1. Introduction
Financial protection is one of the 3 dimensions of universal health care coverage (UHC) (1). However, out-of-pocket (OOP) payments can influence the equality of access to and utilization of health services and decelerate the movement toward UHC (2). Facing with CHE can influence the health of all household members and may push the households into poverty health cycle (3).
Different metrics are used to assist policymakers in becoming informed about the incidence and magnitude of direct payments for health care; one of them is catastrophic health expenditures, for which WHO has identified a specific definition: “Catastrophic heath expenditure occurs when a household’s total out-of-pocket health expenditure is equal to or exceeds 40% of its capacity to pay or nonsubsistence spending.” (4).The household capacity to pay is defined as the effective income remaining after basic subsistence needs have been met (4, 5) Evidence shows that every year approximately 44 million households, or more than 150 million individuals worldwide, face catastrophic expenditures (6).
Identifying the prevalence and determinants of catastrophic health expenditures leads to detection of vulnerable population groups in a society (7).
Iran is an upper-middle-income country (8), with a gross national income (GNI) per capita PPP international of $15 600 in 2013 and a total expenditure on health per capita of $1562 in 2012 (9). In Iran’s high-level documents, i.e., the Fifth Plan of Development (2011 - 2015), is explicitly mentioned that the portion of direct expenditure for health services should be 30% at most, and the ratio of population who face CHE should be reduced to less than 1% (10). However, according to the reports of national health accounts of 2011, it was revealed that out-of-pocket payments for health care services in Iran increased from 2002 to 2008, increasing from 53.49% in 2002 to 53.56% in 2008. In 2005, the percentage reached its highest peak at 55.27% (11).
2. Objectives
The percentage of households facing CHE during the years has been calculated in various studies in Iran and different prevalence of CHE has been reported. Also, some of these studies have investigated factors affecting the possibility of facing CHE, therefore, in this systematic review, we aimed at estimating the pooled prevalence of CHE in Iran and identifying and summarizing the determinants of CHE among Iranian households.
3. Methods
3.1. Eligibility Criteria
Only cross-sectional household surveys that used WHO methodology to calculate catastrophic health expenditures were included in this study. Surveys that used another methodology or did not use 40% as the threshold and studies that calculated catastrophic health expenditures for special diseases were excluded.
3.2. Information Sources
To identify papers (citations or records) relevant to the topic of catastrophic health expenditures, a systematic search of English and Persian databases was conducted on January 2015. Three English databases of PubMed, Scopus, Web of Science, and the Cochrane Library, and 3 Persian databases of SID, Magiran, and IRANDOC were searched. Also, some literature was obtained through colleague communications.
3.3. Search Strategy
Search strategies used combined the following keywords: ‘catastrophic’, ‘expenditure’, ‘cost sharing’, ‘out-of-pocket’, ‘household’, and ‘household survey’, with the word ‘Iran’. Combinations of keywords were used in searches for the publication title, abstract, keywords, or full text (Appendix A).
There were no limitations regarding the year of publication, publication type, or format. After publications were identified, their bibliographies were checked for any relevant papers not found in the first search.
3.4. Data Extraction and Quality Assessments
A standardized template form was used to extract data from studies and publications satisfying inclusion criteria. Data were collected on the following subjects:
- Study characteristics (title, type, author, name of the study, or survey data obtained, years of study, location, imprint, in press)
- Quality evaluation of research methodology according to STORBE checklist (study design, study population, sampling method, sample size (number of households), and type of statistical analysis done)
- Methodology used to calculate CHE (household consumption expenditures and food expenditures definitions, health expenditures definition, methods used to calculate poverty line, amount of equivalence scale, method used to calculate subsistence expenditure, the household’s capacity to pay, and CHE threshold)
- Percentage of households facing CHE in total and in different income groups, standard error of CHE
- Effective factors as determinants of CHE using regression models (Studies that used logic regression models were included in this part of study.)
To identify the risk of bias in each study, its methodology was assessed and used to calculate CHE and its research methodology according to STORBE checklist.
