1. Background
In order to meet the needs of the community with regard to their mission over time and given the rapid pace of technological change, increased expectations of individuals to use the most recent and best technologies, increased service costs, resource shortages, dominance of the market economy over service providing organizations and its unpleasant effects on the health market as well as issues such as poverty and transition of diseases, the health systems undoubtedly require reforms (1, 2). All countries are actually seeking reforms and innovations in their health system in order to achieve a universal access to services, justice, quality, and fair payments in the system (3-5). On the other hand, 2 important features of health and treatment make the reforms inevitable in this sector. First, health is one of the individuals’ basic needs and rights and the other is the rapid pace of changes and transformations. The transformations in the appearance of diseases, evolution of health concepts, and the advancement of technology in terms of diagnosis, treatment, and provision of services indicate the fast speed of changes in health (6-9).
In this regard, one of the most recent reforms in the health system of the Islamic Republic of Iran is called “Health Transformation Plan (HTP)”. In accordance with its general duties, missions, and upstream documents, especially the 20-year vision document, health legislation in the 5th development plan and the 11th government program, the Ministry of Health and Medical Education, as the main custodian of the country’s health system, initiated the HSRP, in May 2014, with 3 approaches to financial protection of individuals, access to health services and improved quality of services (10-12). In spite of the short lifetime of this plan, several studies have investigated it from different perspectives. In their study, Heidarian and Vahdat (2015) stated that the plan has succeeded in reducing the patients’ out-of-pocket expenses in public hospitals located in Isfahan (Iran), therefore, the patients’ out-of-pocket expenses, after the implementation of the HSRP, decreased within the range of 23% to 64% (13). Rooeintan et al. (2016) assessed the impact of healthcare reform plan on the rate of vaginal delivery and caesarean section in Shiraz (Iran) and showed that healthcare reform has led to an increase in the number of vaginal deliveries in hospitals affiliated to Shiraz University of Medical Sciences (14). In addition, Faridfar et al. (2016) examined the effect of the HSRP on different types of clinical, paraclinical, surgical, and patient satisfaction indicators in Hazrat-e-Rasoul hospital in Tehran (Iran) and the results showed an increase in the frequency of admissions in clinics and paraclinics as well as in patient satisfaction (15).
Since hospitals are one of the largest and most important health service providers that play an important role in improving community health and also in view of the growing expenditures of health care, more attention to the hospitals` performance seems necessary (16-19).
The performance assessment of health care providers, including hospitals, can provide decision-makers with timely and relevant information related to the efficiency of these centers in order to monitor their status and current activities (20-22). This information informs the program managers and policymakers and would provide the grounds for monitoring the national goals and assessing relevant policies. Timely monitoring and evaluation of reforms can provide evidence to guide the more proper implementation of reforms (23, 24).
2. Objectives
Considering the vital role of monitoring and evaluation of each project in determining its effectiveness, this study aimed to evaluate the effect of the implementation of the HSRP on the performance indicators of teaching hospitals affiliated with Shiraz University of Medical Sciences in 2017. The findings can be implemented in planning, policy making, and reviewing the plan as well as in finding the most suitable executive solutions in this field. Therefore, in view of the general objectives of the health reform plan to increase the quantitative and qualitative services to patients in the hospital complex and also a need for a profound understanding of the evaluation ofthe mentioned plan by policymakers at the top of the decision making system and executive managers in hospitals for efficient use of limited resources and achieving the effectiveness ofthe results, this research can be used as an objective example applied by policymakers at different levels of implementation.
3. Methods
The present research was a descriptive-analytic study and longitudinally carried out in 10 teaching hospitals affiliated to Shiraz University of Medical Sciences in 2017. Regarding the implementation of the HSRP in all hospitals affiliated to the ministry of health since May 2014, some selected performance indicators were examined in the concerned hospitals. In order to evaluate the performance of the hospital, several indicators are used, among which the bed occupancy rate (BOR), bed turnover rate (BTR), and average length of stay (ALS) are the most important and most often-used indicators for assessing the hospital efficacy and have been used in well-known hospital performance measurement models such as Pabon and Lasso’s (25, 26).
