1. Background
Mental disorders are highly prevalent and have substantial burden among diseases. The global burden of disease for mental disorders, as measured by disability-adjusted life years (DALYs), was estimated to be 13% worldwide in 2005 and expected to reach 15% by 2020 (1, 2). Mental disorders are also the prime reason for DALYs in Iran so that they are responsible for 16% of the burden of disease in the country (3). According to the Iranian National Mental Health Survey (IranMHS) conducted in 2011, the prevalence of any mental disorder and severe mental disorders (SMDs) was about 24% and 1%, respectively, in the Iranian population (4).
The costs of mental disorders are substantial, which can be a great barrier to accessing care for patients with mental disorders (5). Health system financing is fair when health spending of the households is distributed based on their ability to pay rather than their own risk of illness. Some of the consequences of the unfair health system financing include facing catastrophic health expenditures (CHE) and sustainable medical impoverishment for households (6, 7).
Studies in Iran have reported that the incidence of CHE ranges from 1.97 to 15.3% at the national level, 3.6 to 24 % at the regional level, and 4.8 to 72.5% among specific groups (8-14). There is, therefore, still a gap between the goal of the Fifth Economic, Social, and Cultural Development Plan of Iran, which is to reduce the rate of households facing CHE to less than 1% (15). Accordingly, the health transformation plan (HTP) started in Iran’s health system in May 2014. The HTP is one of the largest health system reform programs in Iran with the aim of protecting citizens against health-related costs and vulnerable populations by organizing hospital services and reducing the share of out-of-pocket (OOP) health payments for households in hospitals affiliated to the Ministry of Health and Medical Education (MoHME) (16).
Obviously, the presence of a disease, especially a chronic and costly disease, is an important factor in increasing the number of households facing CHE. Although numerous studies have addressed the CHE in Iran and other countries (6, 10-29), many of them have concentrated on the general population rather than vulnerable groups and no previous study has investigated the CHE among households with mental disorders patients.
2. Objectives
The present study aimed to measure the CHE and analyze factors affecting CHE in households with SMDs patients after the implementation of the HTP. The findings of the current study can help health policymakers to formulate policies related to promoting financial protection against the expenditures of households with SMDs patients.
3. Methods
This cross-sectional study was conducted among households with SMDs patients who referred to the psychiatric hospitals for outpatient services from July 2017 to March 2018. The criteria for selecting the subjects were Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for schizophrenia, schizoaffective, or bipolar disorders based on the clinical diagnosis of the treating psychiatrist, age of above 18 years, informed consent for participation in the study, no co-morbidity with severe organic conditions, no addiction, and no mental retardation.
The sample was recruited from four university centers located in Tehran including all the three university psychiatric hospitals (Roozbeh Psychiatric Hospital, Iran Psychiatric Hospital, and Razi Psychiatric Hospital affiliated to Tehran University of Medical Sciences (TUMS), Iran University of Medical Sciences (IUMS), and University of Social Welfare and Rehabilitation Sciences (USWRS), respectively) and the Psychiatry Clinic of Imam Hussein General Hospital as the main psychiatric center affiliated to Shahid Beheshti University of Medical Sciences (SBUMS).
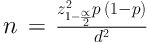
Considering α = 0.05, d = 0.05, and P = 15% (the percentage of households facing CHE in a study on the households of patients discharged from hospitals) (13), a sample of 196 households was needed, using the following formula:
However, to increase the precision of the study, 400 households were enrolled in the study. Therefore, 100 participants were consecutively selected from each hospital. The data were collected through interviews with the patient’s attendants, who were often family members, or the patients themselves if they were mentally capable of being interviewed.
3.1. Study Tools
The household section of a questionnaire entitled the World Health Survey was employed for data collection. The questionnaire was translated into Persian and its reliability and validity were verified by Kavosi et al. (17).
3.2. Measurement of the CHE and Its Determinants
The method considered by the WHO was used to measure the CHE. In this method, CHE occurs when a household’s OOP health payments equal or exceed 40% of its capacity to pay. Households' capacity to pay was derived from the deduction of households' subsistence expenditure from its total expenditure, as a surrogate of effective income. Using the food poverty line (a proportion of food expenditure to total household expenditure), each household’s subsistence expenditure was calculated. Xu describe the methodology of CHE measurement in details (6).
A forced-entry logistic regression technique was applied to assess the factors affecting the CHE. Therefore, the crude odds ratios (ORs) using the model coefficients were calculated and P-values of less than 0.05 were taken as statistically significant.
All statistical analyses were carried out using STATA version 14.0 software. The study protocol was approved by the Ethics Committees of TUMS. The participants were informed about the confidentiality of their information and voluntary participation in the study.