In all studies, we used WHO methodology to calculate CHE, in some of them details of calculation had also been described; finally, we included all these studies to the systematic review.
For quality evaluation of research methodology, we used STORBE checklist, specially sampling method of studies and type of statistical analysis done were checked, moreover, method of sampling was random sampling in some studies, and in some others the process of sampling was explained.
3.5. Data Synthesis and Management
The meta-analysis included 27 surveys involving 440 410 households. All the included studies focused on percentage of CHE; however, the standard error of CHE was not reported in some of them. Therefore, it was calculated using binomial distribution formula; and the STATA Version 11 was used to calculate the 95% confidence interval for the prevalence when it was not reported.
To estimate the overall pooled prevalence of CHE, comprehensive meta-analysis software Version 2 was used.
Because of the importance of data sources to calculate CHE, subgroup meta-analyses were conducted to assess the influence of the study questionnaire that was used for data collection. Also, separate subgroup meta-analyses were conducted to assess the influence of scope of researches. Moreover, the effect of sample size and survey year on facing CHE was checked using meta-regression checked.
In some studies, the determinants of CHE were studied using a logic regression model, and the possibility of facing or not facing CHE was illustrated. These determinants were summarized and categorized.
4. Results
4.1. Included Studies
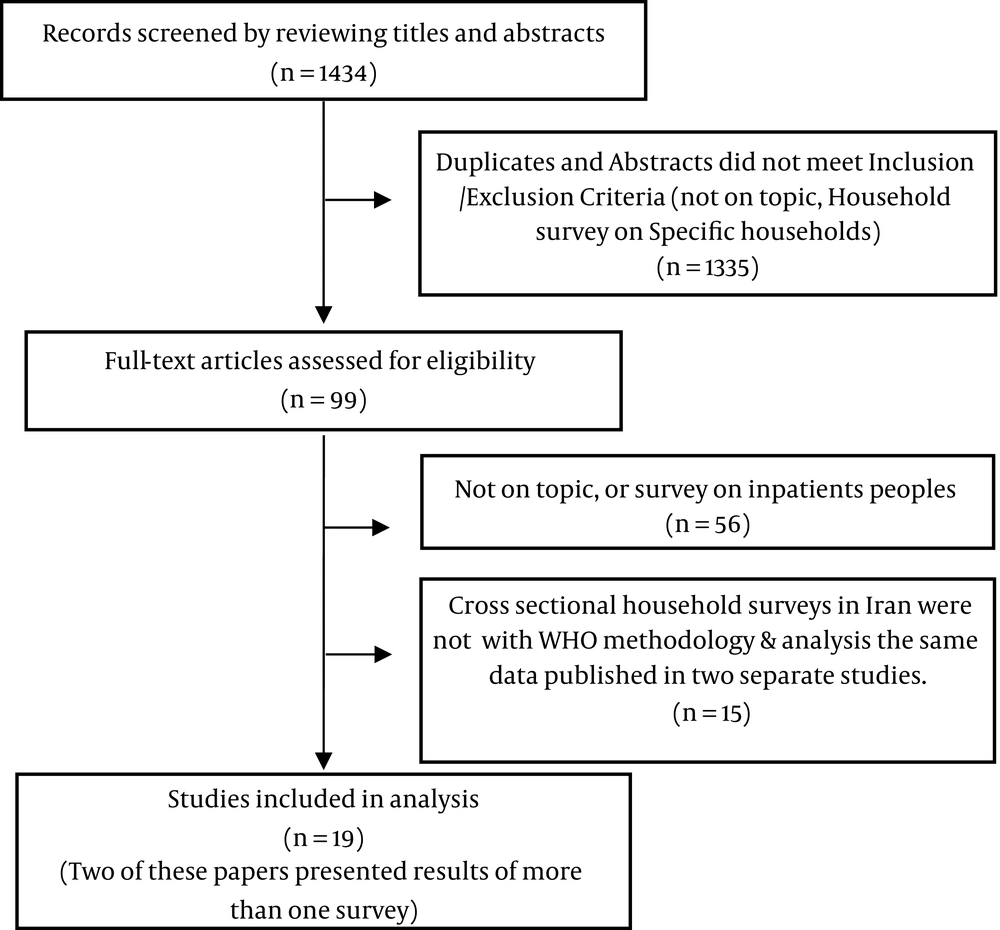
One of these articles presented the results of 2 surveys (12), and another report presented the results of an- 8- year study (13). In total, results from the surveys of 27 households extracted from 19 articles were included in the current systematic review.
