1. Background
Health care delivery is one of the main functions of the health system to improve people’s health conditions. For this purpose, people should be at the center of attention by health services, because as a user, they make a choice for using health care to influence their health (1).
Health equity in has been a complicated issue. Whitehead (2) defines it as equality of access to health care for equal needs, equal utilization for equal needs, and equal quality of care for all. In addition, it is divided by Egalitarian equity goals into two distinct items, including horizontal and vertical equity. The former focuses on the equal treatment of equals, i.e. people with the same need should receive the same services, whereas the latter emphasizes on the appropriate unequal treatment of unequals, i.e., people with different health care needs should receive different suitable and qualified services (3). In health care research and policy, horizontal equity has been focused more than vertical equity. The main principle of horizontal equity indicates that people who need health care services should receive the same service for a similar need regardless of their color, race, ethnicity, socioeconomic level, etc.
It is not only important to use health care by people who need such services, but the main responsibility of the health care system is to ensure how they use such facilities. The difference in using health services in different social groups, such as economic classes has been a concern. For example, an increase in the gap between the poor and rich people makes the issue unfair. Governments should secure equitable health care access and utilization by organizational arrangements in their health care systems. How such services are organized and delivered to different people and how different they use the services should be the governments and policymakers’ concern (1). Equitable distribution of health care has been considered as a value in legislation in several countries (3). They try to achieve this through reforms (4-6), and quantification of the inequalities in using health care to follow the changes after these reforms.
Many studies have focused on horizontal inequality and inequity of health care utilization (3). Some studies have made cross-country comparisons to reveal the differences in equity between countries (7, 8). Other studies have evaluated the effects of a special policy on health care utilization and its resulted consequences (6, 9-11). Few studies have focused on the health care system and measured health inequality and equity in both outpatient and inpatient care, and also in public and private sectors, as well (12-21).
A few studies have examined health care utilization inequity in Iran (22-26), most of which have measured health inequalities in different health care services (27-31). Most of these studies have evaluated subnational data, therefore, their data cannot be used at the national level (25, 26, 32). Other studies in Iran have not measured the differentiation between public and private sectors (27, 33). None of these studies has examined all aspects of health care delivery in detail and in public and private sectors, as well.
Considering the availability of health care utilization inequalities or differential utilization of health care services by people in different socioeconomic levels with the same need, and compare it with other countries, using an internationally accepted method seems necessary. This assessment tool should be comprehensive and include all aspects of the health care delivery system. In this study, we used the data from a nationally representative survey to examine health care utilization inequalities in both public and private sectors by outpatient and inpatient health services. Key results of this measurement can be helpful in both policy implication and evaluation and provide a baseline for assessing the effects of new reforms.
1.1. Health Care Delivery in Iran
Iranian health care delivery system involves a mixture of public and private provisions. Primary health care is free and is delivered by the public sector. Secondary and tertiary health services are not free and are provided by both the public and private sectors (34).
The Ministry of Health and Medical Education (MOH) manages national health policies in Iran through the National Five-Year Development Plan (NFYDP). Some issues about health equity and equitable access were pointed in the fourth (2005 - 2009) and fifth (2011 - 2014) NFYDP by MOH. At the provincial level, medical universities handle the public health sector and supervise the private sector on behalf of the MOH. All primary health care (PHC) centers and university hospitals deliver health services to people. In addition, the private health sector brings medical services to the community typically by private hospitals and clinics (35).
National Health Insurance Council (NHIC) in MOH sets medical tariffs for the public and private sectors annually and coordinates all health insurance systems in the country. Different health insurance companies introduce multiple insurance schemes to people. Governmental Medical Services Insurance Organization (MSIO), newly named the Iranian Health Insurance, covers the government, public employees and all rural population, as well. Social Security Organization (SSO) manages the labor force, and the Army Medical Service Insurance Organization (AMSIO) covers military personnel with their families. Imam Khomeini Foundation (IKF) also targets poor people for medical services expenditure (34).
Generally, copayments are introduced by the tariff system for outpatient and inpatient services about 30% and 10% of the patient bills, respectively. It is the same for both public and private facilities. Insured people can use health services in both public and private sectors without limitation, but the insurance organization just pays or reimburses based on the pre-designed benefit package by the schemes (36). SSO, Ministry of Oil, and some other organizations own their facilities and provide free health services to the eligible population. On the other hand, people with no insurance coverage should pay the entire bill by themselves.
Iran has implemented different reforms during the last ten years. Rural FP, rural health insurance, urban FP and the newly established Health Transformation Plan (HTP) are the most important reforms in the health care system in Iran. Rural FP program targets the PHC in the rural areas, and urban FP program was tested in two provinces, providing PHC to the urban population. Along with these programs, MOH established the referral system with some incentives for public health care facilities and users, as well. The aim of HTP is increasing basic health insurance coverage (toward universal health coverage), reducing out-of-pocket (OOP) payments for inpatient services at the MOH hospitals, financial support for specific diseases, improving the quality of specialist outpatient services in university hospitals, providing financial support for poor people, and making normal vaginal delivery free in MOH hospitals (37, 38). The main common basis of all these reforms is to improve health equity through reducing heath inequalities. Thus, measuring health inequality in health care utilization is essential in evaluating these reforms.
