1. Background
Hepatitis A virus (HAV) infection is the most common form of acute viral hepatitis in the world. The incidence and prevalence of this infection are highly correlated with low socioeconomic and health indices (1). HAV contains a positive single-stranded RNA in the capsid without an envelope. This virus belongs to the genus Hepatovirus and the family Picornaviridae. HAV only contains one serotype, which is transmitted through direct contact with an infected person or by ingestion of contaminated water and food; the incubation period is about one month. HAV proliferates in liver cells, disrupts the liver function, and induces an immune response and an inflammatory process in the liver. This virus is excreted through the stool and can contaminate drinking water and food. Fecal shedding mostly occurs late in the incubation period, a few days before the emergence of clinical signs.
The majority of patients with HAV infection fully recover, and the fatality rate is reportedly low, without any comorbid chronic liver diseases. Also, these individuals usually acquire lifetime immunity (1). In developing countries, HAV infection occurs in childhood. The clinical signs of acute infections are usually milder, non-specific, or even asymptomatic and may remain undiagnosed due to the absence of jaundice. In children, viral shedding persists for a long time, while in adults, the virus causes acute infections with mild symptoms or may result in serious complications (1).
Around 1.5 million symptomatic HAV cases are reported each year worldwide (2). In recent decades, the prevalence of HAV infection has declined following the improvement of sanitation behaviors, especially water and food hygiene, besides the availability of HAV vaccines. On the other hand, the reduced infection rate has significantly increased the average age of infection. In other words, late exposure to the virus in adults may make this population significantly susceptible to the infection and increase the risk of HAV outbreak. Since the severity of HAV infection increases with age, it is appropriate to implement vaccination programs, especially among children, to reduce the risks in populations, including susceptible adults.
Detection of HAV seroprevalence is essential for evaluating the appropriateness of an infection control strategy in a population (1). According to the World Health Organization (WHO), HAV infection is endemic in Iran (3). Recent studies have shown that the seroprevalence of HAV is declining in some provinces of Iran and that today, the country can be considered as a low endemic area for HAV (4). Nonetheless, HAV vaccination has not been incorporated in Iran’s routine vaccination program.
According to previous studies in Iran, the prevalence of anti-HAV antibodies was 6% among children and young adults (age: 1 - 23 years) in Tehran (4) and 69% (age: 15 - 24 years) in Birjand, East of Iran (5). The weighted prevalence of anti-HAV antibodies varied across 16 provinces of Iran, ranging from 50.43% in Fars Province to 78.81% in Markazi Province (6). The anti-HAV seroprevalence was estimated at 93.2% in the general population of Hormozgan Province in the south of Iran (7). The prevalence of anti-HAV antibodies was also 91% among blood donors in Golestan Province in the Northeast of Iran (8). In addition, the prevalence of anti-HAV in Iranian blood donors was 70.7% in Tehran (2) and 49.0% in Qazvin Province (9).
Generally, the blood donor community can represent an accessible and practical sample of the general population for evaluating the seroepidemiology of HAV infection (2). Since routine blood donations are not monitored for HAV, there is no information on the seroprevalence of HAV in Iranian blood donors, especially in the West of Iran.
2. Objectives
This study aimed to determine the seroprevalence of HAV among blood donors in Sanandaj, Kurdistan Province, Iran.
3. Methods
3.1. Study Population and Specimens
In this cross-sectional study, 268 blood donors, presenting to the Kurdistan Division of Iranian Blood Transfusion Organization (IBTO) in Sanandaj, Iran, were randomly selected. The participants gave their consent to participate in the study. Specimens were collected after performing routine tests at the IBTO on the donors’ blood. The clotted blood was centrifuged at 3000 rpm for 15 minutes, and the sera were separated in new tubes and stored in a freezer at -20°C.
Moreover, data, including age, gender, marital status, education, occupation, and blood donor status, were collected in this study. The blood donors’ information was kept confidential. The present study was approved by the Kurdistan University of Medical Sciences (proposal and ethics code: IR.MUK.REC.1396/272).