The bed occupancy rate (BOR) is a measure of utilization of the available bed capacity. It indicates the percentage of beds occupied by patients in a defined period of time, usually a year. It is the amount of occupied beds, which is relative to the bed of the day to the active bed in a given period. The bed turnover interval for the average length of time (in days) that elapses between the discharge of one inpatient and the admission of the next inpatient to the same bed at specialty level/significant facility, over any period of time. The average length of stay (ALOS) is often used as an indicator of efficiency. All other things being equal, a shorter stay will reduce the cost per discharge and shift care from inpatient to less expensive post-acute settings. The ALOS refers to the average number of days that patients spend in the hospital (25).
In addition, some other indicators including inpatient to constructed beds ratio, frequency of patients admitted in the clinical and para clinical sectors, frequency of emergency, and elective operations and frequency of cesarean and normal delivery were also concerned since they reflect the performance of the hospitals.
The data gathering method was field data collection. Information was collected through referring to the existing records and documents prior to (2013) and after (2015) implementation of health reform plan. Thus, the statistical information needed for the study was collected by providing a registration form which its reliability was approved by 6 faculty members of Shiraz school of Management and Medical Informatics by referring to the hospital medical statistics department, each month, separately.
Regarding the ethical considerations, 1st a research letter was received from the vice-chancellor of Shiraz’ Management and Medical Informatics School and the letter of university preservation department received. Then, they were referred to each of the mentioned hospital’s management and after doing demanded coordination, necessary data were collected.
To analyze the data, Excel and SPSS software version 23, as well as descriptive statistics, frequency, and paired sample t-test were used (Regarding normal distribution of data). The level of significance was set at α = 0.05.
4. Results
With regard to the findings, the highest mean values for each of the indicators including BOR, inpatient to constructed beds ratio, BTR, ALS, patients admitted in the clinical and para clinical sectors, emergency and elective operations, as well as cesarean and normal delivery in 2013 were 75.07 in August, 0.77 in December, 2.24 in April, 4.64 in April, 2329.28 in December, 19130.57 in May, 211.5 in June, 575.75 in October, 290.5 in August, and 519 in September, respectively (Table 1).
| Indicator Month | BOR | Inpatient to Constructed Beds Ratio | BTR | ALSa | Patients Admitted in Clinical Sectors | Patients Admitted in Para Clinical Sectors | Emergency Operations | Elective Operations | Cesarean Delivery | Normal Delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| April | 65.16 | 0.72 | 2.24 | 4.64 | 1766 | 15718.85 | 188.17 | 289.37 | 245.5 | 349 |
| May | 72.87 | 0.73 | 1.21 | 4.21 | 1984.42 | 19130.57 | 203 | 561.5 | 231.5 | 379.5 |
| June | 74.43 | 0.74 | 1.01 | 4.12 | 2038.14 | 18783.42 | 211.5 | 505 | 257 | 400.5 |
| July | 72.98 | 0.74 | 1.24 | 4.36 | 2225 | 18490.42 | 210.5 | 575 | 288 | 506.5 |
| August | 75.07 | 0.75 | 1.05 | 4.17 | 2237.85 | 17677 | 208.34 | 549.37 | 290.5 | 491.5 |
| September | 74.07 | 0.76 | 1.06 | 4.33 | 2281.42 | 18013.14 | 154.84 | 574.5 | 275 | 519 |
| October | 74.87 | 0.76 | 1.12 | 4.29 | 2171.28 | 17917.42 | 203.5 | 578.75 | 262 | 440.5 |
| November | 72.86 | 0.76 | 1.32 | 4.26 | 2060.42 | 17292.14 | 196.67 | 545 | 244 | 458.5 |
| December | 73.43 | 0.77 | 1.18 | 4.23 | 2329.28 | 18270.28 | 200.34 | 522.62 | 282 | 467 |
| January | 70.85 | 0.77 | 1.27 | 4.12 | 2028.42 | 17780.85 | 128.67 | 506.5 | 270.5 | 428.5 |
| February | 72.26 | 0.75 | 1.19 | 3.99 | 2116.14 | 17812.28 | 182.5 | 543.25 | 278.5 | 454 |
| March | 73.66 | 0.75 | 1.30 | 3.93 | 2087.57 | 16987.42 | 182.16 | 464.62 | 243 | 424.5 |
aOne of the reasons for the high average length of stay is the long-term stay of patients in Ibn Sina psychiatric hospital.
