
| 4 | 15.8 | 6.6 | 5.7 | 12.0 | 4.8 | 5.6 | 9.0 |
| 5 | 11.1 | 4.8 | 4.4 | 10.2 | 2.2 | 2.5 | 5.8 |
| 6 | 9.2 | 4.3 | 4.3 | 7.6 | 2.9 | 3.0 | 4.1 |
| 7 | 13.2 | 7.0 | 5.3 | 12.2 | 3.3 | 4.2 | 8.3 |
| 8 | 14.0 | 6.8 | 6.9 | 15.2 | 4.0 | 5.2 | 6.9 |
| 9 | 12.9 | 5.7 | 4.0 | 13.5 | 4.5 | 5.1 | 6.9 |
| 10 | 13.6 | 6.2 | 4.3 | 10.7 | 3.1 | 3.7 | 7.0 |
| 11 | 11.2 | 5.0 | 4.4 | 8.7 | 1.9 | 4.2 | 5.3 |
| 12 | 12.3 | 4.5 | 5.4 | 13.3 | 4.7 | 5.1 | 4.9 |
| 13 | 8.4 | 3.2 | 3.3 | 8.8 | 2.9 | 2.7 | 4.2 |
| 14 | 16.8 | 6.1 | 6.0 | 14.5 | 3.7 | 5.1 | 9.4 |
| 15 | 13.5 | 6.3 | 6.2 | 12.1 | 3.1 | 4.2 | 8.3 |
| 16 | 14.6 | 4.6 | 5.1 | 12.6 | 2.7 | 2.6 | 10.1 |
| 17 | 10.8 | 4.0 | 4.7 | 9.1 | 3.1 | 3.9 | 6.0 |
| 18 | 11.7 | 5.2 | 3.2 | 9.9 | 3.1 | 3.3 | 7.9 |
| 19 | 9.4 | 4.2 | 3.8 | 8.9 | 2.9 | 2.6 | 5.3 |
| 20 | 12.8 | 7.7 | 5.6 | 11.5 | 4.0 | 4.7 | 7.8 |
| 21 | 19.3 | 8.7 | 7.9 | 15.6 | 3.8 | 5.0 | 11.5 |
| 22 | 13.4 | 4.8 | 4.7 | 11.6 | 2.5 | 4.0 | 5.1 |
| X2 | 155.9 | 79.5 | 69.6 | 116.6 | 45.6 | 61.8 | 138.1 |
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.001 | < 0.001 | < 0.001 |
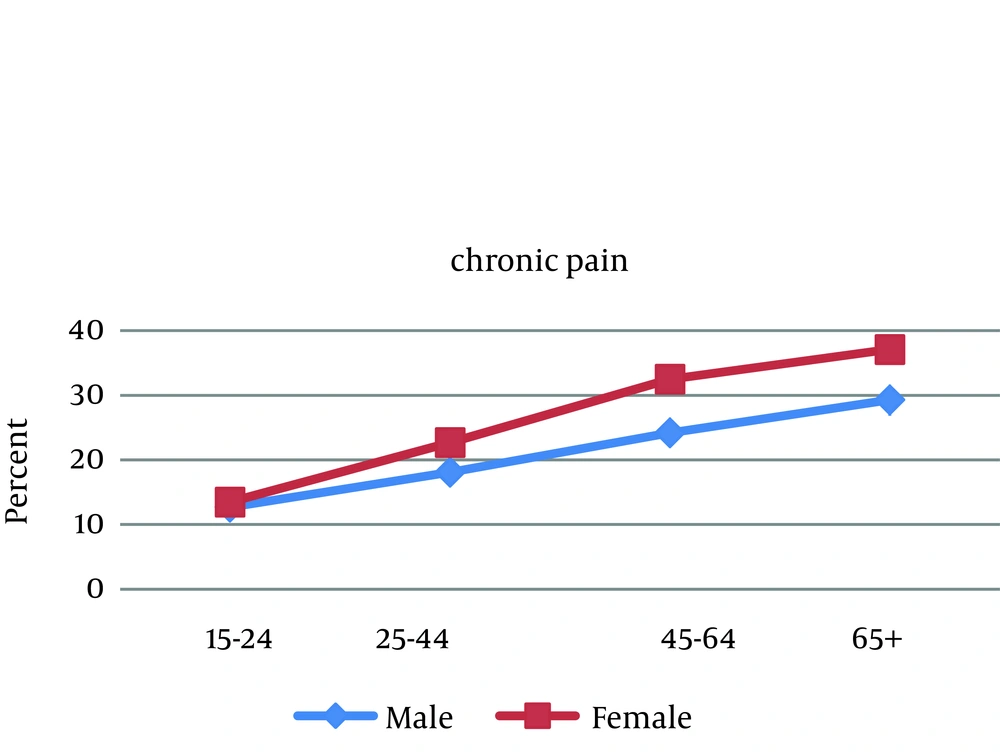
The results of this study showed a significant difference in chronic pain prevalence between the two sexes (χ2 = 68.7, P < 0.001). Women of all ages had a higher prevalence of chronic pain (The differences range: 1.6 % - 10.2%). There was almost an upward trend in pattern of chronic pain prevalence for both male and female sexes (Figure 4). This pattern was seen in all types of chronic pain; however, headache was an exception. Chronic headache had an upward trend until 64 years old and decreased after that. We didn’t show the figure of it here.
4.3. Interference of Chronic Pain in Daily Life
In this study, 87.2% of women and 88.3% of men with chronic pain expressed that pain created some degree of impairment in their daily life.
4.4. Health Characteristics by Chronic Pain Sufferers and People Without Chronic Pain
There was a significantly higher percentage of poor self-assessment of general health of all types of chronic pain sufferers compared to people without chronic pain (P < 0.001).
Moreover, the results showed that the prevalence of anxiety and depression in patients with chronic pain was significantly higher than in individuals without chronic pain (50.5% versus 35.1% and 42.8 versus 34.1%, respectively, P < 0.001).
4.5. Lifestyle Characteristics of Chronic Pain Sufferers
Higher levels of satisfaction with household income caused lower prevalence of chronic pain (P < 0.001). Moreover, people with chronic pain significantly suffered catastrophic expenditures more than people without chronic pain (11.1% versus 8.0%, P < 0.001).