3.2. Antibody Detection
Total anti-HAV antibodies (IgM and IgG) were measured using the competitive enzyme-linked immunosorbent assay (ELISA) kit, according to the manufacturer’s instructions (Diapro Diagnostic Bioprobes Srl, Italy). With the Food and Drug Administration (FDA) approval, the kit showed 100% sensitivity and more than 98% specificity.
3.3. Statistical Analysis
The results of ELISA assay and demographic data were entered in STATA version 14.0 and analyzed. P-values less than 0.05 were considered statistically significant.
4. Results
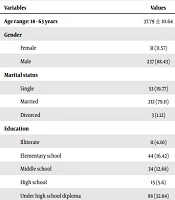
The mean age of 268 blood donors was 37.79 ± 10.64 years (range: 18 - 63 years). The demographic data of blood donors are presented in Table 1.
| Variables | Values |
|---|---|
| Age range: 18 - 63 years | 37.79 ± 10.64 |
| Gender | |
| Female | 31 (11.57) |
| Male | 237 (88.43) |
| Marital status | |
| Single | 53 (19.77) |
| Married | 212 (79.11) |
| Divorced | 3 (1.12) |
| Education | |
| Illiterate | 11 (4.10) |
| Elementary school | 44 (16.42) |
| Middle school | 34 (12.68) |
| High school | 15 (5.6) |
| Under high school diploma | 88 (32.84) |
| High school diploma | 20 (7.46) |
| Associate degree | 47 (17.54) |
| Bachelor or master of science degree | 9 (3.36) |
| Occupational status | |
| Unemployed | 31 (11.56) |
| Worker | 38 (14.18) |
| Farmer or rancher | 15 (5.6) |
| Employee or teacher | 58 (21.64) |
| Health worker | 3 (1.12) |
| Others | 123 (45.9) |
| Blood donation status | |
| First time | 52 (19.41) |
| Lapsed | 74 (27.61) |
| Regular | 142 (52.98) |
The Demographic Data of Blood Donors Presenting to the Iranian Blood Transfusion Organization (IBTO) in Sanandaj, Kurdistan Province, Irana
Out of 268 blood samples, 218 (81.34%) were positive, and 50 (18.66%) were negative for anti-HAV antibodies. The correlation between age and antibody seropositivity was significant (P = 0.014). In this study, 194 (81.86%) men and 24 (77.42%) women were positive for anti-HAV antibodies; however, the difference was not significant (P = 0.551). There was a significant relationship between marital status and anti-HAV antibody status, as the highest rate of anti-HAV positivity was found among married individuals (n = 179, 84.43%) (P = 0.027). The highest frequency of anti-HAV positivity (n = 10, 90.91%) was found in the illiterate group (n = 11), followed by the group with primary school education (n = 39, 88.64%) out of 44 donors. The lowest seropositivity was reported in subjects with a bachelor’s or Master of Science (MSc) degree, and six out of nine donors (66.67%) were positive for HAV antibody; however, no significant relationship was found (P = 0.586).
Analysis of the relationship between occupation and anti-HAV status showed that most positive cases were in the group of farmers and ranchers (14 out of 15; 93.33%), while the lowest rate of positivity was found in the unemployed (19 out of 31; 61.29%); the relationship between these two variables was statistically significant (P = 0.045). Among three groups of first-time, lapsed, and regular blood donors, the prevalence of anti-HAV antibodies was estimated at 82.69%, 82.43%, and 80.28%, respectively. However, there was no significant relationship between the donor status and HAV antibody results (P = 0.893) (Table 2).
