1. Context
Breast cancer (BC) is the most common type of female cancer (1), afflicting nearly 12% of women population worldwide (2). As one of the most important cancers among women, BC accounted for 25.2% of all cancer cases diagnosed in women in 2016 (3). The incidence of BC is higher in most developed countries than in developing countries (4).
According to the statistics of the World Health Organization (WHO), one of every 8 - 10 women is diagnosed with BC (5). In Iran, one of every 10 - 15 women are diagnosed with BC. However, the age at the incidence of BC is at least 10 years lower in Iran than in developed countries (6). In a study performed by Azgomi et al., the incidence of BC was reported to be 26.4 per 100000 Iranian population (7).
To date, extensive advances in the treatment of BC have resulted in a better response to treatment and have increased the survival of these patients (8). Nonetheless, there are some factors affecting the mental health of BC patients, including suffering from the disease, family members’ concerns about the future, fear of death, treatment complications, reduced function, probability of deformity, pain, lack of social welfare, and sexual problems (9-11). In this context, depression and anxiety disorders emerge in most patients. Studies have shown that depression and anxiety are the most common problems that appeared in cancer patients (12, 13). Severe depression often causes the patients to spend the rest of their lives waiting for death (14). Moreover, studies have shown a higher prevalence of anxiety and depression in patients with BC than in patients with other types of cancer. Many BC women experience mild-to-severe symptoms of the disease, such as anxiety, depression, and feeling of hostility (15). In fact, BC increases the risk of depression and anxiety in such groups when compared to the general population (16). In some studies, the risk of major depression in patients with BC was twice that in the general population (17). Additionally, a previous study indicated that the risk of death was higher in adults with cancer suffering from depression (18).
Long-term anxiety and depression in patients with BC can reduce their well-being and negatively affect the effectiveness of the recovery process (19). Therefore, such patients cannot easily return to their normal lives due to stress and psychological anxiety while depression could affect their immune system (20). Depression is a risk factor for reducing the survival of cancer patients and an important factor in treating patients who deny their disease. Anxiety and depression can also affect patients’ psychological status, quality of life, immune system, life expectancy, disease progression, treatment efficiency, and length of hospitalization (21, 22).
In Iran, there are several studies assessing depression among cancer patients (23, 24). Since BC is the most important malignancy in women and no systematic review has examined its prevalence among women with BC, the present systematic review aimed to address this epidemiological gap.
2. Evidence Acquisition
This systematic review was designed in 2016 and commenced in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (25).
2.1. Search Strategy
A literature search of published studies was carried out in the international databases (Medline/PubMed, Scopus, Web of Sciences, Embase, and Google Scholar) for English papers and Iranian databases (Scientific Information Database (www.sid.ir), MagIran (www.magiran.com), IranMedex (http://www.barakatkns.com), and Irandoc (www.irandoc.ac.ir)) for Persian papers.
The Medical Subject Headings (MeSH) keywords were used including “Breast cancer”, “Breast neoplasm”, “Breast tumors”, “Depression”, “Depression disorder”, “prevalence”, “frequency”, “epidemiology”, and “Iran”. The obtained papers were imported into an EndNote X7 library (Thomson Reuters, Carlsbad, CA, USA) and duplicates were removed. No language and time limitations were considered.
2.2. Selection Criteria and Quality Assessment
The titles and abstracts of all retrieved papers were independently reviewed by two reviewers. The full-texts of all relevant articles were then assessed by both reviewers. Original, cross-sectional studies in English or Persian that reported the prevalence of depression in BC patients were included in this meta-analysis. On the other hand, prospective, case-control, and experimental studies, as well as clinical trials, reviews, commentaries, case reports, systematic reviews, and meta-analyses, were excluded. One of the researchers extracted the data from the eligible studies and entered them into a pre-designed data extraction form. The study setting and design and the prevalence of depression and its associated factors were extracted. Then, the results were synthesized in a narrative review. Discrepancies between the reviewers were resolved by consensus.