4.2. Description of the Reviewed Results
In the 19 studies included in this systematic review, the CHE of Iranian households during 1995 to 2015 was studied.
Review of the studies conducted in Iran revealed that the data required calculating CHE was provided by 3 different questionnaires.
| No. | First Author | Questionnaire | Region /Scope (Name of Place) | Year of Survey | Sample size (HH) | HH with CHE, % | Has Logit Model |
|---|---|---|---|---|---|---|---|
| 1 | Soofi (14) | WHO questioner | National | 2001 | 10300 | 15.31 | Yes |
| 2 | Mohammad Alizade (15) | SCI questioner | National | 2002 | 32000 | 3.9 | Yes |
| 3 | Razavi (13) | SCI questioner | National | 1995 | 37233 | 2.13 | No |
| 1996 | 21863 | 2.13 | No | ||||
| 1997 | 21857 | 1.97 | No | ||||
| 1998 | 17404 | 2.13 | No | ||||
| 1999 | 27399 | 2.14 | No | ||||
| 2000 | 26873 | 2.18 | No | ||||
| 2001 | 26898 | 2.19 | No | ||||
| 2002 | 32086 | 2.32 | Yes | ||||
| 4 | Kavosi (12) | WHO questioner | At a city (Tehran) | 2003 | 579 | 12.6 | Yes |
| 2008 | 592 | 11.8 | Yes | ||||
| 5 | Mehrara (16) | SCI questioner | National | 2008 | 31283 | 2.5 | Yes |
| 6 | Karami (17) | WHO questioner | At a city (Maskan, Kermanshah) | 2008 | 189 | 22.2 | No |
| 7 | Nekoei Moghadam (18) | SCI questioner | National | 2008 | 39088 | 2.8 | Yes |
| 8 | Nekoei Moghadam (19) | SCI questioner | At a Province ( Kerman) | 2008 | 1480 | 4.1 | Yes |
| 9 | Amery (20) | WHO questioner | At a Province (Yazd) | 2011 | 400 | 8.3 | Yes |
| 10 | Asefzadeh (21) | Researcher-made questioner | At a city (Qazvin, Minodasht) | 2011 | 100 | 24 | No |
| 11 | Yousefi (22) | SCI questioner | National | 2011 | 36071 | 3.38 | No |
| 12 | Sabermahani (23) | Researcher-made questioner | At a city (Tehran) | 2011 | 34700 | 11.3 | Yes |
| 13 | Kavosi (24) | WHO questioner | At a city (Shiraz) | 2012 | 800 | 14.2 | Yes |
| 14 | Amery(25) | WHO questioner | At a city ( Torbat Heydariyeh) | 2012 | 384 | 6.77 | Yes |
| 15 | Fazaeli (26) | SCI questioner | National | 2012 | 36551 | 2.85 | No |