4.6. Association Between Chronic Pain and Independent Variables by Type of Pain
Any association between any type of chronic pain and independent variables was determined using multiple logistic regressions (Table 3). Anxiety and age were risk factors associated with all types of chronic pain.
| Type of Pain | Low Back | Neck | Knee | Shoulder | Upper Limb | Lower Limb | Headache | ||
|---|---|---|---|---|---|---|---|---|---|
| Gender | |||||||||
| Male | 0.84 (0.73- 0.96) | 0.71 (0.58- 0.87) | 0.81 (0.71- 0.94) | 0.80 (0.65- 0.98) | 0.91 (0.70- 1.18) | 0.89 (0.70- 1.12) | 0.91 (0.76- 1.09) | ||
| Female | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Age group, y | |||||||||
| 15-24 | 0.39 (0.30- 0.50) | 0.30 (0.21- 0.45) | 0.25 (0.19- 0.33) | 0.30 (0.20- 0.44) | 0.51 (0.32- 0.82) | 0.26 (0.16- 0.40) | 0.95 (0.69- 1.30) | ||
| 25-44 | 0.62 (0.54- 0.73) | 0.54 (0.43- 0.66) | 0.39 (0.34- 0.46) | 0.51 (0.41- 0.64) | 0.59 (0.45- 0.78) | 0.39 (0.31- 0.50) | 1.32 (1.07- 1.63) | ||
| 45-64 | 0.84 (0.77- 0.95) | 0.89 (0.75- 1.07) | 0.74 (0.65- 0.84) | 0.85 (0.71- 1.02) | 0.84 (0.67- 1.05) | 0.60 (0.50- 0.73) | 1.18 (0.98- 1.42) | ||
| ≤ 65 | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Education | |||||||||
| Illiterate | 1.46 (1.22- 1.74) | 1.17 (0.91- 1.50) | 1.78 (1.49- 2.12) | 1.55 (1.21- 2.00) | 1.59 (1.16- 2.19) | 1.46 (1.10- 1.94) | 1.86 (1.47- 2.34) | ||
| Primary and secondary | 1.38 (1.21- 1.57) | 1.20 (0.99- 1.45) | 1.42 (1.23- 1.63) | 1.27 (1.04- 1.56) | 1.52 (1.18- 1.96) | 1.47 (1.17- 1.84) | 1.32 (1.11- 1.57) | ||
| High school | 1.19 (1.06- 1.34) | 1.05 (0.89- 1.24) | 1.16 (1.03- 1.32) | 1.09 (0.91- 1.31) | 1.27 (1.01- 1.60) | 1.13 (0.92- 1.39) | 1.25 (1.07- 1.44) | ||
| College education | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Occupational status | |||||||||
| Unemployed (looking for work) | 0.97 (0.78- 1.21) | 0.74 (0.53- 1.05) | 1.03 (0.82- 1.29) | 0.97 (0.69- 1.36) | 0.83 (0.53- 1.31) | 1.03 (0.72- 1.49) | 1.05 (0.79- 1.38) | ||
| Housewife | 1.31 (1.11- 1.53) | 1.17 (0.93- 1.48) | 1.26 (1.06- 1.49) | 1.21 (0.95- 1.55) | 1.37 (1.01- 1.85) | 1.17 (0.89- 1.54) | 1.34 (1.09- 1.64) | ||
| Student | 1.00 (0.76- 1.32) | 0.10 (0.67- 1.49) | 1.23 (0.93- 1.64) | 1.29 (0.86- 1.95) | 1.13 (0.66- 1.92) | 1.02 (0.62- 1.67) | 1.51 (1.11- 2.06) | ||
| Have income without work | 0.96 (0.70- 1.31) | 1.14 (0.75- 1.73) | 0.92 (0.67- 1.26) | 0.96 (0.61- 1.51) | 1.25 (0.78- 2.10) | 1.16 (0.74- 1.84) | 1.05 (0.69- 1.59) | ||
| Retiree and pensioner | 1.22 (1.05- 1.41) | 1.20 (0.97- 1.49) | 1.18 (1.01- 1.37) | 1.26 (1.01- 1.58) | 1.28 (0.97- 1.69) | 1.27 (0.99- 1.61) | 1.31 (1.07- 1.61) | ||