2.3. Quality Assessment
In order to assess the quality of articles, a checklist prepared by the Joanna Briggs Institute (JBI) was used (26). The purpose of this appraisal is to assess the methodological quality of a study and determine the extent to which a study has addressed the possibility of bias in its design, conduct, and analysis.
2.4. Risk of Bias Across Studies
A random-effects model was used for minimizing the risk of bias across studies (27, 28).
2.5. Statistical Analysis
Heterogeneity was assessed by Cochran’s Q test (with a significance level of P ≤ 0.1) combined with I2 index (with a significance level of I2 > 50%). In the presence of significant heterogeneity (P ≤ 0.1 and I2 ≥ 50%), a random-effects model (with inverse variance method) was used. All analyses were carried out using STATA version 13 software (STATA Corp. LP, College Station, Texas).
3. Results
3.1. Description of Literature Search
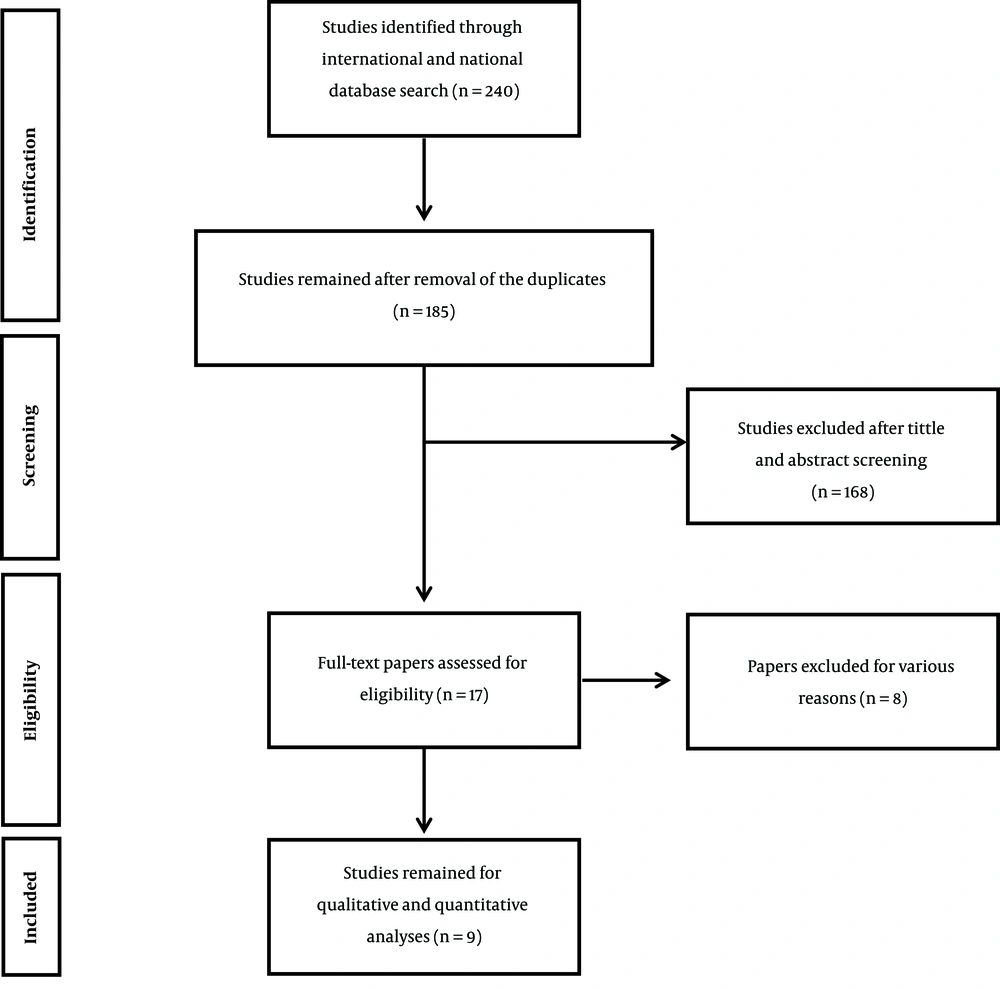
In total, our search retrieved 240 potentially relevant studies, out of which 185 unique studies were reviewed and 17 studies were entered into the second stage of evaluation. Overall, we found nine unique studies (six in English and three in Persian). Study retrieval and selection process is outlined in Figure 1. Some studies were excluded from the review since they were not relevant to the topic (n = 166), had an inappropriate study population (n = 8), or were duplicated (n = 2).