| Variables | HAV Antibody | P-Value | |
|---|---|---|---|
| Positive (N = 218) | Negative (N = 50) | ||
| Age | 38.57 ± 10.84 | 34.4 ± 3.07 | 0.014 |
| Gender | 0.551 | ||
| Female | 24 (77.42) | 7 (22.58) | |
| Male | 194 (81.86) | 43 (18.14) | |
| Marital status | 0.027 | ||
| Single | 37 (69.81) | 16 (30.19) | |
| Married | 179 (84.43) | 33 (15.57) | |
| Divorced | 2 (66.67) | 1 (33.33) | |
| Education | 0.586 | ||
| Illiterate | 10 (90.91) | 1 (9.09) | |
| Elementary school | 39 (88.64) | 5 (11.36) | |
| Middle school | 29 (85.29) | 5 (14.71) | |
| High school | 11 (73.33) | 4 (26.67) | |
| Under high school diploma | 68 (77.27) | 20 (22.73) | |
| High school diploma | 16 (80.0) | 4 (20.0) | |
| Associate degree | 39 (82.98) | 8 (17.02) | |
| Bachelor’s or master of science (MSc) degree | 6 (66.67) | 3 (18.66) | |
| Occupational status | 0.045 | ||
| Unemployed | 19 (61.29) | 12 (38.71) | |
| Worker | 30 (78.95) | 8 (21.05) | |
| Farmer or rancher | 14 (93.33) | 1 (6.67) | |
| Employee or teacher | 48 (82.76) | 10 (17.24) | |
| Health worker | 2 (66.67) | 1 (33.33) | |
| Others | 105 (85.37) | 18 (14.63) | |
| Blood donation status | 0.893 | ||
| First time | 43 (82.69) | 9 (17.31) | |
| Lapsed | 61 (82.43) | 13 (17.57) | |
| Regular | 114 (80.28) | 28 (19.72) | |
The Status of Anti-HAV Antibodies with Regard to the Demographic Data of Blood Donors Presenting to the Iranian Blood Transfusion Organization (IBTO) in Sanandaj, Kurdistan, Irana
5. Discussion
In the present study, the prevalence of total anti-HAV antibodies (IgG and IgM) was 81.34% among blood donors; this indicates that HAV is prevalent in the study area. The antibody positivity was correlated with age and marital status. A high seroprevalence of HAV was also reported among men. However, there was no significant association between HAV seropositivity and gender. The high seroprevalence of anti-HAV antibodies was found in the illiterate group (n = 10, 90.91%). The majority of anti-HAV positive cases were farmers and ranchers (93.33%).
According to previous reports, the seroprevalence of HAV was 61.60% and 62.60% in the Middle East and Eastern Mediterranean region, respectively; also, the WHO reported an incidence rate of 65.74%. Cyprus reported the lowest prevalence rate of HAV (2.61%), while the United Arab Emirates (UAE) and Kuwait reported prevalence rates below 50%. The highest seroprevalence rates of HAV were reported in Afghanistan (99.01%), Iraq (96.35%), Somalia (96.00%), and Palestine (93.70%) (10).
In this regard, a study from Tehran, Iran, evaluated the seroprevalence of HAV among one- to 23-year-old people referred to hospitals of Tehran in 2017. The blood samples of 1120 people (516 men and 604 women) were tested for total anti-HAV antibodies by ELISA assay. The overall prevalence of anti-HAV antibodies was 6%, and a significant difference was found between genders (4). Moreover, the seroprevalence of HAV was evaluated among healthy people in Birjand, east of Iran. A total of 496 people were randomly selected, and total anti-HAV antibodies were determined by ELISA assay. The overall seroprevalence of HAV was 92.78%, while it was 69% among 15- to 24-year-old people. There was a significant correlation between anti-HAV antibodies and age, marriage, and education (5).
Furthermore, in a cross-sectional study conducted in different provinces of Iran (2009 - 2010), the serum samples of 10- to 18-year-old adolescents were examined for anti-HAV antibodies. A total of 2,494 samples were selected from 16 provinces by multistage random cluster sampling. The weighted seroprevalence of HAV varied across provinces, ranging from 50.43% in Fars to 78.81% in Markazi. Symptomatic HAV infections were seen among adolescents in all provinces of Iran (6). Also, in a cross-sectional study in 2013, a total of 501 serum samples were selected using multistage cluster sampling and evaluated for anti-HAV IgG antibodies in Shahrekord (Center of Chaharmahal and Bakhtiari Province) in southwest of Iran. The seroprevalence of HAV was estimated at 90.8% (11).
Moreover, the age-specific HAV seroprevalence was examined in a representative sample of Iranian adolescent students, aged 10 - 18 years. A total of 2494 serum samples were tested for anti-HAV antibodies by the enzyme immunoassay. The overall seroprevalence of HAV was 64%, which increased from 14.8% to 72.9% among 10- and 13-year-old students, respectively, without any significant increase in 18-year-old students. Also, no significant difference was observed in the seroprevalence of HAV between men and women or urban and rural residents. Overall, the seroprevalence of HAV was similar in four different socioeconomic regions of Iran (12).
