1. Background
According to the latest statistics report in 2013, of the estimated 39.4 million HIV patients in the world, approximately 12.9 million receive antiretroviral therapy (1). In Iran, it is estimated that 85,000 people are infected with HIV; and currently, 464 patients with AIDS have been identified in Bushehr province (2).
Antiretroviral treatment (ART) is effective in reducing HIV-related morbidity and mortality (3). Today, 95% or greater adherence, maintained over time, is necessary to achieve viral suppression (3, 4). Virus resistance towards antiretroviral drugs develops in cases of inadequate adherence (5). Inadequate use of ART causes drug resistance and subsequent increase in viral load (6). However, research suggests that adherence rates fall within the range of 30% to 70%, but the rates of adherence decrease even further during treatment (4).
Considering the problems of creating and preserving adherence to therapy, it is highly important to use theories or models of behavior change in this field. One of the comprehensive predicting models used in health promotion behaviors is Pender’s HPM. The framework of this model was offered as a guide to explore the complex biopsychosocial processes that motivate individuals to engage in behaviors directed toward the enhancement of health. This model with ecological approach is applicable to any health behavior in which threat is not proposed as a major source of motivation for behavior (7). Therefore, this model with ecological approach and consideration of biopsychosocial factors seem to be useful in adhering to antiretroviral therapy.
According to this model, health promotion behavior is influenced by personal and interpersonal elements such as individual characteristics and experience (e.g., personal, biological, psychological, and social factors, and prior related behaviors) and behavioral specific cognitions and affects (e.g., perceived benefits of action, perceived barriers to action, perceived self-efficacy, activity related affect, interpersonal influences from family, peers, and providers, and situational influences) (7).
Several studies have been conducted on adherence to ART, but not on the behavioral change model (8-10), and only few studies have focused on constructs (11, 12). Therefore, many studies should be conducted using models and theories of behavior change to investigate the efficiency of such models in adherence to therapy.
2. Objectives
The present study was conducted to use HPM as a theoretical framework to design an educational plan in adherence to ART in HIV- infected patients to consider personal and interpersonal effective elements (family, friends, and social support).
3. Methods
3.1. Participants
This randomized trial study (IRCT2015022821262N1) was conducted on 61 HIV positive patients at a behavioral disease counseling center in Bushehr, a southwestern province in Iran. All patients met the study’s inclusion criteria (18 years of age or over, the ability to read and write, free of marked cognitive impairment, CD4 (glycoprotein on the surface of immune cells) below 350, and prescribed ART at study inception). The study protocol was approved by the ethics committee of Bushehr University, Iran, and informed consent was obtained from all participants prior to participation.
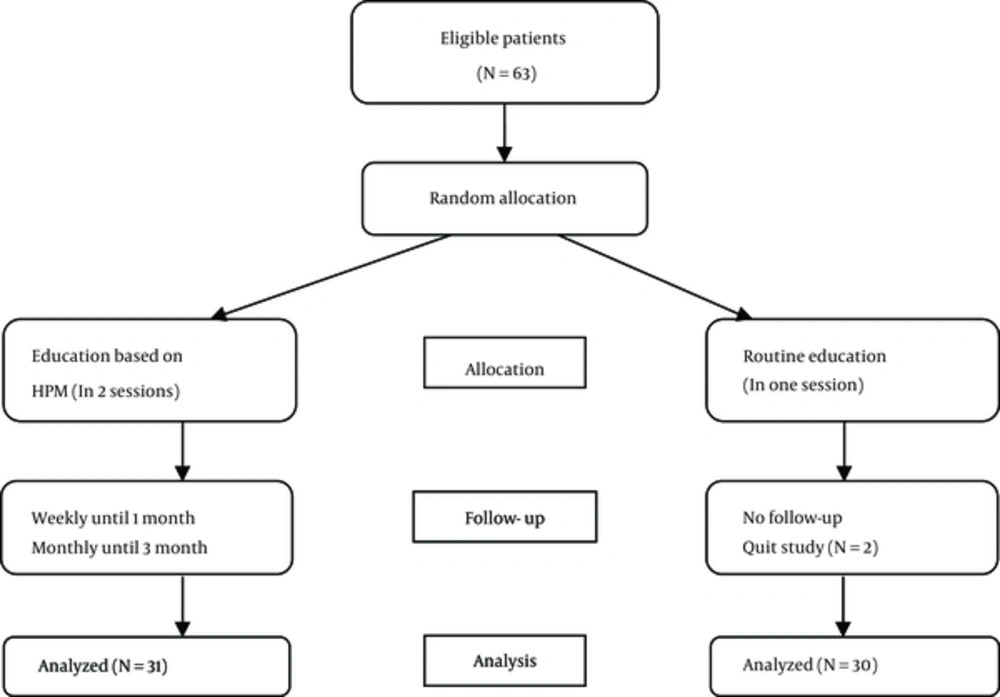