Further, the highest mean values for each of the indicators including BOR, inpatient to constructed beds ratio, BTR, ALS, patients admitted in the clinical and para clinical sectors, emergency and elective operations, and cesarean and normal delivery in 2015 following the implementation of the HSRP were related to November (89.15), December and January (0.81), April (1.66), December (5.95), January (2929.28), January (22755.42), July (237.83), September (719. 12), August (437), and July (631.5) (Table 2).
| Indicator Month | BOR | Inpatient to Constructed Beds Ratio | BTR | ALSa | Patients Admitted in Clinical Sectors | Patients Admitted in Para Clinical sectors | Emergency Operations | Elective Operations | Cesarean Delivery | Normal Delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| April | 72.69 | 0.75 | 1.66 | 4.83 | 2096.28 | 18842.28 | 219.67 | 419.27 | 319 | 474.5 |
| May | 80.97 | 0.76 | 1.03 | 5.27 | 2437.14 | 21722.71 | 220.83 | 651.5 | 336.5 | 557 |
| June | 81.15 | 0.77 | 1.01 | 5.38 | 2479.71 | 22305.71 | 239 | 679.25 | 368.5 | 560 |
| July | 82.03 | 0.77 | 0.93 | 5.39 | 2478.28 | 22381.42 | 237.83 | 673.5 | 393 | 631.5 |
| August | 84.75 | 0.79 | 0.79 | 5.36 | 2538.14 | 22734.85 | 230.5 | 697.5 | 437 | 603.5 |
| September | 82.73 | 0.80 | 1.07 | 5.55 | 2538.85 | 22693.85 | 203.67 | 719.12 | 396.5 | 526.5 |
| October | 81.92 | 0.80 | 0.95 | 5.85 | 2516 | 21443.57 | 226.5 | 637 | 324 | 516.5 |
| November | 89.15 | 0.80 | 1.04 | 5.75 | 2542.71 | 21389 | 190.83 | 660.12 | 344 | 483 |
| December | 80.33 | 0.81 | 1.09 | 5.95 | 2795.14 | 21840.42 | 181.5 | 649.75 | 360.5 | 479.5 |
| January | 81.56 | 0.81 | 1.07 | 5.52 | 2929.28 | 22755.42 | 148.84 | 690.87 | 342.5 | 460.5 |
| February | 79.63 | 0.79 | 1.13 | 5.31 | 2729 | 22301.42 | 201.5 | 616.87 | 346 | 509 |
| March | 79.75 | 0.79 | 1.01 | 5.03 | 2458.85 | 21510.28 | 200.5 | 557.75 | 293 | 442 |
aOne of the reasons for the high average length of stay is the long-term stay of patients in Ibn Sina psychiatric hospital.