| 16 | Rezapour (27) | WHO questioner | At a city (Tehran) | 2013 | 2200 | 6.54 | Yes |
| 17 | Bagheri Faradonbeh (28) | WHO questioner | At a city (Tehran) | 2014 | 625 | 3.8 | Yes |
| 18 | Ghafoori (29) | Researcher-made questioner | At a city (Tehran) | 2014 | 792 | 7.2 | No |
| 19 | Piroozi (30) | WHO questioner | At a city (Sanandaj) | 2015 | 663 | 4.8 | Yes |
Studies Included in Analysis
4.3. Overall Meta-Analysis
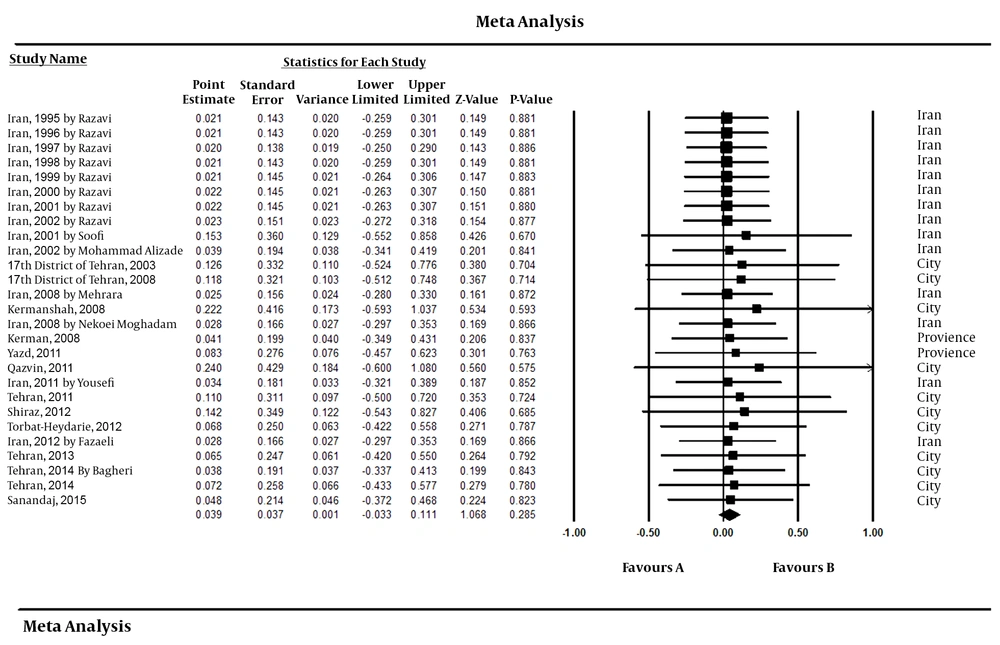
The results of 27 surveys in which the CHE in Iran was calculated were analyzed using meta-analysis. Accordingly, prevalence estimates from the included studies for CHE with random model estimate was 3.91% with a 95% confidence interval and equaled to -3.26% and 11.07%. The results of the random model corresponded to the results of the fixed model.
Based on the meta-analysis results and considering the insignificance of the chi-square test, and the positioning of the I-square value in the homogenous domain (0.001), no heterogeneity was observed. Therefore, the results of model estimates using the fixed and random models were the same (Figure 2).
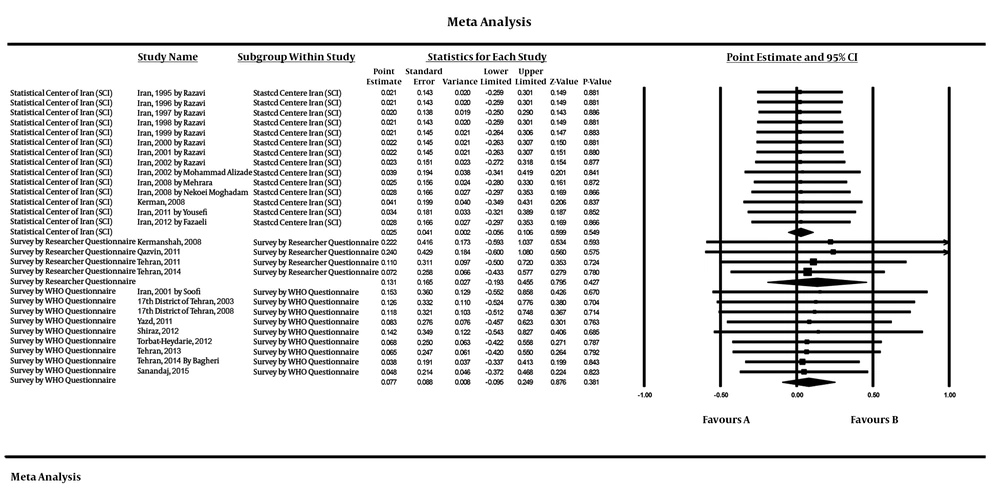
4.4. Subgroup Meta-Analysis by Data Sources and Tools
To assess the influence of study questionnaire for data collection, subgroup meta-analyses was performed. As displayed in Figure 3, in the SCI questionnaire group, 14 surveys were analyzed; and the pooled estimate of CHE in this group was 2.48% (95% confidence interval, CI: -5.64 - 10.61). In the subgroup of author-made questionnaire, 4 surveys were analyzed and the pooled estimate of CHE was found to be 13.14% (95% confidence interval, CI: -19.25 - 45.53). In the subgroup of the WHO questionnaire, the pooled estimate of CHE in 9 surveys was 7.71% (95% confidence interval, CI: -9.53 - 24.94). In all 3 cases, the results of the random model were the same as the results of the fixed model. The tests of heterogeneity, i.e., the results of chi-square test and the I-square test statistic showed no heterogeneity in the subgroups.
