1. Background
Clinical symptoms of inhalation exposure to formaldehyde (FA) include eye, nose, and upper-respiratory irritation, aggravate pre-existing asthma, and depressed lung function activities (1, 2). FA is a genotoxic chemical that can cause squamous cancer of the nasal passages and cancer of nasopharyngeal regions (3). International Agency for Research on Cancer (IARC) classified FA as ‘human carcinogen’ (group 1) (4). FA is also an endogenous compound produced in cells and excreted through exhaled breath (5).
The U.S. Occupational Safety Health Administration (OSHA) has established the permissible exposure limit (PEL) for airborne FA at a value of 0.75 parts per million (8 h time-weighted average (TWA)); the short-term (15 min) exposure limit (STEL) is 2 ppm. The National Institute of Occupational Safety and Health (NIOSH) has also presented PEL of 0.016 ppm (8 h TWA) and 0.1 ppm (STEL). American regulating authorities require the individuals having higher exposure to use proper respirators (6).
Concerns have been raised regarding the health of employees and students exposed to FA in the anatomy laboratories due to the vapors emitted during the dissection of cadavers in producing complaints as: unpleasant odor (68%), cough (64%), sore throat and runny nose (56%), nasal irritation and itching (52%), and eye irritation (48%) (7). However, the effects of chronic exposure of FA could be more severe than respiratory symptoms and recently higher incidence of amyotrophic lateral sclerosis (ALS) was reported as the result of FA (8). Occupational monitoring of anatomy laboratory workers to FA in the various university anatomy theaters has been reported to be a health concern; more stringent evaluations and controls in the form of a lateral exhaust ventilation system for the dissection tables and personal protective equipment were requested (9).
Generally, biological monitoring is an accurate evaluation of occupational exposure to volatile organic compounds (10). Due to the difficulties and disadvantages of blood and urine sampling, recent approaches for assessing occupational and environmental exposure to several chemicals as well as biological monitoring have focused on exhaled breath (11, 12). There is no commonly accepted method for biological monitoring for FA (13). Several factors, including the skin absorption, age-related differences in individual uptake, behaviors of workers, poor personnel work practice, the effectiveness of personal protective equipment (PPE), and the workload will probably influence personal sampling in workplaces. Biological monitoring has been traditionally recommended as the complementary method in the evaluation of the chemical exposures (14). However, this approach is changing and biological monitoring is recommended for hazardous chemicals as the method of choice for monitoring exposure and health risk assessment (15). There are several attempts for biological monitoring of FA such as: exploring DNA-protein cross-links in workers exposed to FA (16) and sister chromatid exchange rate in the personnel with exposure to FA in the range of 0.04 to 6.9 ppm (17). In clinical monitoring of cancer patients and cigarette smokers, FA was measured in their exhaled breath (12, 18).
The results of toxicokinetic studies indicated that inhaled FA absorption in humans occurs primarily at the site of entry. The site of absorption of FA from the respiratory tract depends on a number of factors, including airway anatomy, breathing pattern, and ventilation rate (19). According to some studies, the half-life of circulating FA in the bloodstream, upon the absorption in the respiratory tract is reported about 1 minute (20). Generally, it is reported that Inhaled FA rapidly biotransforms to formate (13, 21-23). Thus, FA, in exhaled breath has been reported in the range of a few parts per billion concentrations, however, the validity of measurement methods was reported questionable (21).
2. Objectives
Due to the toxicity of FA and the absence of any reliable biological monitoring for FA, the objective of this study was to explore the feasibility of biological monitoring of exposed anatomy staff through the analysis of unchanged FA in their exhaled breath.
3. Methods
This study was conducted at an anatomy theater of an Iranian medical school during early winter. The doors of the theater were closed when the theater was not in use. The inclusion criteria for this study were: the healthy, nonsmoking population with at least one year of work history. The participants of this study included 20 anatomy staff exposed to FA and 20 library staff for checking the residual concentration of FA in the exhaled breath of non-exposed working population. Upon approval of the proposal by the Shahid Beheshti University of Medical Sciences, written consent of all participants was received according to an ethics committee form. The authors of this study observed all safety precautions during their sampling and laboratory practices.
The anatomy theater was just equipped with a general ventilation system. There were also no local ventilation systems for dissection tables. The ventilation system of the theater was off the entire time during the winter. In this study, cadavers were placed on the tables. Dissection sessions usually last for two hours.
In order to investigate the relationship between the concentration of FA in the air with its concentration in exhaled breath, demographic data such as age, work hours, work experience, and health status as well as using personal protective equipment were investigated by face-to-face interview.