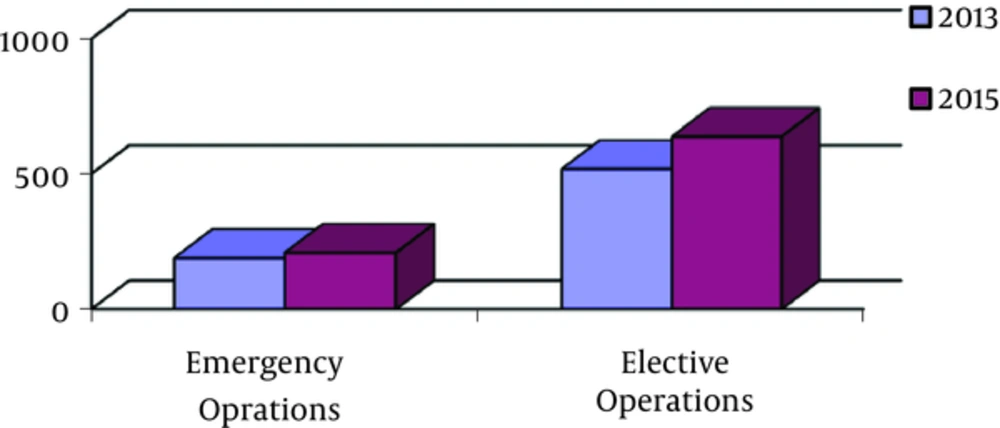
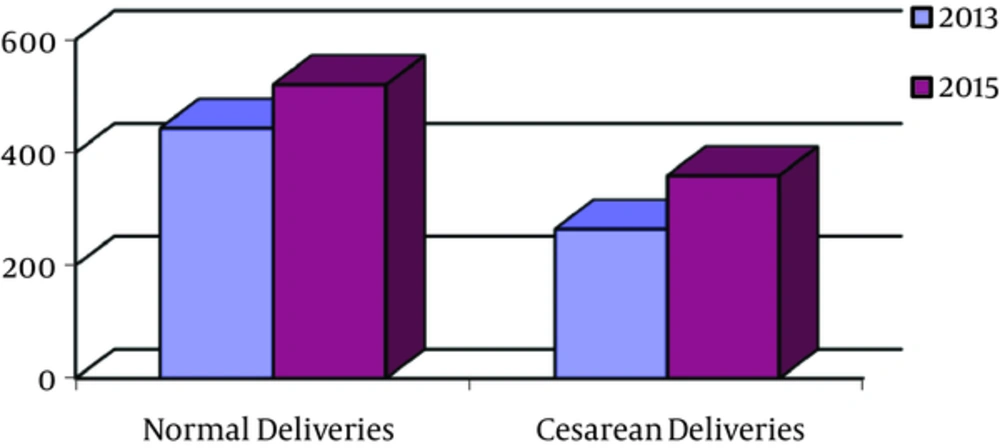
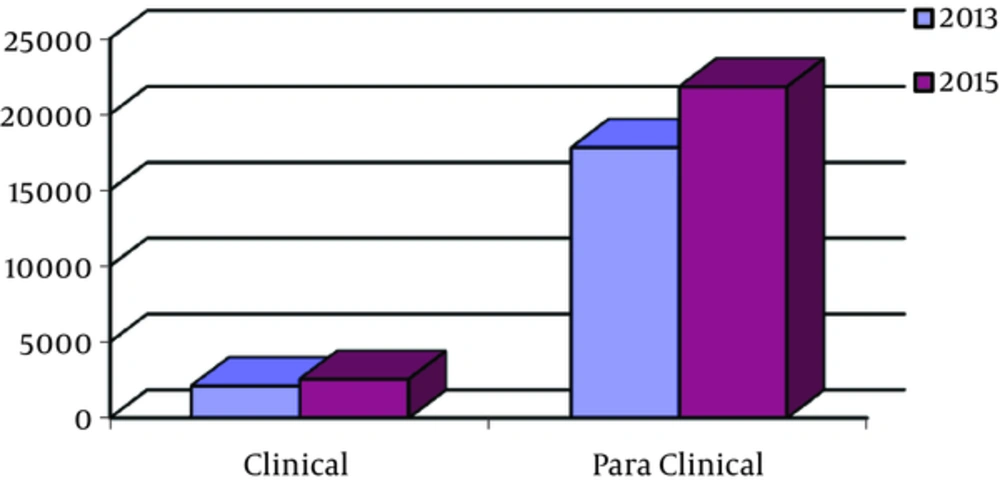
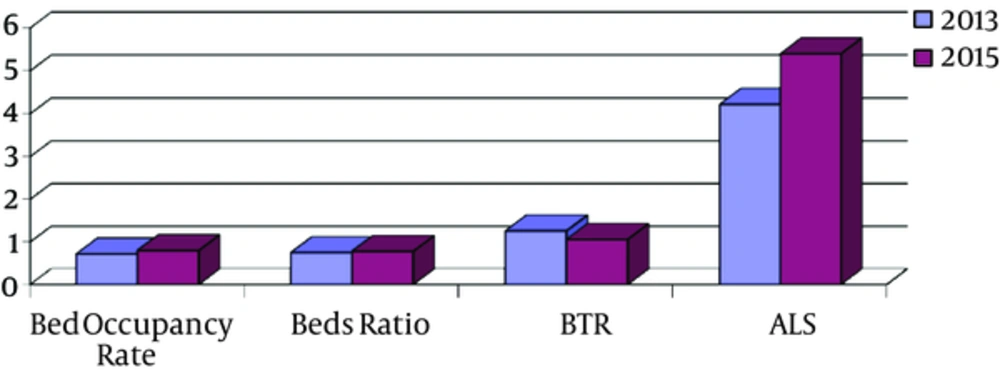
A comparison of the mean differences in the performance indicators before and after the implementation of the HSRP using the paired sample t-test indicated a statistically significant increase for the indicators of bed occupancy ratio, inpatient to constructed beds ratio, the mean length of stay, frequency of patients admitted in the clinical and para clinical sectors, frequency of emergency and elective operations, and frequency of cesarean and normal delivery (P < 0.05). On the other hand, the hospital bed turnover rate revealed a significant decrease, compared to the year prior to the implementation of the HSRP (P < 0.05) (Table 3). The changes in the indicators studied during the year before and after implementation of the HSRP are shown in Figures 1 - 4.
| Performance Indicator | 2013 | 2015 | P Value |
|---|---|---|---|
| BOR | 72.70 ± 2.65 | 80.55 ± 2.91 | 0.001 |
| Inpatient to constructed beds ratio | 0.75 ± 0.01 | 0.78 ± 0.01 | 0.001 |
| BTR | 1.26 ± 0.32 | 1.06 ± 0.20 | 0.001 |
| ALS | 4.22 ± 0.18 | 5.40 ± 0.29 | 0.001 |
| Patients admitted in clinical sectors | 2110.16 ± 153.58 | 2553.00 ± 209.42 | 0.000 |
| Patients admitted in para clinical sectors | 17822.81 ± 892.05 | 21826.74 ± 1068.47 | 0.000 |
| Emergency operations | 189.18 ± 24.92 | 208.43 ± 26.30 | 0.003 |
| Elective operations | 517.95 ± 79.66 | 637.71 ± 80.55 | 0.000 |
| Normal delivery | 25.443 ± 74.50 | 29.520 ± 19.58 | 0.001 |
| Cesarean delivery | 264.33 ± 22.80 | 359.20 ± 38.24 | 0.000 |
| Normal to cesarean delivery ratea | 1.67 ± 0.13 | 1.46 ± 0.01 | 0.002 |
aAlthough the average number of normal delivery increased after the implementation of health transformation plan, the average normal to cesarean delivery rate decreased in 2015 in comparison to 2013.
5. Discussion