2. Methods
2.1. Data
In this cross-sectional survey, data derived from the national Utilization of Health Services Survey (UHSS) in 2014 were used for assessing the demand and utilization of the health services in Iran during 2013 - 2014. It was designed based on the Anderson model (39) and done by the Statistical Center of Iran (SCI) (40). In the UHSS, 22470 households (15360 urban and 7110 rural) were participated using three-stage stratified random sampling method. In the survey, two questionnaires were used and the trained personnel collected the data through interviews. The household questionnaire assessed all members of a household with individuals' characteristics, such as gender, age, education, occupation, marital status, basic and complementary insurance, and finally feeling the need for outpatient or inpatient care. The questionnaire did not contain information about household income or expenditure. However, household assets were asked, such as owning a house, the location of the house, and having facilities, like the car, motorcycle, computer, internet, a kitchen in the house, telephone, and central package.
The questionnaire contained questions about the needs for health care, efforts made to receive health services, and the health services received sequentially. In outpatient services, up to ten subjects received care from any provider recorded for each need. For the first need, except for the need for pharmacy, laboratory and para-clinical services, the three last referrals to the providers were listed. The information about the three last hospital admissions was recorded in detail. Overall, the people were asked about outpatient and inpatient health services used during the last two weeks and the last 15 months (from the last autumn), respectively (40).
For the utilization measure, the number of doctor visits by a FP, general practitioner (GP) and specialist (SP) was used as the outpatient services. Inpatient services included the number of inpatient admissions to the hospitals. All these services, as dependent variables, were separated into the public and private facilities utilization. The hospital admissions during 2013, i.e., data related to the first six months, were excluded from the study. It should be noted that all variables were adjusted for one year by multiplying outpatient variables by 26 and inpatient variables by 12/9. Some independent variables included age, gender, place of residence, education, occupation, marital status, type of insurance, having complementary insurance, and being women as the head of the household. Age was categorized based on the MOH age categorization into five age groups, and all the utilization variables were adjusted for the one-year duration.
The household assets were used to construct the asset index as a proxy for household socio-economic status (SES) by principal component analysis (PCA) (41, 42). We tested the suitability of the variables by Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (0.706) and Bartlett test of sphericity (χ2 = 11000, P < 0.00). The households were ranked in decile and the pre-defined sample weight was used for the health care utilization distribution.
2.2. Statistical Analysis
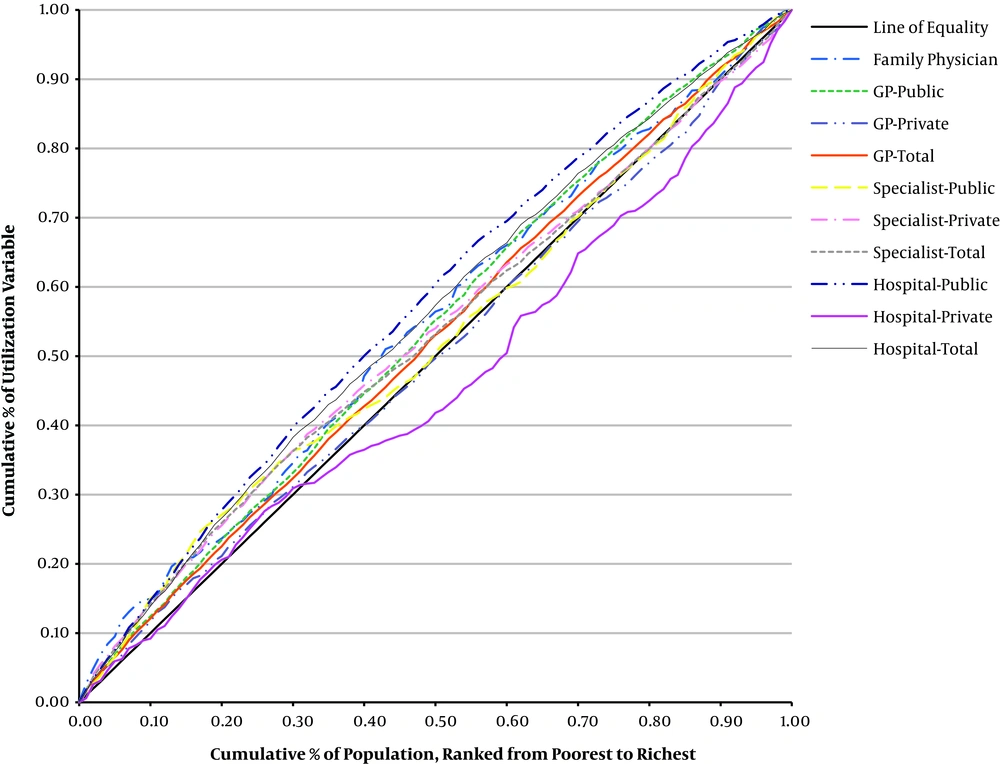
To measure inequality in the health utilization, we used concentration curve (CC) and concentration index (CI), based on the World Bank guideline (3). The CC plots the shares of health variable compared with the socio-economic condition ranked from the poorest to the richest. If all people in a sample have the same value of the variable, the curve will be on the 45-degree line (the equality line). However, for the high or low variable, for example in poor people, the curve will be on the top or bottom of the equality line, respectively. Thus, CC shows how the health variable concentrates on the poor or rich, but it cannot display the magnitude of inequality.