| Employed | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Marital status | |||||||||
| Widowed | 1.05 (0.91- 1.23) | 0.98 (0.79- 1.20) | 1.10 (0.95- 1.28) | 1.09 (0.89- 1.35) | 0.95 (0.73- 1.24) | 0.97 (0.76- 1.22) | 0.96 (0.78- 1.19) | ||
| Divorced | 0.95 (0.71- 1.27) | 1.11 (0.76- 1.63) | 1.11 (0.83- 1.48) | 1.03 (0.68- 1.57) | 1.13 (0.70- 1.83) | 1.06 (0.67- 1.68) | 1.08 (0.76- 1.53) | ||
| Single | 0.75 (0.62- 0.93) | 1.07 (0.82- 1.38) | 0.99 (0.82- 1.20) | 1.08 (0.82- 1.42) | 0.74 (0.51- 1.07) | 1.00 (0.73- 1.38) | 0.69 (0.55- 0.88) | ||
| Married | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Depression | |||||||||
| Yes | 1.07 (0.98- 1.17) | 1.18 (1.04- 1.35) | 1.12 (1.02- 1.23) | 1.23 (1.07- 1.41) | 1.36 (1.16- 1.61) | 1.29 (1.11- 1.50) | 1.40 (1.25- 1.58) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Anxiety | |||||||||
| Yes | 1.82 (1.67- 2.00) | 2.11 (1.86- 2.42) | 1.70 (1.55- 1.87) | 2.43 (2.11- 2.80) | 2.26 (1.93- 2.63) | 2.38 (2.01- 2.82) | 2.03 (1.80- 2.28) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Obesity | |||||||||
| Yes | 1.17 (1.05- 1.30) | 1.03 (0.89- 1.20) | 1.15 (1.03- 1.28) | 1.03 (0.89- 1.22) | 1.30 (1.10- 1.54) | 1.18 (0.98- 1.42) | 1.08 (0.94- 1.24) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Satisfaction of household income | |||||||||
| None | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Somewhat | 0.87 (0.80- 0.95) | 0.84 (0.74- 0.95) | 0.83 (0.76- 0.91) | 0.88 (0.77- 0.99) | 0.81 (0.70- 0.94) | 0.79 (0.67- 0.92) | 0.88 (0.79- 0.98) | ||
| Quiet | 0.75 (0.63- 0.89) | 0.77 (0.59- 0.99) | 0.68 (0.56- 0.82) | 0.75 (0.56- 0.98) | 0.68 (0.56- 0.82) | 0.69 (0.48- 0.98) | 0.89 (0.71- 1.11) | ||
| Smoking | |||||||||
| Yes | 1.10 (1.00- 1.22) | 1.09 (0.96- 1.26) | 1.09 (0.98- 1.20) | 1.05 (0.91- 1.22) | 1.15 (0.98- 1.35) | 1.08 (0.90- 1.28) | 1.18 (1.05- 1.34) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Diabetes Mellitus | |||||||||
| Yes | 1.35 (1.17- 1.56) | 1.47 (1.22- 1.79) | 1.32 (1.15- 1.53) | 1.60 (1.31- 1.94) | 1.27 (1.01- 1.58) | 1.47 (1.16- 1.86) | 1.10 (0.89- 1.35) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Cancer | |||||||||
| Yes | 1.14 (0.69- 1.86) | 1.24 (0.65- 2.36) | 1.31 (0.81- 2.12) | 1.20 (0.61- 2.35) | 1.31 (0.81- 2.12) | 1.31 (0.81- 2.12) | 1.60 (0.90- 2.86) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Exercise | |||||||||
| Yes | 0.97 (0.88- 1.06) | 0.83 (0.73- 0.95) | 0.93 (0.85- 1.03) | 0.90 (0.78- 1.03) | 0.93 (0.85- 1.03) | 0.77 (0.64- 0.92) | 0.93 (0.82- 1.04) | ||
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
a Data are presented as OR (95% CI).
5. Discussion