Because the number of eligible patients was limited, all patients participated in this study. Then, those who were qualified for participation were randomly assigned into one of the 2 groups: (1) intervention group, and (2) control group. Participants were given a code and the codes were randomly divided into 2 groups.
In the intervention group, 31 patients initially entered the study and completed the study. In the control group, 32 patients initially entered the study, of whom 2 left the study due to lack of time and submission of incomplete data questionnaire.
3.2. Instruments
Data collection tool in this study consisted of 3 sections. The first section inquired about individual characteristics and experiences by 10 questions about age, sex, educational level, mode of HIV transmission, disclosing HIV diagnosis to family, number of ART prescribed pills, duration of treatment, experiencing side effects, history of non-adherence to ART, and history of non-adherence to other treatments.
The second section included constructs related to behavior- specific cognitions and effects containing perceived benefits of adherence to therapy, perceived barriers to medicine, self-efficiency of medicine use, family social support, and effect or belief about ART. The constructs include perceived self-efficacy, perceived barriers, perceived benefits, prior related behavior, interpersonal influence (social support) as well as demographic characteristics that were significant in most of the studies (7).
Perceived benefits: To evaluate perceived benefits of ART, the Drug Attitude Inventory was used 5 items. These questions were evaluated using a 5-point Likert scale, ranging from strongly agree = 5 to strongly disagree = 1 (13).
Affect about ART: Horn et al. (1999) designed the beliefs medicines questionnaire (BMQ) to measure beliefs about medicines in HIV- infected patients. The original version of this scale, which included 10 items, assessed the beliefs about specific medications using 2 subscales, each with 5 questions evaluating the beliefs on the necessity of using prescribed medicines and 5 questions evaluating the worries about the long-term effects of using medications. The questions of this study’s construct were evaluated based on a 5-point Likert scale from strongly agree = 5 to strongly disagree = 1 (14).
Perceived Barriers: patient medication adherence questionnaire (PMAQ) was designated to assess the perceived barriers of adherence to therapy. This scale has 25 items, wherein all the items are rated using a Likert scale from strongly agree = 5 to strongly disagree = 1 (15).
Perceived Self-efficiency: Self-efficacy refers to people’s judgments on their own possibilities in relation to situational behavior. This standard questionnaire includes 12 items, wherein all the items are rated using 0 (can’t do it at all) to 10 (can do it completely) response scale (16).
Social Support: The questionnaire designated by Sherbourne and Stewart (1991) containing 19 questions was used. It evaluated family members and friends support in 4 different mental-emotional areas such as informational support, emotional support, affective support, and positive social support using 4-point Likert scale from never = 1 to always = 4 (17).
The third section evaluated adherence to therapy. Self-report adherence therapy was determined using the Questionnaire of Adherence to Therapy designed by the Center for AIDS Prevention Studies of University of California. The adherence to antiretroviral therapy was evaluated with 5 questions (18).