The CI, based on CC can quantify the inequality in health variables. It is defined as twice the area between the CC and the line of equality. The index is bounded between -1 and 1 and for no inequality, it is zero. A curve above the equality line has a negative value, indicating that equality in healthcare utilization is focused on the poorer people. When CC lies below the line of equality, it takes a positive value and shows the concentration on rich people. Its scale reveals the magnitude of the relationship between health variables and living standards distribution and also, the sign of CI shows the direction of this relationship.
The CI is defined as:
In this formula hi is the health variable, µh is the mean of health variable, and ri = i/N represents individual i fractional rank in the socioeconomic distribution. For the poorest and richest people, i is considered 1 and N, respectively. The CI depends only on the association between the health and the SES rank. It is not affected by the variations in the level of SES inequality. The extended CI and health achievement index were used for a more detailed explanation and a better understanding of CI in this study. Overall, when calculating standard CI, the poorest individual takes a weight close to 2 and the richest one takes a weight close to 0. It is possible to change this weighting by setting the value of an inequality-aversion parameter using the “extended CI” which is equal to the CI when the parameter is equal to 2. The poor individuals get greater weights when the parameter is increased to 3 and 4, and these weights decrease faster than reaching linearly 0, for the richest ones.
On the other hand, in the present study, the achievement index was also tested. The achievement index is a measure of the average health focusing on the health inequality. Accordingly, the greater the health inequality, the smaller the achievement index. The achievement index is equal to the average health multiplied by factor 1 minus the extended CI. It is sensitive to the degree of aversion to inequality and the corresponding aversion parameter (3).
Two distinct methods (direct and indirect) are available to standardize the health care utilization. The former needs group data, whereas the latter needs microdata. We had micro-data and an indirect method was used. Below is the indirect method formula:
Where, health utilization is yi , the individual is i, and the parameter vectors are α, β, γ. Health care utilization is standardized by the confounding variables (xj) for age and gender. The non-confounding variables (zk), for which CI was not standardized, were used in order to estimate the partial correlations with the confounding variables. Binary non-confounding variables, like being educated or illiterate, women as a head of household, being employed, being married, being poor or rich (by income decile) and having basic and complementary insurance were applied for this purpose. Regression estimates (
Through the difference between actual and x-expected utilization, the standardized health can be indirectly estimated by adding the overall sample mean (
We can interpret the distribution of
3. Results
Table 1 shows the summary of basic data and variables used in the analysis. It is obvious from the last column that, we had binary variables, such as gender, urban/rural residency and our utilization variables were count data. Moreover, there was no missing data.
As Table 1 shows, there were 21697 households with 78378 individuals in the survey dataset. Most of the studied individuals lived in the urban areas (67%), and were in the decile 4 (10.8%), male (50.7%), in the middle age group (30 - 59 years) (39.57%), illiterate (13.7%), and unemployed (72.7%). Also, most of them had SSO health insurance coverage (39.7%), but they did not have complementary health insurance coverage (83%). The number of their visits and hospital admissions in the studied year is provided in Table 1, which shows the main utilization variables with the same frequency and without missing values.
Table 2 provides the summary of specified health utilization variables. This table displays the households' characteristics and shows the mean number of outpatient visits and inpatient admissions. The standard errors of the mean and frequency were removed to decrease the used statistical measures.
Iranian people had 0.246 FP visits, 1.521 public GP visits, 0.936 private GP visits, 0.529 public SP visits, and 1.612 private SP visits during 2014. They were admitted 0.056 and 0.012 times during this year into the public and private hospitals, respectively. The total GP visits (2.468) were more than that SP visits (2.145) and the total hospital admission was 0.069 during the studied year.
| No. (%) | Mean | Min | Max | Nunique | |
|---|---|---|---|---|---|
| Households' Characteristics | |||||
| Households | 78378 | 21697 | |||
| Urban/rural | 1.3 | 1.0 | 2.0 | 2 | |
| Urban | 52520 (67.0) | ||||
| Rural | 25858 (33.0) | ||||
| Living standards measure | 0.1 | -3.0 | 2.5 | 21170 | |
| Decile 1 | 8325 (10.6) | ||||
| Decile 2 | 8192 (10.5) | ||||
| Decile 3 | 8333 (10.6) | ||||
| Decile 4 | 8442 (10.8) | ||||
| Decile 5 | 8205 (10.5) | ||||
| Decile 6 | 8091 (10.3) | ||||
| Decile 7 | 7436 (9.5) | ||||
| Decile 8 | 7552 (9.6) | ||||
| Decile 9 | 7343 (9.4) | ||||
| Decile 10 | 6459 (8.2) | ||||
| Insurance | 3.2 | 1.0 | 9.0 | 8 | |
| MSIO | 12199 (15.6) | ||||
| Rural | 19404 (24.8) | ||||