This study describes the prevalence and risk factors of chronic pain types in Tehran. The motivation of this study was providing epidemiological information about chronic pain types. Having a large enough sample size to investigate the relationship between risk factors and chronic pain types can be considered as an important feature of this study.
The prevalence of chronic pain among adults of Tehran was 24%, which compared to some developed countries was higher than Canada (18.9%) (11), similar to Norway (24%) (7) and lower than the United States (30.7%) (12). Also, it was lower compared to some developing countries such as Brazil (42%) (13) and Nepal (47%) (14).
In this study, low back pain and knee pain were the most frequent types of chronic pain, which is similar to some studies (12, 15).
District 21 had the first rank related to the prevalence of 5 chronic pain types (lower back, neck, shoulder, knee and headache) and district 4 had the first rank related to the prevalence of 2 chronic pain types (lower limb and upper limb). So, these districts need more consideration.
Based on the multivariate logistic regression results, the gender difference is found in the prevalence of all types of chronic pain and female gender was associated with more types of pain, although the difference was not statistically significant for lower limb, upper limb and headache. These findings are in accordance with those of similar studies (16, 17). A possible explanation for this may be relevant to sociological, cultural and physical differences (17).
Consistent with other studies (18, 19), we found the prevalence of all types of chronic pain is an ascendant function of age exception chronic headache. Chronic headache had an upward trend until 64 years old, but the prevalence of it decreased after that (peaking between 25 and 64 years). These findings are similar to the findings of studies conducted by Lipton et al. (20). This might be likely as a result of reduction of physical activity level, interpersonal relationships, and social activities (e.g. working and recreation) because of increasing age (21).
In general, lower educational level was associated with a greater risk factor for all chronic pain types, which support prior studies (16, 21). High education levels make adequate preparation to obtain information. Individuals with high education levels have more awareness about application of accessing health resources to alleviate and control their pain problems. Those healthy individuals might use such resources to keep up their health status. Furthermore, they could have significantly more possibilities to acquire extra information on health issues (21).