3.2. Description of the Included Studies
The included studies were published from 2002 to 2014. Based on the geographical location, two studies were conducted in Isfahan province (29, 30), two in the city of Babol (31, 32), one in Kerman province (33), one in the city of Zahedan (23), one in Tehran province (34), one in Kermanshah province (35), and one in Hamadan province (36). The design of the included studies and the characteristics of BC patients are listed in Table 1.
| Author | Time of Study | Place of Study | Sample Size | Event | Prevalence of Depression, % | 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower, % | Upper, % | ||||||
| Ramezani (33) | 2002 | Kerman | 120 | 49 | 40.8 | 32.4 | 49.8 |
| Mashhadi et al. (23) | 2005 | Zahedan | 42 | 32 | 76.2 | 61.1 | 86.7 |
| Montazeri et al. (34) | 2005 | Tehran | 177 | 52 | 29.4 | 23.1 | 36.5 |
| Shakeri et al. (35) | 2008 | Kermanshah | 78 | 33 | 42.3 | 31.9 | 53.5 |
| Derakhshanfar et al. (36) | 2008 | Hamadan | 111 | 68 | 61.3 | 51.9 | 69.9 |
| Didehdar et al. | 2009 | Babol | 60 | 30 | 50 | 37.6 | 62.4 |
| Taghavi et al. (29) | 2011 | Isfahan | 240 | 82 | 34.2 | 28.4 | 40.4 |
| Musarezaie et al. (30) | 2012 | Isfahan | 297 | 102 | 34.3 | 29.2 | 39.9 |
| Nikbakhsh et al. (32) | 2014 | Babol | 40 | 11 | 27.5 | 15.9 | 43.2 |
The Design of the Included Studies and the Characteristics of BC Patients
3.3. The Results of the Meta-Analysis
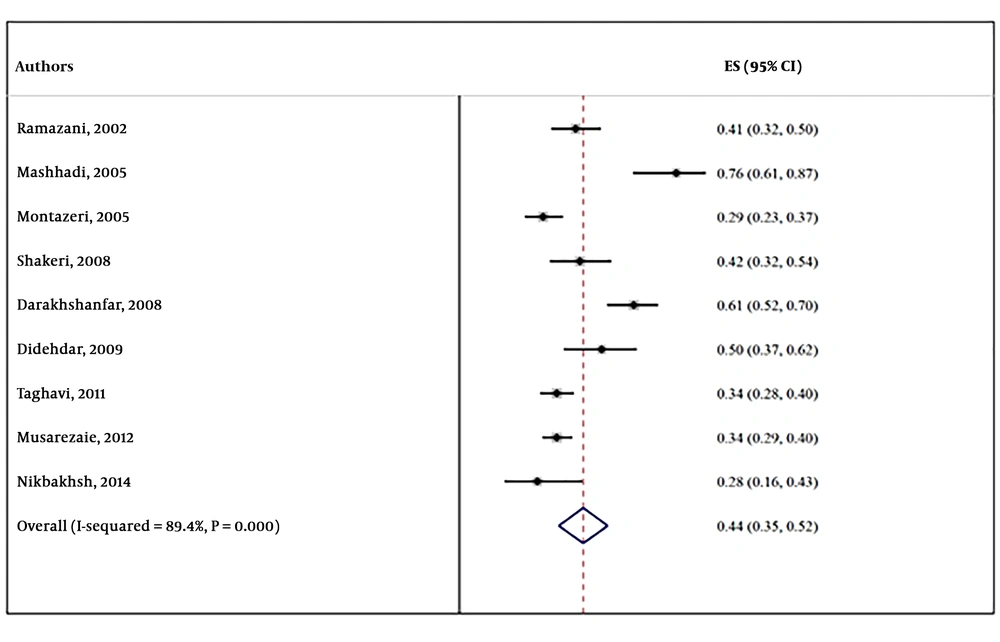
In total, 1165 participants in the nine selected studies were analyzed. The overall prevalence of depression in BC patients was 44% (95% CI: 35% - 52%). In addition, the results of Cochran’s test proved the heterogeneity of studies (Q = 1678.2, df = 8, I2 = 89.4%, P < 0.001). The forest plot of the random-effects meta-analysis of the prevalence of depression in BC patients in Iran is presented in Figure 2.