| SSO | 31134 (39.7) | ||||
| AMSIO | 2547 (3.2) | ||||
| IKF | 703 (0.9) | ||||
| Others | 5062 (6.5) | ||||
| Uninsured | 7083 (9.0) | ||||
| Complementary insurance | 2.5 | 1.0 | 8.0 | 3 | |
| Yes | 13353 (17.0) | ||||
| Individuals’ Characteristics | |||||
| Gender | 1.5 | 1.0 | 2.0 | 2 | |
| Male | 39721 (50.7) | ||||
| Female | 38657 (49.3) | ||||
| Age | 31.7 | 0.0 | 99.0 | 100 | |
| 0-5 (child) | 6696 (8.54) | ||||
| 6-18 (juvenile) | 15967 (20.37) | ||||
| 19-29 (young) | 16494 (21.04) | ||||
| 30-59 (middle age) | 31016 (39.57) | ||||
| > 59 (old) | 8205 (10.47) | ||||
| Education | 23.0 | 0.0 | 71.0 | 11 | |
| Illiterate | 10759 (13.7) | ||||
| Occupation | 2.4 | 0.0 | 6.0 | 7 | |
| Employed | 21359 (27.3) | ||||
| Main variables (numbers of) | |||||
| FP visit | 78378 | 0.22 | 0.0 | 208.0 | 7 |
| GP visit-public | 78378 | 1.64 | 0.0 | 182.0 | 8 |
| GP visit-private | 78378 | 0.89 | 0.0 | 130.0 | 6 |
| GP Visit | 78378 | 2.5 | 0.0 | 182.0 | 8 |
| SP visit-public | 78378 | 0.48 | 0.0 | 156.0 | 6 |
| SP visit-private | 78378 | 1.65 | 0.0 | 260.0 | 8 |
| SP visit | 78378 | 2.1 | 0.0 | 260.0 | 9 |
| Hospital admission-public | 78378 | 0.1 | 0.0 | 4.0 | 4 |
| Hospital admission-private | 78378 | 0.0 | 0.0 | 4.0 | 4 |
| Hospital admission | 78378 | 0.1 | 0.0 | 4.0 | 4 |
Regarding rural-urban area of residence, rural residents referred to the FPs (0.379 vs. 0.196) and GPs in public sector (1.936 vs. 1.362) more than urban residents, however urban residents referred to the private GPs (0.987 vs. 0.802), public SPs (0.617 vs. 0.298) and private services (1.682 vs. 1.429) more than rural residents. Urban and rural residents referred to public hospitals more than the private ones, and those living in urban areas used private hospitals more than the rural subjects. Rural residents had GP visits and hospitalization more than those living in urban areas, whereas they had less SP visits; in contrast, urban residents had more SP visits.
People with different insurance schemes used outpatient and inpatient services differently. Those with no insurance used the least services in all groups. Subjects who had complementary insurance used private GPs, SPs and hospital services slightly more than those with no insurance coverage. Distribution of health care utilization by decile, as a factor of socioeconomic status of the household, in the utilization of some services was straightforward. For example, the utilization of FP services decreased from lower to upper deciles. It was the same for GP visits in the public sector and SP visits, as well. In contrast, GP visits in the private sector showed a none-normal pattern affected by deciles. Distribution of the admission in public hospitals decreased from lower deciles to upper ones, however in the private hospitals, it was associated with deciles, however, it showed a none-normal pattern. In total, GP and SP visits like hospital admission decreased in the same none-normal pattern.
Table 3 displays health care utilization according to the individuals’ characteristics. Women used all types of health care services more than men. For example, they had 2.052 private SP visits, but men had 1.183 visits during this year. Age is a continuous variable, however it was categorized into different groups. Lower ages, especially those fewer than 5 years old and over 59 years old, used GP services more than other age groups. In addition, the middle-aged group (30 - 59 years old) used SP visits and hospitalization more than others, but less than the old age group. Illiterate people used most of the services more than literate subjects and graduated people used the minimum services. Employment status did not show a clear relationship with health services usage.
Table 4 shows health care utilization according to the socioeconomic status (i.e., income decile). This distribution was not standardized by demographic factors, like age and gender. The number of FP visits in the first decile was 0.367, which decreased toward the upper decile.
| FP | GPa | SPa | Hospitalb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Public | Private | Total | Public | Private | Total | Public | Private | Total | ||
| Place of residence | ||||||||||
| Urban | 0.196 | 1.362 | 0.987 | 2.365 | 0.617 | 1.682 | 2.304 | 0.053 | 0.014 | 0.068 |
| Rural | 0.379 | 1.936 | 0.802 | 2.739 | 0.298 | 1.429 | 1.729 | 0.065 | 0.006 | 0.072 |
| Insurance | ||||||||||
| MSIO | 0.267 | 1.299 | 1.026 | 2.342 | 0.584 | 2.141 | 2.726 | 0.055 | 0.016 | 0.072 |
| Rural Ins. | 0.448 | 1.843 | 0.766 | 2.611 | 0.271 | 1.320 | 1.592 | 0.062 | 0.004 | 0.066 |
| SSO | 0.211 | 1.638 | 0.993 | 2.641 | 0.643 | 1.659 | 2.309 | 0.057 | 0.014 | 0.072 |
| AMSIO | 0.104 | 1.657 | 0.914 | 2.578 | 1.019 | 1.977 | 2.996 | 0.070 | 0.024 | 0.097 |
| IKF | 0.285 | 2.056 | 1.721 | 3.777 | 0.558 | 1.739 | 2.297 | 0.085 | 0.008 | 0.093 |
| Others | 0.138 | 1.231 | 0.982 | 2.242 | 0.671 | 1.857 | 2.551 | 0.065 | 0.011 | 0.078 |
| Uninsured | 0.045 | 0.822 | 0.852 | 1.693 | 0.244 | 0.936 | 1.180 | 0.025 | 0.016 | 0.041 |
| Complementary insurance | ||||||||||
| Yes | 0.288 | 1.439 | 1.171 | 2.629 | 0.758 | 2.282 | 3.046 | 0.060 | 0.031 | 0.093 |
| No | 0.267 | 1.633 | 0.904 | 2.545 | 0.505 | 1.539 | 2.048 | 0.059 | 0.007 | 0.067 |
| Unknown | 0.054 | 0.976 | 0.757 | 1.751 | 0.311 | 0.994 | 1.305 | 0.036 | 0.007 | 0.045 |
| Total | 0.246 | 1.521 | 0.936 | 2.468 | 0.529 | 1.612 | 2.145 | 0.056 | 0.012 | 0.069 |
aPer capita visit.
bPer capita admission.
