1. Background
Knowledge management (KM) is a new managerial approach to manage intellectual property and information in the organization, supporting the organization in achieving a competitive advantage. Knowledge management is now a field of study, which has grown rapidly since 1980 (1). In the contemporary age of knowledge, organizations act in a more competitive, complex, and varied environment than they did in previous times (2). Knowledge is the main source of power in an organization, explaining why intellectual capital has replaced physical capital in leading organizations (3). Studies on organizational knowledge have led to the implementation of KM theories (4). Through KM processes, organizations can use their critical information and experiences in planning, decision-making, and problem-solving (5).
Two types of knowledge, i.e., tacit and explicit knowledge, can be found in each organization. Implicit knowledge is in the individual’s mind, whereas explicit knowledge can be traced and documented (6). Knowledge management often seeks to manage tacit knowledge and convert it into explicit knowledge. Different studies have been conducted on KM, aiming to facilitate the management of this type of knowledge (4-6).
Given rapid developments in the 21st century and widespread changes in organizations, KM seems to be a relatively serious challenge for the health system (7). Some studies claim that KM is still in its initial stages in the healthcare setting and its implementation in this sector has not been yet successful. Healthcare systems are faced with the shortage of medical personnel in many countries around the world and the elderly population is on the rise in different countries (8). Accordingly, physicians and other hospital staff need knowledge and lifelong learning to provide effective care for patients and improve the physical and mental health of patients upon admission, diagnosis, and treatment (4, 8, 9).
An organizational culture (OC) that supports knowledge is one of the most important factors in the proper understanding of knowledge among organizational members. An appropriate culture can integrate KM processes, such as creating, storing, sharing, and applying knowledge (10). From a constructivist point of view, OC is a continuous process of constructing/reconstructing identity inside and outside the organization (11). Previous studies showed that the collaboration of organization employees was highly important to implement KM (12).
A collaborative culture explains how organization employees cooperate actively in the workplace (13, 14). On the other hand, the learning culture points to the extent of efforts made by the organization to encourage its staff to learn and improve themselves for long-term success (10). According to the findings of much research (15, 16), a correlation exists between KM and the learning process. Also, organizational trust is an essential factor in the KM process (17). In fact, trust in an organizational context is associated with more communication among employees for the distribution of information (18).
Nevertheless, the culture and system of hospital organizations have not been yet implemented for successful KM (19). Also, there are uncertainties about the effective implementation of KM in organizations (20). Studies have shown the moderate status of KM and OC in teaching hospitals of Iran and the effects of OC on KM and its various dimensions have not been well defined. Despite the abundance of knowledge in teaching hospitals, it is not being used properly (2, 3).
2. Objectives
The current study aimed at evaluating the impact of different types of OC, such as learning, collaboration, and trust culture, on the implementation of KM from the perspective of employees in teaching hospitals of Qom, Iran.
3. Methods
This descriptive-analytical study was conducted in 2017. The study population consisted of all the staff working in medical, paraclinical, and administrative sectors of all the six governmental teaching hospitals, affiliated to the Qom University of Medical Sciences, Qom, Iran. The standard sample size was determined based on the literature recommendations for factor analysis studies. According to a previous study, the minimum sample size for factor analysis was 3 - 20 times the number of variables for each item of the questionnaire (21, 22).
The inclusion criteria consisted of all the staff with at least four years of work experience, and full-time cooperation with teaching hospitals. Being unwilling to participate in the study and incomplete questionnaires were the exclusion criteria. The data collection tool (questionnaire) for OC included 19 items. To increase precision, 570 participants were selected for the study. The proportional stratified sampling method was used for selecting eligible participants. Each hospital was considered a stratum. The share of each hospital was determined in a total of 570 questionnaires in proportion to the total number of employees in each hospital. Samples were selected by the simple randomized sampling method from a list prepared by the administration department and also based on the inclusion and exclusion criteria. The signed informed consent form was obtained from each eligible participant. The participants were also assured of the confidentiality of their information. Data were collected by self-reported questionnaires administered to the participants in person at the teaching hospitals. This study was done between December 2017 and March 2017.