4. Results
Overall, 400 households were enrolled in the study. Most of the patients had bipolar disorder (235, 58.75%) and 165 had schizophrenia or schizoaffective disorders (41.25%). Other demographic variables of the participants and their household heads are shown in Table 1.
| Variables | Household Head, No. (%) | Patient, No. (%) |
|---|---|---|
| Age | ||
| ≤ 39 | 48 (12.00) | 235 (58.75) |
| 40 - 59 | 182 (45.50) | 143 (35.75) |
| ≥ 60 | 170 (42.50) | 22 (5.50) |
| Gender | ||
| Male | 315 (78.75) | 230 (57.50) |
| Female | 85 (21.25) | 170 (42.50) |
| Level of education | ||
| Illiterate | 70 (17.50) | 13 (3.25) |
| Primary school | 101 (25.25) | 41 (10.25) |
| Middle school | 73 (18.25) | 84 (21.00) |
| High school | 116 (29.00) | 187 (46.75) |
| University | 40 (10.00) | 75 (18.75) |
| Marital status | ||
| Single | 27 (6.75) | 195 (48.75) |
| Married | 274 (68.50) | 127 (31.75) |
| Other (divorced, widowed, etc.) | 99 (24.75) | 78 (19.50) |
| Basic health insurance status | ||
| Yes | 381 (95.25) | 382 (95.50) |
| No | 19 (4.75) | 18 (4.50) |
| Supplementary health insurance status | ||
| Yes | 121 (30.48) | 81 (20.30) |
| No | 276 (69.52) | 318 (79.70) |
Table 2 presents the rate of facing CHE and mean OOP health expenditures of the households according to hospitals. As the results show, 103 (25.75%) households with SMDs patients faced CHE.
| Hospital | Percentage of Households Facing CHE | Mean OOP Health Expenditure (SD), $ |
|---|---|---|
| Roozbeh | 35 | 128 (176) |
| Iran | 24 | 130 (184) |
| Imam-Hussein | 18 | 103 (125) |
| Razi | 26 | 136 (284) |
| Total | 25.75 | 124 (200) |
Table 3 shows the relationship between households facing CHE and study variables. The results of the logistic regression model demonstrated that the age range of 40 to 59-years-old for the household heads was a protective factor against experiencing CHE (OR = 0.283). The results also showed that with a rising education level of the household head, the likelihood of facing CHE decreased. Moreover, there were statistically significant relationships between the chance of facing CHE and the utilization of dental (OR = 12.38), rehabilitation (OR = 6.99), and medication (OR = 3.17) services. Households in the higher economic quintile were less likely to face CHE compared to households in the lower economic quintile so that with increasing the households' monthly expenditure, the likelihood of facing CHE decreased. There were no significant relationships between facing CHE and other demographic variables such as the place of residence, the household size, gender, job, marital status, and supplementary health insurance status. The Hosmer-Lemeshow test results indicated that the goodness-of-fit was satisfactory.
| Variables | Faced with CHE, No. (%) | Odds Ratio | P > |z| | 95 %CI | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Dependent variable | |||||
| CHE (1 = Facing CHE; 0 = Otherwise) | |||||
| Independent variables | |||||
| Age of the household head | |||||
| ≤ 39b | 17 (35.42) | 31 (64.58) | |||
| 40 - 59 | 38 (20.88) | 144 (79.12) | 0.283 | 0.049 | 0.081 - 0.995 |
| ≥ 60 | 48 (28.24) | 122 (71.76) | 0.488 | 0.370 | 0.101 - 2.35 |
| Education status of the household head | |||||
| Illiterateb | 26 (37.14) | 44 (62.86) | |||
| Primary school | 28 (27.72) | 73 (72.28) | 0.536 | 0.204 | 0.205 - 1.40 |
| Middle school | 20 (27.40) | 53 (72.60) | 0.449 | 0.170 | 0.143 - 1.41 |
| High school | 22 (18.97) | 94 (81.03) | 0.215 | 0.010 | 0.067 - 0.690 |
| University | 103 (25.75) | 297 (74.25) | 0.075 | 0.002 | 0.015 - 0.377 |
| Utilization of dental services | 5.60 - 27.35 | ||||
| Nob | 61 (19.43) | 253 (80.57) | |||
| Yes | 42 (48.84) | 44 (51.16) | 12.38 | 0.000 | |
| Utilization of rehabilitation services | 1.54 - 31.72 | ||||
| Nob | 90 (24.26) | 281 (75.74) | |||
| Yes | 13 (44.83) | 16 (55.17) | 6.99 | 0.012 | |
| Utilization of medications | 1.00 - 10.01 | ||||
| Nob | 3 (7.69) | 36 (92.31) | |||
| Yes | 100 (27.70) | 261 (72.30) | 3.17 | 0.049 | |
| Household expenditures quintile | |||||
| Quintile 1b | 31 (38.75) | 49 (61.25) | |||
| Quintile 2 | 20 (24.69) | 61 (75.31) | 0.236 | 0.002 | 0.095 - 0.586 |
| Quintile 3 | 20 (25.32) | 59 (74.68) | 0.251 | 0.004 | 0.098 - 0.640 |
| Quintile 4 | 16 (20) | 64 (80) | 0.841 | 0.000 | 0.028 - 0.253 |
| Quintile 5 | 16 (20) | 64 (80) | 0.111 | 0.000 | 0.039 - 0.319 |
a LR chi2 (49) = 131.26, Log likelihood = -159.69217, Prob > chi2 = 0.0000, Pseudo R2 = 0.2913. Hosmer-Lemeshow goodness-of-fit test, Prob > chi2 = 0.8423, Number of observations = 394.
b Reference group.