The CI for FP visits was slightly negative (-0.088), indicating that poor people used it more than rich people. Regarding GP visits in public facilities, its distribution was similar to FP with a slightly negative CI (-0.077). Although private GP visits were not associated with deciles, a significant relationship was found between socioeconomic status and the CI (0.001). It means that the poor and rich participants used this service equally. Total GP visit was decreased with decile and indicating a pro-poor distribution (-0.042).
SP visits in both public and private sectors and in total did not follow a clear pattern, but they decreased from low decile toward upper decile accompanied by random fluctuations. However, the CI of these services was slightly negative (-0.042 and -0.060, -0.055, respectively), showing a pro-poor distribution. Public hospital services decreased from 0.083 to 0.031, from lower to upper deciles, and supported the strong negative CI (-0.145). These services showed a pro-poor distribution. On the other hand, private hospital services increased with deciles, but did not show a normal pattern and had a positive CI (0.077). The total hospital admissions showed the pattern similar to the public ones indicating a pro-poor distribution (-0.108).
| FP | GP | SP | Hospital | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Public | Private | Total | Public | Private | Total | Public | Private | Total | ||
| Gender | ||||||||||
| Male | 0.185 | 1.309 | 0.811 | 2.133 | 0.432 | 1.183 | 1.620 | 0.050 | 0.008 | 0.059 |
| Female | 0.309 | 1.738 | 1.064 | 2.812 | 0.628 | 2.052 | 2.685 | 0.063 | 0.015 | 0.079 |
| Age | ||||||||||
| 0 - 5 (child) | 0.378 | 2.466 | 1.427 | 3.900 | 0.575 | 1.664 | 2.247 | 0.053 | 0.005 | 0.058 |
| 6 - 18 (juvenile) | 0.184 | 1.474 | 0.849 | 2.332 | 0.269 | 0.773 | 1.045 | 0.023 | 0.003 | 0.027 |
| 19 - 29 (young) | 0.174 | 0.966 | 0.696 | 1.670 | 0.276 | 0.983 | 1.267 | 0.050 | 0.009 | 0.060 |
| 30 - 59 (middle age) | 0.249 | 1.444 | 0.915 | 2.376 | 0.618 | 1.828 | 2.450 | 0.057 | 0.014 | 0.072 |
| > 59 (old) | 0.390 | 2.263 | 1.270 | 3.538 | 1.132 | 3.532 | 4.667 | 0.131 | 0.028 | 0.161 |
| Education | ||||||||||
| Illiterate | 0.414 | 2.326 | 1.196 | 3.544 | 0.853 | 2.971 | 3.826 | 0.109 | 0.012 | 0.123 |
| Under diploma | 0.225 | 1.557 | 0.845 | 2.412 | 0.516 | 1.370 | 1.891 | 0.053 | 0.008 | 0.062 |
| Diploma | 0.178 | 0.949 | 0.845 | 1.802 | 0.417 | 1.446 | 1.867 | 0.047 | 0.018 | 0.066 |
| Graduated | 0.176 | 0.863 | 0.834 | 1.710 | 0.390 | 1.346 | 1.747 | 0.031 | 0.017 | 0.048 |
| Occupation | ||||||||||
| Under 15 years old | 0.275 | 2.017 | 1.143 | 3.171 | 0.404 | 1.152 | 1.561 | 0.033 | 0.003 | 0.037 |
| Employed | 0.162 | 1.105 | 0.734 | 1.848 | 0.381 | 1.150 | 1.535 | 0.042 | 0.009 | 0.051 |
| Looking for a job | 0.083 | 0.677 | 0.673 | 1.350 | 0.360 | 1.126 | 1.486 | 0.046 | 0.008 | 0.055 |
| With income | 0.316 | 2.106 | 1.051 | 3.170 | 1.097 | 3.068 | 4.165 | 0.115 | 0.028 | 0.145 |
| Student | 0.147 | 0.909 | 0.548 | 1.478 | 0.196 | 0.696 | 0.892 | 0.018 | 0.007 | 0.026 |
| Homeworker | 0.361 | 1.869 | 1.122 | 3.005 | 0.793 | 2.587 | 3.390 | 0.089 | 0.020 | 0.110 |
| Others | 0.294 | 1.179 | 1.141 | 2.331 | 0.759 | 1.669 | 2.427 | 0.105 | 0.014 | 0.120 |
| Total | 0.246 | 1.521 | 0.936 | 2.468 | 0.529 | 1.612 | 2.145 | 0.056 | 0.012 | 0.069 |
The extended CI with inequality aversion parameter of 3 and 4 showed that, all outpatient services were more negative by increasing the aversion to inequality. It means that more weight of the first decile than the last decile made it more negative, because of a higher average of utilization in the first decile. Public hospital services and total hospital admissions showed the same pattern, but changing inequality aversion did not affect private hospitals. The achievement index for most of the services was higher than that of the average of health utilization. In these cases, CI was negative and when weight was given to the poorest individuals, it showed a higher utilization, which indicated that the poor individuals used these services more than rich cases. Private hospitals showed the same pattern, and the achievement index in cases using these facilities was not affected by the rises in the inequality aversion parameter. In other words, when weight was given to the poorest individuals, private hospital utilization did not change. It means that the rich individuals used such services more than the poor participants.