The measurement instruments were created based on a literature review and using the modified version of the KM instrument adapted from the Gold index (23) with 24 items. Moreover, OC was measured using a modified version of OC assessment instruments by Hurly (1998), Islam et al., and Gold et al. (10, 14, 23) with 19 items. The items of the questionnaire were rated based on a five-point Likert scale, ranging from one (strongly disagree) to five (strongly agree).
To assess the validity and reliability of the instrument used in the current study, a pilot study of 30 subjects was performed. Cronbach’s alpha coefficients ranged from 0.856 to 0.967 for all the constructs. Likewise, composite reliability was measured in this study. Content validity was also evaluated, based on the feedback of academics in healthcare management. Moreover, two methods, namely convergent validity and discriminant validity, were used to validate the instrument. Finally, the validated and standardized questionnaire was utilized for data collection.
Data were analyzed in several stages. First, for descriptive statistics, SPSS version 16 was employed using mean and standard deviation and to determine the number of factors, exploratory factor analysis was used to assess the construct validity. The Principal Component Analysis (PCA) with varimax rotation was used to create different components of the scale from the correlated separate variables. Second, in LISREL 8.8, the measurement model was evaluated via confirmatory factor analysis. Finally, structural equation modeling was utilized to assess the fitness of the model.
4. Results
The demographic characteristics evaluated in this study included age, sex, education level, total years of job experience, and professional position in teaching hospitals. Based on the results, 66.7% of the participants were female and 33.3% were male. The majority of the participants (50.4%) were 31 - 40-years-old and 57.6% had a work experience of fewer than 10 years. The results are presented in Table 1.
| Variables | Frequency (%) |
|---|---|
| Gender | |
| Female | 380 (66.7) |
| Male | 190 (33.3) |
| Age (years) | |
| 20 - 30 | 162 (28.4) |
| 31 - 40 | 287 (50.4) |
| 41 - 50 | 110 (19.3) |
| > 50 | 11 (1.9) |
| Work experience (years) | |
| < 5 | 164 (28.8) |
| 5 - 10 | 164 (28.8) |
| 11 - 15 | 122 (21.4) |
| 16 - 20 | 69 (12.1) |
| 21 - 25 | 38 (6.7) |
| > 25 | 13 (2.2) |
| Education level | |
| Bachelor’s degree | 502 (88.1) |
| Master of science | 42 (7.4) |
| General practitioner | 6 (1) |
| Medical specialist | 20 (3.5) |
| Job description | |
| Specialist | 20 (3.5) |
| General practitioner | 7 (1.2) |
| Nurse | 357 (62.6) |
| Midwife | 46 (8) |
| Operation room expert | 13 (2.3) |
| Anesthesiologist | 10 (1.8) |
| Radiologist | 13 (2.3) |
| Laboratory expert | 10 (1.8) |
| Office affairs | 28 (4.9) |
| Financial affairs | 22 (3.9) |
| IT expert | 2 (0.4) |
| Medical record expert | 16 (2.8) |
| Hospital management | 1 (0.2) |
| Secretary | 13 (2.3) |
| Others | 12 (2.1) |
| History of attending conferences | |
| Yes | 404 (70.9) |
| No | 166 (29.1) |
| Total | 570 |
The KMO value was 0.962, indicating the sufficiency and suitability of the sample size for factor analysis. The Bartlett test was also found to be significant (P < 0.001). Furthermore, factors were extracted using principal component analysis and Varimax rotation. The results showed that the factor loadings of five items were below 0.5, which had to be deleted. The remaining 14 items were paired into three sets with eigenvalues of higher than one (Table 2). In total, these factors explained 86.21% of the variance of their respective variables.