In the present study, the hospital performance indicators prior to and following the implementation of the HSRP with a time interval of 12 months were investigated in 10 teaching hospitals affiliated to Shiraz University of Medical Sciences. The results indicated that after the implementation of the HSRP, significant changes were made in the performance indicators of the examined hospitals. The findings of other similar studies in this field show the positive effects of the HSRP, which partly confirms the findings of the current study. In the Faridfar et al. study (2016), it was shown that the HSRP has had a great impact on the number of admissions, surgeries, and patients’ satisfaction (15). The findings of a study in Isfahan suggested that implementation of the HSRP could reduce the patients’ out-of-pocket expenses (13). Furthermore, the results of the Bahadori et al. study (2015) concluded that the reform can lead to a decrease in the overall costs of healthcare and hospitals as well and improve the cost effectiveness of services (11). According to research findings, the BOR indicator increased by 8% and enhanced from 72.7 to 80.55. However, the BTR decreased from 1.26 to 1.06. The average length of stay also increased from 4.22 to 5.40. One of the reasons for this could be the lower proportion of treatment costs paid by patients in the public sector in comparison with the private sector after the implementation of the HSRP and shifting them to public hospitals to receive health care, consequently. In this case, the public hospitals’ bed occupancy rate will increase and bed turnover intervals will decrease. In addition, average length of stay for patients will increase, ultimately. Similar studies conducted in the hospitals affiliated to Bushehr University of Medical Sciences (Iran) also came to the conclusion that the plan has enhanced the bed occupancy rate and the average length of stay and the bed turnover ratio has also been steadily increasing (27). Also, the results of the study by Sajadi et al. (2017) showed that BOR, ALOS, and BTR indicators have been increasing since the implementation of the HSRP (28).