4.5. Subgroup Meta-Analysis by Scope (National- Province-City)
In the subgroup of studies at city level, 11 surveys have been analyzed, based on the pooled estimate of CHE in this group, which was 8.62% (95% confidence interval, CI: -7.66 - 24.89). In the studies at national level, 14 surveys were analyzed accordingly, and the pooled estimate of facing CHE in this group was 2.58% (95% confidence interval, CI: -5.66 - 10.83). In the subgroup of studies at provincial level, 2 surveys were analyzed, and the pooled estimate of facing CHE in this group was 5.54% (95% confidence interval, CI: -26.08 - 37.16). In each of these 3 cases the results of the random model estimate were the same as the results of the fixed model. The results of the fixed model were reported in all 3 cases. The tests of heterogeneity, i.e., the results of chi-square test, and the I-square test statistic revealed no heterogeneity in the subgroups.
4.6. Meta Regression by Year and Sample Size
According to the results of meta-regression method, sample size and year of survey had no significant effect on facing CHE.
4.7. Study Findings: Variables as Determinants of CHE
On the whole, 15 regression models were obtained from the studies, and the effects of 18 different variables on the possibility of facing CHE were examined in 2 or more studies. These variables were categorized into 4 groups (Table 2).
| No. | Factors as Determinants of CHE in 2 or More Studies | Total Studies that This Factor Analyzed as Determinant of CHE | Frequency of Studies with This Factor | ||
|---|---|---|---|---|---|
| Increased Likelihood of CHE | Decreased Likelihood of CHE | No Significant Impact | |||
| Demographic Characters of HHH: | |||||
| 1 | Increase in age of HHH: | 3 | 2 | 0 | 1 |
| 2 | Female HHH: (Female vs. Male) | 5 | 2 | 1 | 2 |
| 3 | Married HHH :(Married vs. Single) | 2 | 1 | 1 | 0 |
| 4 | Higher HH size: | 13 | 5 | 3 | 5 |
| Socioeconomics Characters of HH: | |||||
| 5 | HH with lower income: (Q1vs. Q5) | 11 | 5 | 2 | 4 |
| 6 | More members earn income in HH | 2 | 1 | 1 | 0 |
| 7 | Lake of insurance in HH: (Not Have vs. Have) | 15 | 7 | 0 | 8 |
| 8 | No employed HHH: (Employed vs. Not Employed) | 3 | 3 | 0 | 0 |
| 9 | Rural HH: (Rural vs. Urban) | 5 | 5 | 0 | 0 |
| 10 | Lower education of HHH: (low vs. High) | 8 | 5 | 1 | 2 |
| Special Person in HH: | |||||
| 11 | Have children in HH: (Have vs. Not Have) | 11 | 3 | 2 | 6 |
| 12 | Have elderly in HH: (Have vs. Not Have) | 11 | 5 | 0 | 6 |
| 13 | Have member with disability in HH: (Have vs. Not Have) | 3 | 2 | 0 | 1 |
| 14 | Have member with chronic or cardiac illness in HH: (Have vs. Not Have) | 4 | 3 | 0 | 1 |
| Health care Utilization by HH Members: | |||||
| 15 | Use inpatient service by HH members: (Have vs. Not Have) | 10 | 8 | 0 | 2 |
| 16 | Use outpatient service by HH members: (Have vs. Not Have) | 9 | 3 | 0 | 4 |
| Use outpatient service by HH members: (Frequency) | 2 | ||||
| 17 | Use dentistry service by HH members: (Have vs. Not Have) | 6 | 5 | 0 | 1 |
| 18 | Usage of drugs by HH members: (Have Drugs Costs vs. Not Have) | 4 | 4 | 0 | 0 |
| Total Logit Regression Models include in systematic review | 13 | ||||
Variables as Determinants of CHE
5. Discussion
The prevalence of CHE in Iran during 1997 and 2015 fluctuated from 1.97% (13) to 24% (21). Principally, the equity indexes such as CHE has a high inertia, and there is no possibility for immediate leaps in this index (13). Therefore, to identify reasons for this inconsistency, the questionnaire and scope of studies, and year and sample size of surveys, should be checked by the results of subgroup meta-analysis and meta-regression. The results revealed that the highest percentage estimate of facing CHE is associated with author-made questionnaires and the lowest is related to the SCI questionnaire. The SCI questionnaire is a general tool which is used every year to estimate the income-expenditure of households and was not designed specifically for the health sector, whereas the other 2 are specifically designed for health care systems. Gotsadze et al. (2009), relying on evidence from Georgia, also stated that those questionnaires that have been particularly designed to study household expenditures for health services are more accurate (31).