| Constructs | Standardized Loading | t-Value | R2 | Cronbach’s Alpha | Composite Reliability | AVE | CVR | CVI |
|---|---|---|---|---|---|---|---|---|
| Learning culture | 0.974 | 0.976 | 0.886 | |||||
| Lea.cul1 | 0.96 | 30.96 | 0.92 | 1 | 0.97 | |||
| Lea.cul2 | 0.95 | 30.37 | 0.90 | 0.83 | 0.97 | |||
| Lea.cul3 | 0.93 | 29.23 | 0.86 | 1 | 0.97 | |||
| Lea.cul4 | 0.91 | 28.33 | 0.83 | 0.83 | 0.91 | |||
| Lea.cul6 | 0.96 | 30.86 | 0.92 | 0.83 | 0.97 | |||
| Collaboration culture | 0.944 | 0.997 | 0.817 | |||||
| Col.cul1 | 0.92 | 28.37 | 0.85 | 1 | 0.97 | |||
| Col.cul2 | 0.92 | 28.44 | 0.85 | 0.66 | 0.91 | |||
| Col.cul3 | 0.92 | 28.31 | 0.85 | 1 | 1 | |||
| Col.cul4 | 0.85 | 24.98 | 0.72 | 0.66 | 0.97 | |||
| Trust culture | 0.945 | 0.945 | 0.817 | |||||
| Tru.cul1 | 0.90 | 27.67 | 0.81 | 1 | 0.97 | |||
| Tru.cul2 | 0.89 | 26.79 | 0.79 | 1 | 0.97 | |||
| Tru.cul3 | 0.88 | 26.40 | 0.77 | 0.83 | 0.94 | |||
| Tru.cul4 | 0.86 | 25.58 | 0.74 | 0.83 | 0.94 | |||
| Tru.cul5 | 0.87 | 25.78 | 0.76 | 0.83 | 1 | |||
| Knowledge management | 0.724 | 0.476 | ||||||