All questionnaires, except the questionnaire on adherence to therapy, were answered in 3 stages: before, immediately, and 3 months after education. The adherence questionnaire was completed before and 3 months after the educational sessions.
All the instruments were translated by the principal researcher and a bilingual person and were then validated using the back translation technique. The translated instruments were reviewed by a group of Iranian health education experts. Several items were omitted considering the opinion of the panel of experts, content validity index (CVI), and content validity ratio (CVR). One item of affects about ART questionnaire (I don’t know how my ARVs work), 4 items of perceived barriers to antiretroviral adherence questionnaire (Feeling embarrassed to get the medications at a drug store; sometimes refills are not acquired due to high cost, it is easy to talk to the doctor about medications, denying medicines are helping), and 1 item of social support questionnaire) availability of someone to get together for relaxation (were omitted. Prior to data collection, the questionnaires related to constructs were tested for reliability. All the questionnaires were reliable, and Cronbach’s alpha coefficient was 0.68 for affect about ART, 0.72 for perceived barriers, 0.73 for perceived benefits, 0.95 for social support, and 0.97 for self-efficiency.
3.3. Intervention
In addition to the standard clinic treatment, face to face education was provided for the patients (N = 31) in the intervention group in 2 sessions with a 2-week interval. The objectives of the study were explained to the patients, and then, they were asked to fill out a written consent form and the questionnaires.
In the first session, AIDS, treatment of the disease, and benefits of treatment were discussed; benefits of treatment were explained in the face to face educational session based on the patient need. At the end of this session, each patient was informed about the educational information presented in the second session.
In the second session, each patient was informed about the barriers of the use of medicine, and solutions were itemized to limit each barrier. Moreover, to reduce medication errors or fogetfullness, Medminer (tools and devices that can help patients take their medications on time every day) such as a reminder box and phone reminder were used. In the same session, the participants’ beliefs and perception about medications were investigated based on the present detailed information on side effects associated with ART. Thus, this could provide participants with strategies to manage their side effects and improve their affects about medicines. To gain social support for the participants, the second session was held in the presence of a family member that had been appointed by the participant in the first session. The family member was invited by the researcher through a Witten invitation as well as a phone call.
Moreover, verbal persuasion was used to improve self-efficiency. Those patients who regularly used medicines were verbally encouraged and those who had not used medicine, were asked to attend another (additional) educational session; this extra session was held to evaluate barriers, offer solution, and encourage them to use take their medicine regularly.
The intervention group received weekly phone calls for 1 month; and thereafter, they received monthly calls until the end of the study period (3 months).
All participants in the control group received the standard clinic treatment (ART) as follows: (1) refilling their prescription monthly, (2) being provided with an initial explanation about ART, its action and side effects, and (3) having their blood regularly drawn so that their CD4 cells could be measured. They completed the questionnaires at baseline, 2 weeks, and 3 months after the intervention. The study flowchart is shown in Figure 1.
3.4. Statistical Analysis
Data were analyzed using statistical package for social sciences software (SPSS) Version 18.0. Descriptive statistics, chi- square test, t test, repeated measurement ANOVA, and Wilcoxon signed ranks test were used for data analysis. Chi-square test was used to compare the 2 groups with respect to the qualitative variables and independent t test was utilized for quantitative variables such as age. The repeated measurement ANOVA was used to compare the mean scores of constructs within and between the groups. Wilcoxon signed ranks test was used to evaluate the rate of ART adherence in the 2 groups during the intervention.
A P value of less than 0.05 was considered as statistically significant.
3.5. Ethical Considerations
The aim of this study was verbally explained to the patients who met the inclusion criteria. The participants were told that they could withdraw from the study at any time and that all information would be kept confidential. The required permissions were obtained from the Vice-Chancellor for research of Bushehr University of medical sciences, department of education in city of Bushehr. Also, the study was approved by the university’s ethics committee (Ethics code B-93-16-15).