Tables 4 and 5 are similar, but Table 5 contains the CI standardized for demographic factors, like age and gender. Comparison between the non-standardized and standardized CI revealed a small change in the FP and public GP services CI (-0.088 to -0.089 and -0.077 to -0.086, respectively). It means that standardization did not affect the CI of these two services. The CI of private GPs changed from a positive value (0.001) to a negative value (-0.010), which in contrast to the public SP, that changed from a negative value (-0.042) to a positive value (0.025). Using the need-standardized healthcare utilization, private GP services became pro-poor and public SP distribution changed toward a pro-rich distribution. The CI for total GP visits changed more negatively (-0.047 to -0.057), whereas it became less negative for the total SP visits (-0.055 to -0.007). It means that using the need-standardized healthcare utilization, the former showed more pro-poor distribution, whereas the latter changed toward a less pro-poor distribution. Regarding the private SP and public hospitals as well as hospitals (in total), the CI became less negative and became more positive for the private hospitals, which means that private SP visits and public hospitals admissions showed a less pro-poor distribution, while hospitals (in total) followed a more pro-rich distribution. The magnitude of CI for all outpatient services was small; however it was slightly more than the public and private hospital admissions.
Figure 1 presents the CC of the health services utilization. Based on this graph, the CC for all health services, except for private hospitals, was above the line of equality and this reveals that the utilization of these services were more prevalent among the poor people (a pro-poor distribution). CC for the private GP crossed the line of equality, which shows the minor association with SES. Finally, CC for private hospitals laid below the line of equality, which confirms the fact that utilization of this service was more concentrated on rich people (a pro-rich distribution).
| FP | GP | SP | Hospital | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Public | Private | Total | Public | Private | Total | Public | Private | Total | ||
| Deciles of the household score | ||||||||||
| 1 | 0.367 | 1.888 | 1.096 | 2.993 | 0.793 | 2.252 | 3.045 | 0.083 | 0.011 | 0.096 |
| 2 | 0.216 | 1.681 | 0.883 | 2.564 | 0.640 | 1.872 | 2.512 | 0.074 | 0.013 | 0.088 |
| 3 | 0.268 | 1.474 | 0.934 | 2.431 | 0.489 | 1.737 | 2.228 | 0.068 | 0.012 | 0.081 |
| 4 | 0.309 | 1.742 | 0.820 | 2.566 | 0.318 | 1.521 | 1.839 | 0.058 | 0.006 | 0.065 |
| 5 | 0.230 | 1.613 | 0.917 | 2.540 | 0.432 | 1.322 | 1.775 | 0.059 | 0.006 | 0.066 |
| 6 | 0.236 | 1.594 | 0.975 | 2.592 | 0.491 | 1.492 | 1.983 | 0.051 | 0.010 | 0.062 |
| 7 | 0.214 | 1.461 | 0.876 | 2.342 | 0.546 | 1.245 | 1.791 | 0.052 | 0.017 | 0.069 |
| 8 | 0.199 | 1.421 | 0.795 | 2.238 | 0.497 | 1.459 | 1.982 | 0.046 | 0.009 | 0.055 |
| 9 | 0.191 | 1.244 | 1.107 | 2.360 | 0.621 | 1.565 | 2.185 | 0.043 | 0.015 | 0.059 |
| 10 | 0.232 | 1.089 | 0.956 | 2.055 | 0.459 | 1.655 | 2.115 | 0.031 | 0.017 | 0.049 |
| Total | 0.246 | 1.521 | 0.936 | 2.468 | 0.529 | 1.612 | 2.145 | 0.056 | 0.012 | 0.069 |
| Standard concentration index | -0.088 | -0.077 | 0.001 | -0.047 | -0.042 | -0.060 | -0.055 | -0.145 | 0.077 | -0.108 |
| Standard error | 0.03 | 0.01 | 0.02 | 0.01 | 0.02 | 0.01 | 0.01 | 0.01 | 0.03 | 0.01 |
| Concentration index with inequality-aversion parameter = 3 | -0.148 | -0.109 | -0.016 | -0.072 | -0.092 | -0.121 | -0.113 | -0.221 | 0.077 | -0.172 |
| Concentration index with inequality-aversion parameter = 4 | -0.196 | -0.130 | -0.034 | -0.092 | -0.144 | -0.172 | -0.163 | -0.271 | 0.061 | -0.217 |
| Standard achievement index | 0.268 | 1.637 | 0.935 | 2.583 | 0.551 | 1.708 | 2.263 | 0.065 | 0.011 | 0.076 |
| Achievement index with inequality-aversion parameter = 3 | 0.282 | 1.686 | 0.951 | 2.647 | 0.577 | 1.807 | 2.387 | 0.069 | 0.011 | 0.081 |
| Achievement index with inequality-aversion parameter = 4 | 0.294 | 1.719 | 0.968 | 2.696 | 0.605 | 1.889 | 2.495 | 0.072 | 0.011 | 0.084 |
4. Discussion
No study has been done in Iran assessing both public and private health care utilization inequalities. Our findings showed that health care utilization in Iran had a pro-poor pattern for most services, however with some exceptions; SP visits in public and private hospital admission showed a pro-rich distribution.