Personal exposure monitoring of participants who did not use any personal protective equipment was conducted according to the method presented by NIOSH method No. 2016 (24). The personal sampling was done with a flow rate of 0.1 lit/min for the period of 2 hours using sorbent tubes (SKC Inc., USA) (silica gel coated with 2, 4 Dinitrophenylhydrazine catalog No. 119-226). Absorbed FA on the coated silica gel was extracted with HPLC grade acetonitrile (Merck Co., Germany) and analyzed by Merck-Hitachi high-performance liquid chromatography (HPLC) model D-7000 equipped with ultraviolet (UV) detector set at 360 nm. The mobile phase consisted of 45% acetonitrile and 55% water, and an injection volume of 20 µL, and stainless steel column packed with 5 μm C-18 (Merck KGaA, Germany). A blank was collected for each set of sampling.
Before collecting the exhaled breath for biological monitoring, all of the subjects’ lungs were washed via inhalation of clean ambient air with trace FA concentration below the detection limit (23 µg/m3) for 10 minutes. Having completed the lung wash, exhaled breath was subsequently collected in prewashed 5 liters Tedlar bags while breathing clean air. Within 2 hours after exhaling breath sampling, four liters of exhaled breath was passed through silica gel sorbent tubes coated with dinitrophenylhydrazine (DNPH) via a pump with a flow rate of about 0.1 lit/min. Absorbed FA from exhaled breath on coated silica gel was extracted and analyzed the same as described earlier for personal samples.
The merits of the method for sampling and analysis of FA in the breathing zone, including precision (inter-day and intra-day coefficient of variations), recovery, linear range concentrations, limit of detection (LoD) and limit of quantitation (LoQ) were examined according to the method described by Mitra (25).
For examining the association between inhalation and exhalation FA in anatomy’s staff, the SPSS version 18.0 software (SPSS, Chicago, IL, USA) and Pearson correlation statistical test were used.
4. Results
The mean (± SD) of age and work history of anatomy staff was 41.5 ± 0.46, 15 ± 0.36 years, respectively.
Linear range concentration of FA analysis in breathing zone was 300 µg/m3 - 8 mg/m3 (r2 = 0.998). The inter-day CV for FA samples ranged from 1.65% to 6.51% and intra-day CV ranged from 0.84% to 4.31%. The recovery from FA samples ranged from 100 ± 0.87% to 100 ± 7%. LoD and LoQ for the analytical method were 23 and 77.5 as µg/m3, respectively.
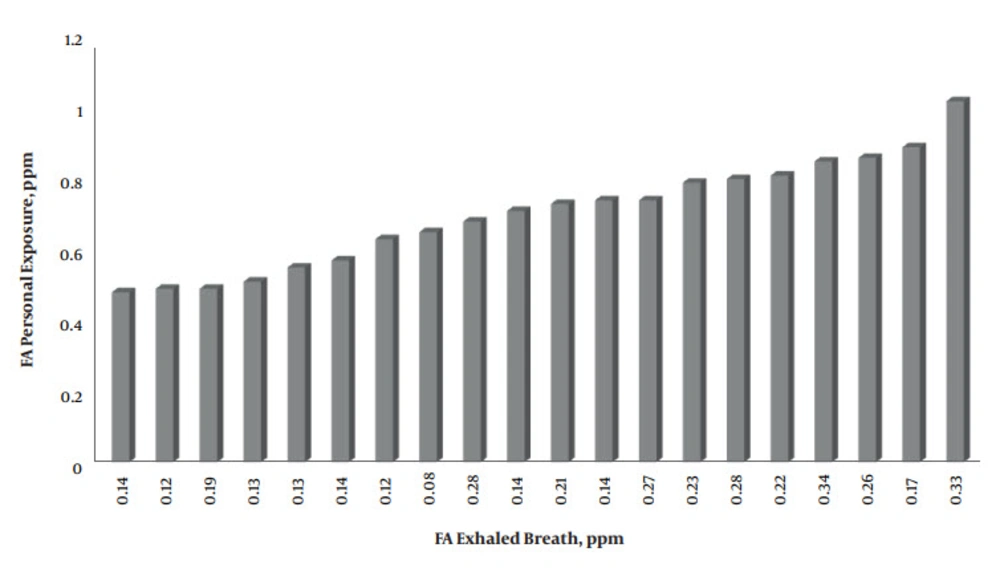
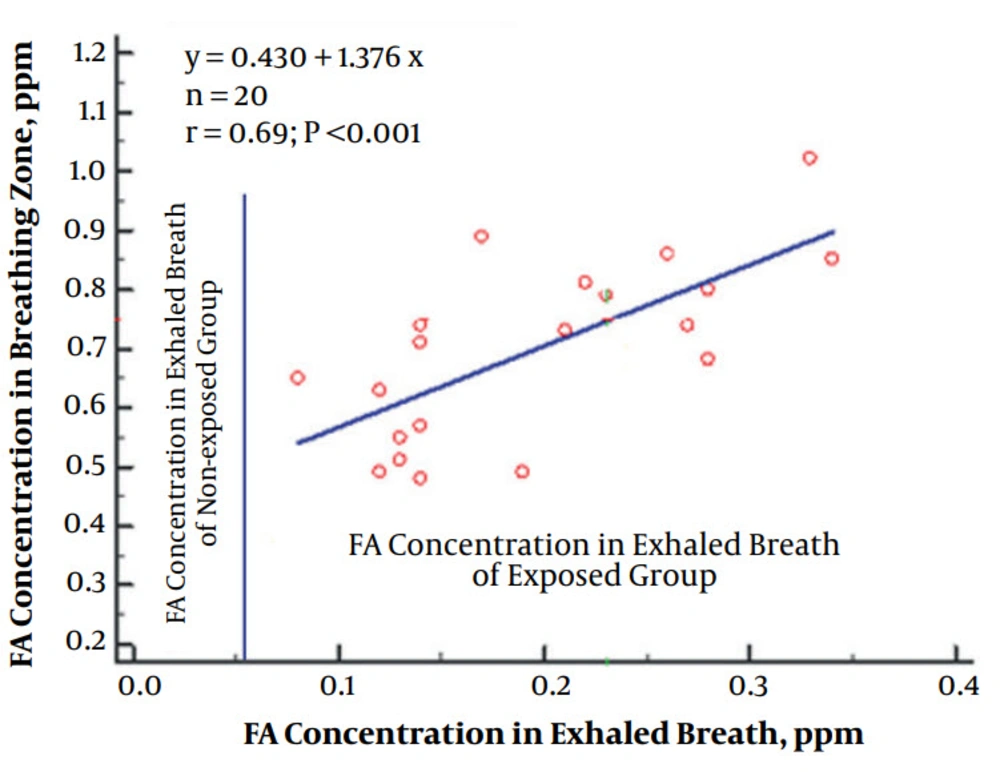