4. Results
A total of 61 HIV- infected patients (N = 31 in the intervention group and N = 30 in the control group) participated in this study. The demographic characteristics of the participants of the 2 groups were similar. For instance, the average age of the intervention group was 40.26 ± 8.28, while that of the control group was 39.13 ± 8.99 (P = 0.614). Other demographic data related to ART adherence are presented in Table 1.
| Individual Characteristics and Experiences | Intervention Group | Usual Care Group | Statistics | P Value | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Sex | 2.79 | 0.146 | ||||
| Male | 20 | 64.5 | 25 | 83.3 | ||
| Female | 11 | 35.5 | 5 | 16.7 | ||
| HIV infection mode of transmission | 2.78 | 0.427 | ||||
| Partner exposure | 8 | 25.8 | 5 | 16.7 | ||
| Heterosexual exposure | 1 | 3.2 | 3 | 10 | ||
| Injecting drug use | 19 | 61.3 | 21 | 70 | ||
| other | 3 | 9.7 | 1 | 3.3 | ||
| Educational level | 1.99 | 0.157 | ||||
| Less than Diploma | 21 | 67.7 | 25 | 83.3 | ||
| Diploma or higher | 10 | 32.3 | 5 | 16.7 | ||
| Has disclosed HIV diagnosis to family | 0.18 | 0.668 | ||||
| Yes | 28 | 90.3 | 28 | 93.3 | ||
| No | 3 | 9.7 | 2 | 6.7 | ||
| Number of AART prescribed pills, pill | 0.89 | 0.639 | ||||
| One | 1 | 3.2 | 1 | 3.3 | ||
| 2 - 5 | 23 | 74.2 | 19 | 63.3 | ||
| 6 - 10 | 7 | 22.6 | 10 | 33.4 | ||
| Duration of treatment, mo | 4.11 | 0.250 | ||||
| Less than 12 | 3 | 9.7 | 6 | 20 | ||
| Between 12 - 23 | 3 | 9.7 | 7 | 23.3 | ||
| Between 24 - 36 | 6 | 19.4 | 4 | 13.3 | ||
| More than 36 | 19 | 61.3 | 13 | 43.4 | ||
| Experiencing side effects | 0.23 | 0.632 | ||||
| Yes | 10 | 32.3 | 8 | 26.7 | ||
| No | 21 | 67.7 | 22 | 73.3 | ||
| History of non-adherence to AART (prior related behaviors) | 0.138 | 0.710 | ||||
| Yes | 13 | 41.9 | 14 | 46.7 | ||
| No | 18 | 58.1 | 16 | 53.3 | ||
| History of non-adherence to other treatment (prior related behaviors) | 0.45 | 0.50 | ||||
| Yes | 14 | 45.2 | 11 | 36.7 | ||
| No | 17 | 54.8 | 19 | 63.3 | ||
Demographic Features and AIDS Treatment Adherence Behaviors in Two Groups Prior to Training
In this study, it was found that patients in the 2 groups were similar in their behavior- specific cognitions and affects related to ART adherence before education, but the difference was statistically significant between the 2 groups after the intervention in all constructs (Table 2).