FP visits in our study had a pro-poor pattern as expected. The Iranian government subsidizes FP program in the rural areas and cities with less than 20000 population and all primary health services are free. Our findings are consistent with of the results of a study in Markazi province in Iran (29). Other international studies in Australia, Korea, and Northern Sweden (16, 19, 20) show that in developed countries with universal health coverage, where the government subsidizes primary health services, all services represent a pro-poor pattern.
In our study, we separated the health care utilization by public and private sectors for GP and SP visits and hospital admission, because they are different in organization and financing arrangement. For example, they have different tariffs and are covered by insurance schemes differently. Many reforms have considered for services in one specific sector. For example, in HTP, inpatient services in the MOH hospitals are subsidized.
Our findings regarding GP visits in the public sector were similar to the results of the FP visits, since the government funds these public sectors Public tariff are introduced for them and they are in contracts with all insurance companies. Thus, they pay a very small amount as copayment at the time of using services. The second reason for this similarity is the growing pattern in using complementary insurance scheme beyond the basic insurance services. The GP visit in the private sectors in our study showed a pro-rich pattern, however it changed slightly toward a pro-poor distribution after standardization for the needs. These results are inconsistent with the findings of a cross-sectional study on urban residents in Shiraz, Iran in 2012 (25). They found a pro-poor pattern for all outpatient services, but following standardization for differences in needs, it changed toward a pro-rich distribution. Fars and Mazandaran provinces are the pilot areas for the installation of the urban FP program in Iran and this program funds all GPs in the private system for the visits and primary health care services or consultations.
| FP | GP | SP | Hospital | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Public | Private | Total | Public | Private | Total | Public | Private | Total | ||
| Deciles of the household score | ||||||||||
| 1 | 0.367 | 1.960 | 1.146 | 3.117 | 0.606 | 1.889 | 2.498 | 0.075 | 0.006 | 0.084 |
| 2 | 0.218 | 1.721 | 0.910 | 2.634 | 0.551 | 1.710 | 2.263 | 0.070 | 0.011 | 0.082 |
| 3 | 0.269 | 1.490 | 0.944 | 2.457 | 0.460 | 1.688 | 2.151 | 0.066 | 0.011 | 0.078 |
| 4 | 0.309 | 1.732 | 0.813 | 2.548 | 0.343 | 1.568 | 1.910 | 0.059 | 0.007 | 0.067 |
| 5 | 0.229 | 1.592 | 0.903 | 2.504 | 0.480 | 1.411 | 1.912 | 0.061 | 0.007 | 0.070 |
| 6 | 0.235 | 1.575 | 0.961 | 2.558 | 0.535 | 1.570 | 2.104 | 0.053 | 0.011 | 0.065 |
| 7 | 0.214 | 1.443 | 0.863 | 2.310 | 0.592 | 1.333 | 1.925 | 0.054 | 0.018 | 0.072 |
| 8 | 0.199 | 1.403 | 0.783 | 2.206 | 0.545 | 1.552 | 2.121 | 0.048 | 0.010 | 0.058 |
| 9 | 0.191 | 1.225 | 1.094 | 2.328 | 0.664 | 1.644 | 2.307 | 0.045 | 0.016 | 0.062 |
| 10 | 0.232 | 1.067 | 0.941 | 2.018 | 0.511 | 1.753 | 2.263 | 0.033 | 0.018 | 0.053 |
| Total | 0.246 | 1.521 | 0.936 | 2.468 | 0.529 | 1.612 | 2.145 | 0.056 | 0.012 | 0.069 |
| Standard concentration index | -0.089 | -0.086 | -0.010 | -0.057 | 0.025 | -0.018 | -0.007 | -0.118 | 0.146 | -0.074 |
| (95% CI) lower | -0.150 | -0.106 | -0.043 | -0.074 | -0.023 | -0.048 | -0.034 | -0/150 | 0/077 | -0/106 |
| (95% CI) upper | -0.032 | -0.064 | 0.022 | -0.039 | 0.075 | 0.002 | 0.011 | -0/106 | 0/197 | -0/064 |
| Concentration index with inequality-aversion parameter = 3 | -0.150 | -0.126 | -0.035 | -0.090 | 0.027 | -0.047 | -0.028 | -0.173 | 0.198 | -0.111 |
| Concentration index with inequality-aversion parameter = 4 | -0.198 | -0.153 | -0.060 | -0.116 | 0.016 | -0.072 | -0.049 | -0.207 | 0.223 | -0.135 |
| Standard achievement index | 0.268 | 1.652 | 0.945 | 2.608 | 0.515 | 1.640 | 2.160 | 0.063 | 0.010 | 0.074 |
| Achievement index with inequality-aversion parameter = 3 | 0.283 | 1.712 | 0.968 | 2.691 | 0.514 | 1.687 | 2.206 | 0.066 | 0.009 | 0.077 |
| Achievement index with inequality-aversion parameter = 4 | 0.295 | 1.753 | 0.992 | 2.755 | 0.520 | 1.728 | 2.251 | 0.068 | 0.009 | 0.078 |
In addition, we found that SP visit in the public sector had a pro-poor pattern, but after standardizing for needs, it changed toward a pro-rich distribution. The same result can be seen in many studies on overall SP visits (27), however no similar study was found in Iran. All studies have focused on overall outpatient visits or GP or SP visits without any differences between public and private sectors.