The average of FA exposure and the average FA concentration in the exhaled breath of the anatomy’s staff were 698 ± 34 and 195 ± 17 as ppb, respectively (Figure 1). The average residual FA in the exhaled breath of non-exposed librarian was 52 ppb. The positive Pearson statistical significant correlation of occupational exposure of the anatomy’s staff with concentrations of FA in their exhaled breath was demonstrated (R square = 0.478 and P < 0.001 (Figure 2).
5. Discussion
According to the results of this study, exposure of 35% of the anatomy personnel was higher than OSHA’s PEL (PEL-TWA = 750 ppb) (22). Generally, anatomy’s staff exposures in this study were almost identical to their colleagues in other countries such as Japan and Portugal (26, 27).
Some authors have expressed doubts in measuring appreciable amounts of FA in exhaled breath (23). However, in studies have reported residual FA in the exhaled breath, which was in agreement with the concentration of FA in the exhaled breath of healthy unexposed librarians in this study (11, 28). Generally, FA in exhaled breath might be due to diet, indoor air pollutants, and FA emitted from wood products (28, 29). Ebelera et al. in their study also demonstrated high concentration of FA in the cancer patient and healthy subjects in the range of 0.42 - 1.2 and 0.3 - 0.6 as ppm, respectively (30). However, other authors reported a lesser amount of FA in the exhaled breath of healthy subjects than the prior study (18, 28).
Despite all diverse results presented by the authors in this study regarding the concentration range of FA in exhaled breath, the authors of this study believe that the reason behind the conflicting results might be due to the hardship of its sampling and analysis of FA. Therefore, considering the task of validation processes of the NIOSH method No. 2016 locally in this study and statistically significant positive correlation between FA concentrations in breathing zone and FA concentrations in exhaled breath of healthy exposed subjects, measurement of FA in the exhaled breath as biomarker of exposure in healthy and non-smokers workers seemed feasible in this study. Generally, established biomarkers of exposure of FA through measuring DNA adducts and sister chromatid exchange rate in blood samples, are more complex than measuring FA through exhaled breath samples (16, 17). The method presented in this study does not require invasive sampling and elaborate analysis. However, due to the limited number of exposed in this study, a more comprehensive study is proposed.
Occupational exposure to FA could endanger the health of anatomy’s staff. A new method proposed for biological monitoring of exposed population through exhaled breath could provide an alternative monitoring. However, for definite and credible results, a more thorough study with a larger population with stringent measures for limiting confounding factors is recommended.