| Constructs | Times | Intervention Group | Usual Care Group | Between Group: P Value |
|---|---|---|---|---|
| Affect about ART | Before intervention | 34.77 ± 5.10 | 36.00 ± 5.40 | 0.000 |
| After intervention | 41.90 ± 4.16 | 34.20 ± 4.84 | ||
| 3 months later | 42.00 ± 4.49 | 34.13 ± 5.27 | ||
| Within group: P value | 0.000 | 0.164 | ||
| Family and Friend support | Before intervention | 51.03 ± 16.38 | 50.27 ± 14.99 | 0.084 |
| After intervention | 53.71 ± 15.89 | 49.50 ± 13.88 | ||
| 3 months later | 56.93 ± 15.13 | 49.60 ± 14.42 | ||
| Within group: P value | 0.008 | 0.935 | ||
| Perceived self-efficacy | Before intervention | 100.84 ± 21.03 | 99.27 ± 23.78 | 0.001 |
| After intervention | 111.81 ± 11.63 | 94.00 ± 22.16 | ||
| 3 months later | 115.26 ± 12.16 | 95.90 ± 19.93 | ||
| Within group: P value | 0.000 | 0.436 | ||
| Perceived benefits | Before intervention | 22.22 ± 2.63 | 21.97 ± 2.34 | 0.000 |
| After intervention | 24.10 ± 1.78 | 20.80 ± 3.24 | ||
| 3 months later | 24.93 ± 0.25 | 21.13 ± 2.86 | ||
| Within group: P value | 0.000 | 0.150 | ||
| Perceived barriers | Before intervention | 55.52 ± 12.85 | 48.70 ± 12.11 | 0.000 |
| After intervention | 35.45 ± 10.31 | 51.80 ± 10.17 | ||
| 3 months later | 32.77 ± 11.30 | 50.27 ± 12.34 | ||
| Within group: P value | 0.000 | 0.237 |
Constructs’ Scores of Health Promotion Model During Interventiona
The results of pre- and posttest (immediate and 3 months later) in the intervention group were compared by repeated measurement ANOVA, and the results revealed an increase in all constructs (P < 0.001) and a decrease in perceived barrier in adherence to ART (P < 0.001).
However, the results revealed no significant differences between the pre- and posttest scores for all constructs in the control group.
After comparing the 2 groups, no significant difference in the scores of all constructs was observed (P > 0.05) (Table 2).
Furthermore, of the 31 patients in the intervention group before education, only 25.8% (N = 8) had more than 95% adherence to ART, but after education, 96.8% (N = 30) had more than 95% adherence to treatment. In the control group, 56.7% (N = 17) had more than 95% adherence, indicating that no significant changes occurred before education. Other information on the rate of ART adherence is demonstrated in Table 3.
| Rate of AAT Adherence | Less Than 80% | 80% - 95% | More Than 95% | P Value | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Intervention group | |||||||
| Before | 4 | 12.9 | 19 | 61.3 | 8 | 25.8 | 0.000 |
| 3 months later | 0 | 0 | 1 | 3.2 | 30 | 96.8 | |
| Usual care group | |||||||
| Before | 1 | 3.3 | 12 | 40 | 17 | 56.7 | 0.614 |
| 3 months later | 3 | 10 | 10 | 33.3 | 17 | 56.7 |
Rate of ART Adherence in Two Groups During Intervention
5. Discussion
The present study aimed at determining the effect of education based on HPM on adherence to ART in HIV positive patients.
In this study, education promoted the patients’ perception of the advantages of ART, their self-efficiency in using medication, and social support. Also, education modified the patients’ affects regarding antiretroviral therapy and decreased barriers of adherence to medicine. Moreover, by changing the patients’ beliefs about therapy, adherence to medicine increased significantly, indicating the effect of education based on HPM on adherence to therapy in the patients.
In this study, education on the improvement of feelings about treatment led to an increase in adherence to therapy. In several studies, the positive effect of education on beliefs about the use of medication and adherence to therapy has been reported (9, 11, 19). In a study by Cote (2012), it was pointed out that computer training could improve the feelings and affects about therapy and increase adherence almost by 20% (11). However, in a study conducted by Mini et al. (2012) in India, it was reported that as a result of social stigma, training could not change the individuals’ beliefs about therapy, but adherence to ART increased from 43% to 88% after intervention. The reason for the ineffectiveness of Mini’s (20) study in changing the individual’s beliefs about medicine can be attributed to the lack of application of behavior change models and placing emphasis only on the side effects of medicines during teaching. In a study in South Africa (14), it was shown that belief about medicine increase adherence to therapy, and this is in line with the findings of this study. Therefore, it seems that through the adjustment of feelings and affect about antiretroviral medicine, adherence can be improved.