| Knowledge creation | 0.71 | 14.50 | 0.50 | 0.972 | 0.80 | 0.96 | ||
| Knowledge storage | 0.71 | 14.59 | 0.50 | 0.971 | 0.83 | 0.98 | ||
| Knowledge sharing | 0.67 | 13.90 | 0.45 | 0.938 | 0.90 | 0.99 | ||
| Knowledge application | 0.67 | 13.95 | 0.45 | 0.902 | 0.89 | 0.99 |
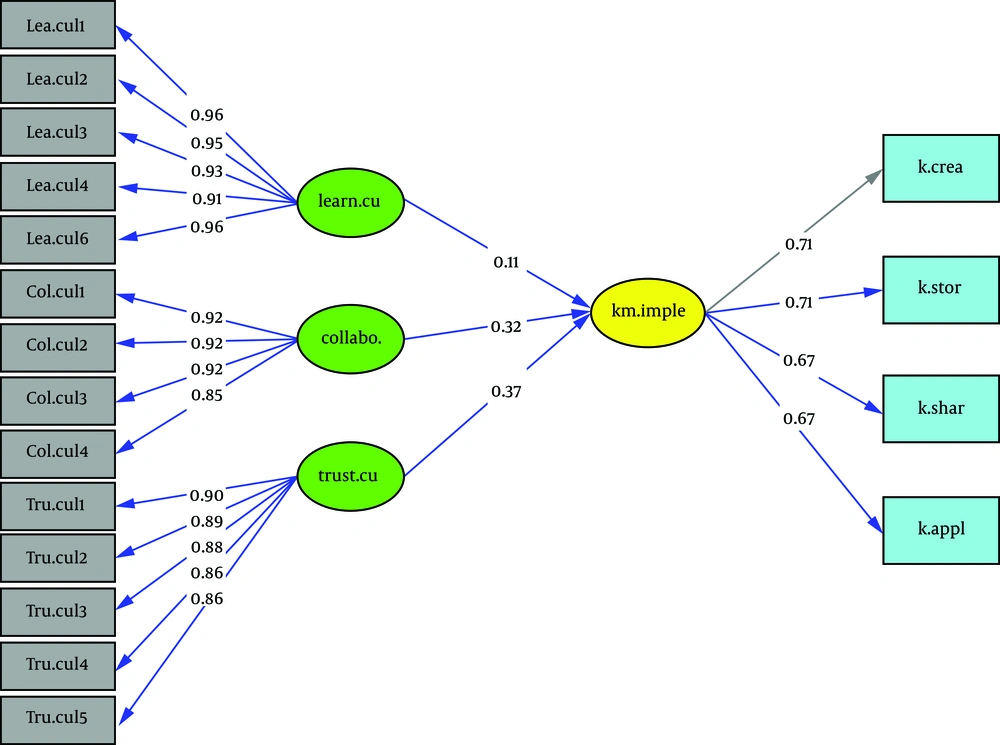
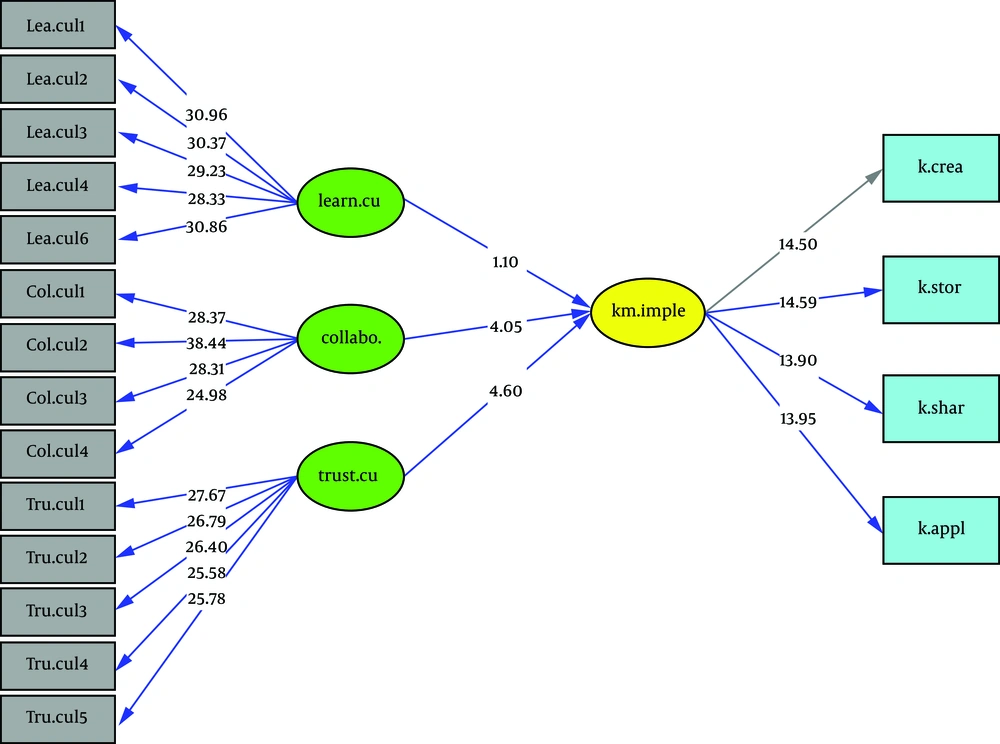
In addition, confirmatory factor analysis was used to verify the structures’ factor loadings. The principal component analysis showed different dimensions of OC including learning culture, collaboration culture, trust culture, and knowledge creation, storage, sharing, and application. The results of the measurement model are shown in Table 2. Also, we measured the standardized loadings, t value, and other metrics, as well as composite reliability and Average Variance Extracted (AVE). According to the results, the factor loadings of the items in the model ranged from 0.67 to 0.96, with Cronbach’s alpha coefficients for all three structures being 0.90 - 0.97. The CVR and CVI values varied from 0.66 to 1 and 0.91 to 1, respectively (Table 2).