Anxiety was another statistically significant predictor for all types of chronic pain. Anxious individuals suffered from more pain. This was true for depression variable, although it was not statistically significant for chronic low back pain. Physical pain is one of the problems in people with anxiety and/or depressive disorders (22). The relationship between pain, depression and anxiety could be, somewhat, explained through “activation of the sympathetic nervous system, the involvement of the hypothalamic-pituitary-axis, and down-regulation of benzodiazepine receptors in the frontal cortex” (23).
We also found an association between obesity and chronic pain in lower back, knee and lower limb. These findings support prior researches conducted by Webb et al. (24) Miranda et al. (19) and Jannini et al. (25). The correlation between obesity and low back pain may be explained through inflammatory mechanisms (26). Obesity may also be a risk factor for bone and joint disorders and have a severe influence on “soft tissue structures, fascia, and the cartilage” (27). Furthermore, it is assumed that being overweight is a risk factor for osteoarthritis in the knees, hips and feet as weight bearing joints. It is claimed this trend can also be extended to the spinal joints too (28).
Another important finding was that being housewife is associated with the higher odds for suffering from chronic pain in lower back, knee and headache. Also, retired or pensioners participants were more likely to report chronic pain in lower back, knee, shoulder, upper limb and headache compared to the employed participants. This finding is consistent with research showing that the prevalence of chronic pain is typically higher among housewives and retirees or pensioners (29, 30). It seems possible that these results are due to a higher rate of mental disorders between housewives and retirees, according to a number of studies (31). Feeling of uselessness can be created and increased as a consequence of being at home most of the time and doing repetitive work by housewives (32).
Our findings in this study showed a higher prevalence of chronic headache in students. Recurrent headache is really a frequent problem in school children (33) and among university students (34). A contributing factor for chronic tension-type headache is stress (35) and different types of stressors including the pressure of academics with an obligation of success, uncertain future and problems envisaged for integration into the system is subjected in a student’s life (36).
Similar to the study by Biglarian et al. (37), we observed that the prevalence of chronic headache and chronic low back pain was less common in single individuals compared to married people. This outcome may be related to higher prevalence rates of mental disorders in married people in Iran as a reason of “economic and social stress factors such as financial matters family management and child care” (31). The comorbidity of a psychiatric disorder and tension-type headache and migraine has been confirmed by Tan et al. (38).
We observed smokers were more likely to experience low back pain and headache, a finding that is in accordance with other studies (30, 37). The association between smoking and chronic low back pain may be related to nicotine’s effect on the central nervous system which affects on an elevated understanding of pain (39). Also, the connection between carbon monoxide intoxication and headache has been recognized (40).
Satisfaction of household’s income was another important risk factor for all types of chronic pain, although it is not statistically significant for chronic neck pain. It seems income is a crucial social element of health. The overall shape of living condition, psychological functioning, and health-related behaviors such as quality of diet, level of physical activity, tobacco use, and exorbitant alcohol use might be affected by level of income. Further, there is a high correlation between level of education as one of the affecting factors on pain incidence and level of income (41).
Our data further showed that chronic pain is generally more prevalent in patients with diabetes (42). There was no statistically significant difference in chronic headache pain between persons with diabetes and persons without diabetes. The reasons can be presented as follows: a) A common complaint among diabetic patients is chronic pain which may be associated with reduced physical activity tolerance (8) b) Among those with known diabetes mellitus, anxiety and other psychological factors may influence their response to the questions about pain. c) It is possible this thought arises in diabetic patients that attempts to keep the glucose level low might affect the incidence of chronic pain (43).
In this study cancer was significantly associated with chronic upper limb pain. Tumor in the apex of the lung, axilla, or lower neck can be considered as reasons for upper limb pain in cancer patients (44).
Our results indicated lack of exercise is another risk factor for more suffering from chronic pain in upper limb and lower limb. Evidence shows that good results can be achieved through exercise in people with neck and upper limb pain (45). Moreover, exercise programs might be effective for hip and knee problems based on results of studies concerning lower limb treatment (46).