4. Conclusions
Cancer is the third leading cause of mortality in Iran (37-42). GLOBOCAN 2012 reported that BC was the most common type of cancer among Iranian women (43). In the present study, the prevalence of depression among Iranian BC patients and its geographical diversity were evaluated through a systematic review and meta-analysis. The study showed that the prevalence of depression was relatively high in patients with BC, which is consistent with the studies conducted in other countries (44-46).
Generally, the prevalence of anxiety and depression in BC patients is much higher than that of the general population (47). Although its diagnosis does not mean imminent death, many studies in Western and Asian countries have shown that such diagnosis can cause deep emotional problems such as stress and anxiety for patients and their families (43). The high prevalence of anxiety and depression might be attributed to the implications of this diagnosis in the minds of patients and their family members, including the probability of deformity, pain, lack of social welfare, dependency, and ultimate death (46).
The prevalence of depression was different (27.5% - 76.2%) among patients living in various provinces of Iran. Such a difference was also reported in the studies performed in Asian countries (48). Nonetheless, the prevalence of depression varied from 12.5% to 31% in patients with BC in Asian countries, which is lower than the rates reported in Iran (49). The difference in the prevalence of depression in different regions of a country can be the result of some factors. These factors are divided into two categories. The first category includes sociodemographic factors, such as age, marital status, education level, number of children, employment status, type of treatment, duration of suffering from the disease, income level, environmental conditions, and social support. The second category includes cancer-related factors, such as fatigue, pain, disability, side effects of radiotherapy and chemotherapy after mastectomy, void of femininity and attractiveness that makes a person feel less ladylike with poor body image, which all are associated with depression (50-54).
Alcalar et al. conducted a study on women with BC in Turkey and reported a significant positive correlation between cognitive disorders and depression in women with breast cancer (55). These results were in line with those obtained by Mehnert et al. that showed patients with children experienced a higher anxiety level (56). In the study by Ramezani and Shakeri et al. the prevalence of depression was higher in patients who were employed and had higher education levels (33, 35). Moreover, Mashhadi et al. indicated that higher education level caused higher depression levels among patients (23). Nikbakhsh et al., Ramezani and Shakeri et al. performed several studies on the relationship between age and the prevalence of depression and reported a significant relationship between the two variables in patients with BC (32, 33, 35). These results were in line with a study conducted in Thailand (57).
4.1. Limitation of Study
The current study had several limitations, the first of which was publication bias. We attempted to minimize this problem by searching various databases in English and Persian, but we did not have access to non-published articles. Second, the studies were performed in different parts of the country and cultural differences might have affected the prevalence of depression. However, this issue was not addressed in the selected studies. Third, the majority of the selected studies was performed on a small group of clinical patients and was not population-based. Lastly, this study only included cross-sectional studies; hence, controlling the confounding factors was not a guaranty.
Despite all these limitations, the collected data from these studies showed that patients with BC were at risk of depression. Therefore, these patients might need medical treatment or psychological interventions. Thus, identifying the risk factors is necessary for physicians in order to take care of these patients.
4.2. Recommendation
In future systematic reviews and meta-analyses, investigating the prevalence of depression in BC patients should not be limited to Iran, and areas covered by WHO should be taken into consideration.