Moreover, convergent validity and discriminant validity were used to validate the construct. According to the results of discriminant validity, the main diameter of the matrix was the square root of AVE, which was higher than the inter-construct correlations (Table 3). The maximum likelihood method was used to evaluate SEM. As shown in Table 4, the fit of the model was considered adequate based on the goodness-of-fit indices, as follows: RMSEA = 0.04, χ2/df = 2.12, SRMR = 0.018, Goodness-of-Fit index (GFI) = 0.95, Adjusted Goodness-of-Fit index (AGFI) = 0.93, Normed Fit index (NFI) = 0.99, Comparative Fit index (CFI) = 1.00, Incremental Fit index (IFI) = 1.00, and Relative Fit index (RFI) = 0.99. The test results and fit indices are illustrated in Figures 1 and 2 and Table 4. Trust culture and collaboration culture had the greatest effect and significance. On the other hand, learning culture was not significant and had the least impact on the implementation of KM in teaching hospitals.
aThe square root of AVE for each latent construct is shown in diagonals.
bCorrelation is significant at 0.01 (two-tailed).
| Independent Variables | Beta | t-Value | Effect |
|---|---|---|---|
| Learning culture | 0.11 | 1.10 | Direct |
| Collaboration culture | 0.32 | 4.05 | Direct |
| Trust culture | 0.37 | 4.60 | Direct |
| Variable | Value | Variable | Value |
| χ2/df | 2.12 | RMSEA | 0.04 |
| GFI | 0.95 | IFI | 1.00 |
| CFI | 1.00 | AGFI | 0.93 |
| NFI | 0.99 | SRMR | 0.018 |
| RFI | 0.99 |
Abbreviations: RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual; CFI, Comparative Fit index; GFI, Goodness of Fit index; AGFI, Adjusted Goodness of Fit index; NFI, Normed Fit index; IFI, Incremental Fit index; RFI, Relative Fit index
5. Discussion
The present study was performed to provide a clearer definition for the impact of OC and its various components (i.e., learning, collaboration, and trust culture) on the implementation of KM in the context of teaching hospitals. An integrated framework of culture was proposed and examined by exploratory and confirmatory factor analysis methods. We tried to choose the components of OC because it could play an important role in the KM process in educational environments. The model fit was approved by different indices.
The factor loadings of items in the proposed model ranged from 0.67 to 0.96. Based on a study by Hair et al., as cited in Liao et al. (24), factor loadings above 0.45 are significant. The Cronbach’s alpha coefficients for all the three structures were between 0.90 and 0.97, which surpassed the recommended threshold value (0.70) proposed by Segars et al., as cited in Liao et al. (24). The recommended AVE value of 0.5 or above for the variables is proposed by Fornel and Larcker, as cited in Taghavi et al. (25). In the current study, the AVE value exceeded 0.5, except for KM that had an AVE value very close to the standard. These findings indicate the good convergent validity of all dimensions. The estimated discriminant validity was higher than the inter-construct correlations. Based on the method described by Vogel et al. (26) and the criteria set by Claes and Larcker, as cited in Lin study (27), the discriminant validity of the study was confirmed. Moreover, the RMSEA value was under the recommended upper limit, showing the good fit of the model (28). The χ2/df value was also below the recommended maximum limit of five (24). Moreover, SRMR was under the recommended maximum limit of 0.08 (28). The GFI, AGFI, NFI, CFI, and IFI indices were higher than the recommended minimum limit of 0.90 (24, 28).
Overall, promoting the culture of learning, collaboration, and trust among the employees, especially in teaching hospitals, can facilitate the processes of creating, storing, sharing, and applying knowledge for treating patients and teaching students across various medical disciplines. This approach seems to be the most important advantage of the study.
The results of the present study revealed that learning, collaboration, and trust culture in teaching hospitals played important roles in establishing KM. The results also indicated that the component of trust culture, compared to the other two components, had a more significant positive impact on KM. Based on these results, fostering a climate of trust is one of the most important tasks of managers in teaching hospitals, which can encourage employees to share their information freely.