Another important finding of this study was summarizing CHE determinants. An overall examination of these variables shows that 11 of them, besides being ineffective, only increased the possibility of facing CHE, whereas 7 other variables had both increasing and decreasing roles.
In general, the variables, which have been ineffective or increased the possibility of facing CHE were as follow: having no health insurance, aging of the household head, unemployment of the household head, inhabitance of the household in the villages, having an elderly person in the household, having a disabled person in the household, having a household member who suffers from chronic or cardiac disease, and any use of health care services. On the other hand, 7 variables including lower income of the household, female household head, lack of education of household head, marital status of household head, the higher number of family members who have an income, more people in the household, and having a child in the household were among the factors that had both an increasing and a decreasing role in facing CHE in various studies.
Health insurance status is the only variable, whose effect on facing CHE was examined in all studies. Most of the studies indicated that having health insurance reduced CHE (12, 14-16, 20, 23, 24, 30). The purpose of acquiring health insurance is to gain financial security by accumulation and prepayment. Therefore, in nearly half of the studies having health insurance did not have a significant effect on reducing CHE (12, 13, 18-20, 27, 28). This, to some degree, shows the deficient function of insurance in Iran in which the cost coverage and service coverage are limited; moreover, as the payment franchise is high (29), it has even reduced the protective effect of insurance.
Aging of the household head also increased the possibility of facing CHE (15, 23). This variable can lead to households facing CHE by decreasing their ability to pay because of the weakened ability to work and lower income and by increasing heath expenditures due to their need for more care.
The unemployment of the household head increased the possibility of facing CHE (15, 16). Employment is an index of one’s socioeconomic situation. The inability of a household head to make income can be directly related to a decrease in the ability of payment of the household.
The households living in a village have an increased possibility of facing CHE (12-16). This could result from lack of facilities in the village, the money and time spent to use city services, or the indirect expenditure of staying in the city to use those services. On the other hand, it could also be caused by the lower ability of villagers to pay. Nevertheless, expensive private facilities in cities can also increase CHE (12).
Having an elderly person in the household increases the possibility of facing CHE (13, 16, 20, 23, 30). The elderly may need more expensive health care services. Also, in most of the reviewed studies, having a disabled person (14) or a person with cardiac or chronic diseases in the household increased the household’s possibility of facing CHE (12, 14, 23, 30). It seems that the presence of these people in the household, aside from imposing heath expenditures, resulted in other household members wasting their time and losing their opportunity to work and produce income.