Smith (1997), in his study, found that patients with much adherence to therapy have the advantage of increased perception about medicine (13); he further emphasized the advantage of individual’s increased perception about medicine on adherence to therapy, and his finding was consistent with the results obtained in the present study.
The individual’s perception about self-efficiency in adherence to therapy has been considered an important determinant in AIDS therapy owing to the fact that as self-efficiency increases, patient’s depression decreases and problem solution skills increase; and as a result, the individual’s tendency to medicine use increases (13). In several studies (13, 16, 21) , it was reported that education improves individual’s perception about self-efficiency and as this construct increases, adherence to ART increases as well; these results are in line with recent findings. In Cote’s (11) study, 4 sessions of computer training increased the patients’ self-efficiency in the regular use of medicine and increased the adherence to therapy from 58% to 75%.
Perceived social support is a strong predictor of adherence to therapy. With increase in social support and family and friends’ encouragement for adherence to therapy, the patient’s tendency to medicine use will increase. Another aspect of social support is the patient- provider relationship, which is strongly related to adherence (22). In this study, as family support increased, patients’ adherence to ART have also increased, and this was consistent with the results obtained by Lyon (22).
As reported by Lyon (2004), 6 training sessions in 12 weeks in the presence of family members increased the patients’ adherence to therapy (91%) (22). In Safren’s study (2000), education increased the patient’s perception about social support to adherence to therapy, and this is in agreement with the findings of this study (23). Therefore, an increase in family support could increase patients’ adherence to ART.
One of the effective factors on adherence to therapy is recognizing perceived barriers to adherence. Patients encounter numerous barriers when it comes to the complexities of medicine regimen and side effects. Therefore, offering interventions to help solve patients’ problems, planning for regular medicine use, and offering strategies to ease and recall medicine diet are recommended. In this study, adherence to therapy increased through providing education about the side effects of medications, offering med minder, and removing other barriers.
In a study by Smith (1997), patients with much adherence to therapy were reported with fewer barriers (13). The findings of Ferguson’s study (2002) revealed that memory aspect is the strongest barrier to adherence to therapy (24). Lyon (22), in his study, found that provision of medicine box, calendar, and alarm can increase adherence to ART (91%), and this result is in line with the results obtained in this study. Thus, adherence to therapy can significantly increase by removing the barriers, especially forgetfulness.
The standard degree of adherence to therapy in patients with AIDS is over 95%. Numerous studies have reached this degree of adherence (10, 25, 26).
The result of this study revealed that after 2 training sessions, 96.8% of the patients reached over 95% adherence to therapy, which is in line with numerous studies. Accordingly, in a study by Spire (2004), it was reported that 3 training sessions without using the behavior change models caused over 95% adherence to therapy in 81% of the patients (8). In an interventional study conducted by Pradier et al. (1999) in Canada, 100% adherence to therapy was reported in the intervention group after 3 training sessions (10). Goujard et al. (2003), in their study, reported that a 1 year training program caused 95% adherence to therapy in 96% of the patients (27). In this study, despite the limited number of sessions and short duration of the intervention, it seems that the use of HPM has desirable effects on adherence to therapy.
Some of the limitations of this study can be ascribed to a short follow-up period, but if it was long (for instance 6 months), more patients would have found enough time to adhere to ART. Secondly, the examination of health beliefs and adherence to ART was self-reported, which is sometimes overestimated; however, because both groups were examined with a particular method, this was true for both groups; the medicine (missed dose) offered to the patients by the counseling center was recognizable.
In this study, training in limited sessions changed the behavior- specific cognitions and affect and also significantly increased the degree of adherence to therapy. Such a high degree of adherence showed the efficiency of HPM on adherence to therapy. Therefore, it seems that the results obtained in this study are useful for educational planning of the counseling clinics and could improve adherence to therapy.
-thumbnail.webp)