In this regard, the study by Lee (29) conducted in four South Korean hospitals indicated a significant positive relationship between trust culture and knowledge sharing and storage in some hospitals. In another study conducted at a South Korean teaching hospital, Lee and Hong (30) concluded that trust among hospital employees had a significant positive impact on KM. Moreover, according to the study by Lee et al. (31), the trust had a mediatory role in the creation and sharing of knowledge. Moreover, knowledge building had a significant positive relationship with trust, while trust among team members had a significant positive relationship with knowledge sharing (31). It seems that the existence of trust culture in the workplace can increase the sharing of knowledge and experience among employees and conversely, weak trust culture among employees will negatively affect knowledge sharing.
According to the findings, the component of collaboration culture had a significant positive impact on KM. Therefore, it is indispensable to take measures to encourage employees to engage in teamwork and improve their collaboration in medical centers, especially hospitals. Evidently, in teamwork, employees prefer collective benefits to individual interests, which is the ultimate goal of teamwork.
In a study by Mirbalouchzehi et al. (32) in hospitals of Iranshahr, there was a direct relationship between collaboration culture and KM. In addition, Pourtaheri and Aalaee (9) showed a significant direct relationship between collaboration culture and KM in Kerman hospitals. Moreover, in line with the results of other studies (9, 32), the existence of a collaboration culture, due to the existence of a great deal of teamwork in teaching hospitals, could lead to team success in the organization. Islam et al. (10) also found a positive relationship between collaboration culture and KM, although this relationship was not significant. The results of our study contradict this finding. It seems that in some organizations, employees believe in the idea that “knowledge is power”. Therefore, they avoid cooperation with others in the KM process because of the fear of losing power.
Based on the findings, learning culture had a positive impact on KM. Nevertheless, this effect was insignificant. Managers of educational hospitals need to encourage the employees to attend classes and workshops to improve their knowledge. In agreement with the results of the present study, Lee (29), in a study conducted in South Korean hospitals, found a direct relationship between learning culture and KM components although this relationship was insignificant. It seems that employees’ high job security and the weakness of annual appraisal in organizations can cause weakness in the learning culture and make the staff less willing to exert much effort to learn.
Concerning organizational learning, employees’ learning through knowledge sharing is a prerequisite for the long-term success of an organization, which has numerous potential advantages. On the other hand, the employees’ lack of interest in organizational learning can be indicative of their lack of motivation for knowledge-based activities and indifference towards organizational success. Therefore, hospital managers are expected to work hard to revive the learning culture among employees. This finding is not supported by previous studies. In this regard, according to Islam et al. (10), there was a significant positive relationship between learning culture and knowledge sharing.
The strength of this study is that it evaluated for the first time the impact of OC on KM implementation in Qom teaching hospitals using structural equation modeling. However, the current study had some limitations in this study. To begin with, this study covered the governmental hospitals, but did not include the private and semi-governmental hospitals. Second, the participants’ unfamiliarity with the concept of knowledge management was another limitation of this study; for this reason, some participants asked us to explain some of the items. Moreover, the effect of salary and benefits as covariates was not assessed in this study. Therefore, it is suggested that future studies compare the effect of OC on the implementation of KM in governmental and nongovernmental hospitals taking into account more confounding variables.
5.1. Conclusions
The present findings indicated that the staff of teaching hospitals had moderate total scores on KM, KM components, and OC (i.e., learning, collaboration, and trust). It can be concluded that teaching hospitals affiliated to Qom University of Medical Sciences have not addressed KM so far. This issue can be a serious challenge for teaching hospitals including weak learning from one another, low collaboration in teamwork practices, and low trust in one another. Therefore, the promotion of knowledge-based culture seems necessary for the establishment of KM in governmental hospitals. To overcome this challenge, it is suggested that knowledge activities such as workshops and staff encouragement programs to carry out teamwork be implemented for promoting the culture of learning, collaboration, and trust in different departments of the hospitals. In this way, hospital staff can become more familiar with the concepts of knowledge management and its benefits.