The number of patients admitted in the clinical and para clinical sections was also one of the other indicators concerned in this study, which showed an incremental increase following the implementation of the HSRP. Clinical admissions may be increased due to reasons such as lower costs in the public sector, the implementation of resident physicians’ package, and the efficient use of specialized and specialist assistants in the hospitals. On the other hand, regarding the increase in para clinic admissions, it can be attributed to the increase in admissions due to the implementation of the HSRP in the examined period, since each single admission in the hospital requires diagnostic examinations, thus increasing in the number of para clinical admissions is expectable consideringupward trend in general admissions.
The findings of the Faridfar et al. study (2016), on the Hazrat-e-Rasoul hospital in Tehran (Iran), reflected an increase in the number of admissions in clinics and para clinics after the implementation of the plan (15). Among the other indicators studied in this study was the number of emergency and elective operations. These indicators have been increasing over the years following the implementation of the HSRP. An increase in the number of operations seems to not be surprising with regard to the increased number of admissions after the implementation of the plan. The findings were in a similar vein with the Faridfar et al. findings, suggesting an increase in all surgical operations in 2015 compared to 2013 (15).
The increased number of normal deliveries in the concerned hospitals was another impact of this plan. Although, the average number of normal deliveries increased after the implementation of the HSRP, the average normal to cesarean delivery ratio decreased in 2015, compared to 2013. In fact, the number of cesarean deliveries has increased with an increase in the number of normal deliveries. This noticeable issue indicates that HSRP wasn’t successful in meeting one of its goals, which is to reduce the rate of caesarean section and increase in normal delivery rate; however, there is a great way to achieve this goal.
Meanwhile, the report of Iran’s national institute for health research explains that the implementation of the plan after 1 year resulted in a 10.2% decrease in the total rate of cesarean delivery compared to the corresponding rate at the beginning of the plan (29). Pirouzi et al. (2016) claimed that the rate of cesarean delivery in the Kurdistan (Iran) province over a year after the implementation of the plan decrease by 14%, compared to the corresponding rate in 2013 (30), which is not consistent with this study. The reasons for not paying attention to normal delivery are simply not due to the financial factor that has been taken into account by the reform plan and other factors (cultural, medical) that are also involved. Therefore, this issue requires more cooperation from organizations outside the ministry of health in order to promote culture and raise mothers and society awareness.
Mentioning the limitations of the current study, the dispersion of hospitals, time consuming data collection process, which were broken down by the Medical Registry Unit of some hospitals delayed the collection of information. The inherent limitations of the research was the differences between the examined hospitals and the combination of services provided by them, which is in view of the purpose of the study on the impact of the reform plan on the performance indicators in total. Therefore, the average of the status of the indicators was used. Furthermore, we were not able to compare the reform with other studies because no similar reforms had been implemented in other countries.
5.1. Conclusions
The performance indicators in the hospitals significantly differed before and after the implementation of the HSRP. It can be concluded that by implementing the HSRP and changing the tariffs for health services and care, the willingness to admit to study centers and receive health care has increased, either because of the client’s request or the offer and willingness of the service provider. This has increased the bed occupancy rate and the average length of stay by increasing the number of active beds. Among the indicators, the normal delivery rate to cesarean section has been reduced after implementation of the reform plan in comparison with the pre-implementation, which is contrary to one of the general objectives of the plan. Therefore, in order to achieve the goal of decreasing the rate of cesarean delivery and promoting natural delivery, in addition to informing mothers about natural delivery and its advantages, it is recommended that suitable cultural platforms be provided by policy makers through intersectional cooperation.