In most of the studies, any use of health care services, e.g., hospitalization (12, 18, 20, 24, 28, 30), outpatient services (12, 14, 18), times of utilization of services (12, 27), dentistry services (12, 24, 25), and the cost of medicines (18, 20, 25) increased the possibility of facing CHE. It seems that the health care system in Iran has created less financial protection for those who are in need of such services. This situation is worse when one considers that the CHE index does not consider those households that have unmet needs.
In this systematic review, some factors increased the possibility of facing CHE, while in other studies they actually decreased it. Income seems to be one of the most effective factors in the possibility of facing CHE. In general, an examination of the effect of a household’s economic situation on the possibility of facing CHE revealed that the possibility of facing CHE is higher in low-income households (12, 14, 18, 24, 30). Clearly, since CHE is calculated based on the ability to pay, it is highly sensitive to the financial situation of a household. Only 2 studies revealed that the possibility of facing CHE was greater in high-income households (16, 23). This could have resulted from the fact that poor families usually refrain from using health care services, or use cheaper services in the public sector, or it could be a result of protective policies that mostly cover poor households (32).
The variable of female household head increased the possibility of facing CHE in 2 studies (23, 30) and decreased it in another (18). Therefore, it seems more appropriate to consider this variable as interacting with other variables such as education or place of residence (city or village) (33).
Low education level of the household head increased the possibility of facing CHE in some studies (13, 15, 23, 28). The reason for this was that educated people take more appropriate care of their health. They also use health and preventive care services more effectively. Moreover, it can be stated that households with economically-active heads (with a lower possibility of facing CHE) are mainly educated (32). However, the results of 1 study revealed that households with educated heads are more in danger of facing CHE (27). This can be a result of more awareness, more visits to health and medical centers, and more money spent on health care services.
In most of the studies, the higher number of household members increased the possibility of facing CHE (14, 16, 20, 25, 27), yet the results of some studies showed a decrease in the possibility of facing CHE (15, 18, 23). Therefore, the variable of household size should not be considered alone, when explaining the possibility of facing CHE; the variables such as average age of household members and the level of use of health care services need to be considered along with household size. Households with 1 and 2 members including single individuals or couples with an average age of 46 years or more should also be considered (34). On the other hand, people in more crowded households take care of each other, and this leads to a reduction in use of health care services by household members (35).
According to the results of several studies, the presence of a child (or children) increases the possibility of facing CHE (13, 16, 23). Children are more vulnerable to diseases and injuries than other age groups. Conversely, some studies revealed that the presence of children in a household had a protective role in facing CHE (20, 25). In a household with a preschool child, the parents are normally young, possibly healthier, and thus less likely to face CHE.
Various plans such as the health sector evolution plan (HSEP) (36) since 2014 were implemented in the Iranian health care system to reduce OOP payments; thus, one of the interventions of HSEP was reducing OOP payments just for inpatient services, and this plan does not cover outpatient services, which according to the results of this research, can increase the probability of facing CHE. It seems necessary to investigate the effect of this plan on household facing CHE in Iran. In this study, only 1 survey had used cross- sectional data after HSEP plan, thus, we could not use subgroup meta-analysis to investigate the effect of this plan.
5.1. Conclusion
Policymakers should consider that researchers may use different instruments to calculate CHE and have different results. Decreasing CHE level to less than 1%, the objective of 2 Iran’s five-year development plans (2007 - 2015), was not met in Iran. This percentage may need to be reconsidered according to the pooled estimate of CHE. The determinant factors of facing CHE in Iranian households revealed that some socioeconomic variables increase the possibility of facing CHE by lowering one’s capacity to pay and increasing the need so that interventions to influence these variables are not solely in the domain of the health sector, and some intersectoral collaboration must be taken to improve the welfare of the vulnerable groups.
It is suggested that households that are simultaneously affected by several factors of CHE be given priority. It is also recommended that in future studies the interactive effect of these variables in facing CHE be investigated to provide detailed information to administrators.