SP visits in the private sector showed controversial findings due to its pro-poor pattern. As shown in Table 5, it included the most frequent visits in Iran. In many developed countries with universal health coverage, SP visits also have a pro-rich model. For example, a study in Australia with a combined public-private health care system showed SP visits with a pro-rich pattern (20). Studies in other developing countries, such as Turkey, also found a similar result despite of the universal health coverage reform (21). These findings are similar to our results regarding SP visits in the public sector. Also, in a study assessing the health care reform effects in Chile introducing the national health plan in 2005, it was found that following CI reform, GP visits became positive, whereas SP visits became less positive (11). These results are not consistent with our findings regarding total GP and SP visits. In addition, another study in Chile showed that from 1992 to 2009, inequality of GP and SP visits was different, but GP visits often followed a pro-rich pattern and SP visits were close to equal (44).
These findings are associated with the effects of the new HTP reform due to the following reasons: First, public SP services are delivered mostly in medical university clinics, characterized by crowding and long waiting time. Second, the government has increased basic health insurance coverage for over 8 million people by changing MSIO to Iranian Health Insurance during 2014. Moreover, the results of UHSS in 2014 revealed that the main barriers in access to outpatient services were a direct payment, insurance coverage, and crowding (45). This situation can explain not only the high prevalence of SP visits in the private sector but also the pro-poor service, as a highly accessible service with a small copayment for newly insured people.
Although some studies conducted in Iran, like Kermanshah in 2017 (32) and Kerman in 2013 (46) found that outpatient care with a pro-poor pattern, a study in Yazd in 2014 reported the overall utilization with a highly pro-rich distribution (28). The results of the two first studies are consistent with our findings regarding total GP and SP visits.
In general, inpatient services in the public and private hospitals in Iran are characterized by a pro-poor and pro-rich pattern, respectively. This figure is similar to some other developing countries (47); however, it is in contrast to some developed countries with universal health coverage, such as Sweden (16), Denmark (18) and Korea (19), and Norway (13). Our results were in line with the findings of a study in Iran (27), in which the national data obtained from the health care utilization survey in 2008 was used and reported a pro-poor distribution for overall inpatient care. Our findings regarding the total hospital admission (with a pro-poor pattern) were also consistent with the results of a study conducted in Mongolia that fond a pro-poor pattern for the secondary care and public hospital visits (47).
Our results showed a high inequality between the public and private sectors in inpatient services, which may be related to different organizational arrangements in public and private sectors. Through an appropriate arrangement, we can guarantee equitable access and delivery that can be sustainable (48). Following the inauguration of the rural FP program, people can use inpatient services with small copayment through the referral system. In addition, people with rural insurance are eligible to pay a lower copayment for inpatient services in public hospitals following HTP. In contrast, no similar arrangement is found for the private sector hospitals. People must pay for a private tariff as much as they pay doctors. They also pay for all services that are not covered by insurance schemes. A study in Brazil showed that through 1998, 2003, and 2008, the overall doctor visits became less positive, however hospitalization became less negative (49). Another study conducted in rural areas of China from 2003 to 2008 reported that inpatient services changed toward less positive indices during the studied years (50). The findings of another study in two provinces in China, Gansu and Zhejiang, showed that outpatient services in both provinces followed a pro-rich pattern. The inpatient services in a less developed area, Gansu, showed a pro-rich distribution, however a pro-poor model was found in Zhejiang, as a well-developed province (14).
4.1. Strengths and Weaknesses
We used UHSS data as an accepted figure at the national level and useless at the subnational level, like provincial analysis. Subnational data can be often more helpful for local policy or decision making (51). Also, local studies can be more helpful or useful for the regional plans. In addition, UHSS contains no information about household consumption or income. According to the World Bank guide book (3), the best living standard measure is the consumption of the household. Thus, we used household assets as a factor as a standard living measure for ranking the households. This study did not address overall health care utilization; instead, we focused on health services utilization at delivery and sector levels. Overall measures showed the general aspects of an event, like overall outpatient services, which might be effective for inter-country comparisons.
Our findings can help health policymakers at the national level as a baseline to follow the effects of the new health sector reforms. It makes them aware of any changes in the level of service utilization in different sectors after each new policy or plan. In addition, the findings not only provide them with the pattern of health services utilization, but also they are representative of the direction and magnitude of inequalities in health service delivery.
Researchers are recommended to follow a more analytical approach in this issue, especially for measuring inequality in other services, such as pharmacy and para-clinical services utilization at the national and subnational levels as well as evaluating inequities in health care utilization. Analysis of the health inequity and decomposing it to its determinants is a potent and proper evidence for arranging the health care delivery system in reforms.
4.2. Conclusions
Different factors affect health care utilization in Iran health care system, among which some factors originate from differences in socioeconomic status. Organizational arrangement through health care delivery is also another effective factor. Equalities in the outpatient and inpatient health care utilization in public and private sectors were examined in this study. We showed that standardization of the health care utilization for differences in needs may change the pattern of inequality from a pro-poor to a pro-rich distribution and vice versa. We also showed the different effects of sectors on inequality. Our findings shed a light on the fact that most public services follow a pro-poor pattern. Private services, especially hospital inpatient services, indicate a pro-rich distribution. We found that Iranian health care delivery system is slightly equitable in the public sector and there is a need to sustain the present condition. The results of this study can be useful for preparing the baseline evidence for policymakers to track the changes using reforms and evaluate the progress toward universal health coverage.