5. Discussion
Based on our measurement, 103 (25.75%) households with SMDs patients referring to four university hospitals located in Tehran were experiencing CHE. The high percentage of households facing CHE indicates that there is a long way to attain the goals of the HTP and the Iranian Development Plan to decrease the percentage of households facing CHE. This result is somehow consistent with the finding of Moradi et al. study in Kurdistan province, Iran, conducted after the implementation of the HTP. They found that the rate of CHE among households with MS patients was 20.6% (14). Moreover, the results of a study carried out in Sistan and Baluchistan province, Iran, after the HTP implementation indicated that the goals of Iranian development plans have not been attained in this context (7). However, some studies showed that the percentage of exposure to CHE declined in Iran after the HTP (10, 11, 21). Moreover, studies by Limwattananon et al. (20) and Yardim et al. (18) in Thailand and Turkey, respectively, showed that the rate of households facing CHE decreased after domestic health reform plans.
There are several possible explanations for the high percentage of facing CHE in households with SMDs patients even after the implementation of the HTP. A possible explanation is that patients referring to government health centers often belong to households with middle to low socioeconomic status. Moreover, as the 2011 Iran MHS showed, mental disorders imposed a significant economic burden on households (4). Therefore, it is expected that facing CHE would account for a high percentage of households with SMDs patients referring to government health centers. Another explanation might be that the HTP concentrates chiefly on decreasing OOP payments for inpatient healthcare services, and it does not sufficiently cover outpatient healthcare services. On the other hand, increased tariffs of medical services in the third phase of the HTP led to an escalation in the monetary value of OOP payments.
Our findings showed that the mean OOP health expenditure for participants was $ 124. Two previous studies conducted after the HTP reported this figure as $ 24 and $ 39 (10, 14). However, these figures are lower than what a study reported before the HTP (13). A survey carried out by Somkotra and Lagrada on Thai households also showed a decrease in OOP health payments after UHC reforms (22).
According to the results, the age of the household head lower than 40 years increased the risk of households facing CHE. A similar finding was reported in Moradi et al. study (14). A possible explanation may be that younger individuals have lower income and asset and therefore, have a greater risk of experiencing CHE. However, some studies reported a directly statistically significant relationship between the age of the household head and the risk of experiencing CHE (23, 27).
Our study showed a statistically significant association between the low education level of the household head and the chance of facing CHE. This finding is confirmed by other studies (13, 14). The more effective utilization of health and preventive care services by educated households can be a reason for this observation. Additionally, it could be declared that an economically active household head (with a lower likelihood of facing CHE) is mostly an educated one (24).
The findings demonstrated that exposing to CHE was 12.4 and 7 times higher in households using dental and rehabilitation services than in households not using the services, respectively. These findings are also confirmed by other studies (14, 17, 21, 28). In Iran, dental and rehabilitation services are of expensive healthcare services while these are not appropriately covered by basic health insurance organizations and thus, households should pay more OOP for them.
As the findings of the study showed, the chance of households for experiencing CHE was 3.17 times greater among those taking medications than among those not taking. This finding is supported by Juyani et al. study (29). The chronic, long-term nature of mental disorders leads to high expenditures of pharmacological treatment over time imposed on households; consequently, it could be a possible reason for the high percentage of facing CHE in these households.
Based on the study results, as supported by other studies (10, 13, 14, 18, 25, 26), there was an inverse relationship between facing CHE and increasing rank of economic quintiles among households. However, the findings of a study by Somkotra and Lagrada in 2009 disclosed that following the implementation of UHC in Thailand, CHE shifted from poor to rich households (24).
The study has some limitations. Since we measured the CHE for households with SMDs patients referring to four university hospitals located in Tehran, the generalizability of the findings to other settings or the whole country may be limited. Moreover, those who were more compliant had more chance to be included in this study. In fact, it would be a better procedure for sampling to randomly call households with SMDs patients referring to the psychiatric centers for both outpatient and inpatient services. Furthermore, the data were collected through interviews with patients or their relatives, which may be subject to recall bias.
5.1. Conclusions
In our study, approximately 26% of households with SMDs patients faced CHE. Facing CHE remains a challenge for these households even after the implementation of HTP. Often, poor people bear the higher burden of mental disorders, with regard to both the risk of having an SMDs patient and less access to treatment. Having less access to affordable treatment makes the course of the disease more severe and debilitating, causing a vicious circle of poverty and mental health disorder that is rarely broken. Therefore, further research to investigate the economic burden of mental disorders is required in Iran.