Additionally, in a cross-sectional study, an anti-HAV antibody (IgG) was evaluated among people referred to healthcare centers for laboratory tests before marriage in Fars Province, south of Iran (2008 - 2009). Out of 1050 people, 88.2% were positive for anti-HAV antibodies. The seroprevalence of HAV increased with age (79.3% in individuals aged < 20 years, 91.3% in individuals aged 20 - 30 years, and 99% in individuals aged > 30 years). Also, the findings showed that 85.1% of people living in urban areas and 95.9% of people living in rural areas were positive for anti-HAV IgG. The seroprevalence of HAV was associated with the family members of the individuals (13).
Moreover, the population-based seroprevalence of HAV was studied in urban and rural areas of Sari, north of Iran, in 2007. A total of 1034 individuals, aged 1 - 25 years, were tested for anti-HAV lgG antibodies by enzyme immunoassays. The total seroprevalence of HAV was estimated at 38.9%. The lowest seroprevalence was 5.2% among younger groups (1 - 5 years) from urban areas, while the highest seroprevalence was 82.0% in older subjects (15 - 25 years) from rural areas. Overall, the seroprevalence increased with age among women and those living in rural areas (14).
In another study from Tehran, Iran, the plasma samples of 1065 children in the age range of six months to 20 years were tested for total anti-HAV antibodies. The total seroprevalence of HAV was 61.6% and increased with age (15). Also, the seroprevalence of HAV was measured in 1869 people aged 18 to 65 years in 2006. The samples were randomly selected from the general population of three provinces of Iran (Tehran, Golestan, and Hormozgan). The total seroprevalence of HAV was 86%, and the seroprevalence of HAV in Tehran, Golestan, and Hormozgan provinces was 85%, 99%, and 96%, respectively. No significant difference was observed between genders. Their results showed a lower seroprevalence in younger people in urban areas (70%). Overall, older age, marriage, and level of father’s education were associated with HAV seropositivity (16).
Moreover, another study was conducted among blood donors, referred to Tehran IBTO in 2014. The mean age of the donors was 38 years, and 95.9% of them were male. Out of 559 blood donors, 19.1% were first-time donors, 29.2% were lapsed donors, and 51.7% were regular donors. The seroprevalence of HAV was 70.7% and increased with age. There was no significant difference between genders in terms of the HAV seroprevalence. Donors with higher levels of education had a significantly lower HAV seroprevalence. However, the seroprevalence of HAV was significantly higher in regular and lapsed donors as compared to first-time donors (2).
Besides, the seroprevalence of HAV and the related risk factors were determined among blood donors in Qazvin, Iran, in 2008. Out of 351 blood donors, aged 17 to 60 years, 49.0% were regular blood donors, 94.0% were men, and 71.0% were married. The seroprevalence of HAV was estimated at 94.9% in this study. The seroprevalence was found to be higher among married and older donors, while it was low among those with high school or vocational secondary school education (9). The seroprevalence of HAV was detected among blood donors in Tehran, Iran. The sera of 407 blood donors, who were negative for anti-HIV, HBsAg, and anti-HCV, were tested for total anti-HAV antibodies (IgG and IgM), anti-HAV IgM, and HAV RNA. The level of antibodies was determined by ELISA assay, and HAV RNA was examined by nested RT-PCR. The prevalence of total anti-HAV antibodies was 86%. However, 1% of blood donors were positive for anti-HAV IgM; RNA was not found in any blood donors (17).
In addition, HAV antibodies and the frequency of acute HAV disease (HAV IgM and RNA) were determined among blood donors in Golestan Province in northeast of Iran for one year from 2016 to 2017. In sera that were negative for anti-HIV antibodies, HBsAg, and anti-HCV, the total anti-HAV antibodies (IgM and IgG) were determined by ELISA and nested RT-PCR assays for HAV RNA. Out of 400 sera, 91% were positive for anti-HAV, and all specimens were negative for anti-HAV IgM and HAV RNA (8).
The blood donor community can represent an easy, accessible, and practical sample of the general population for evaluating the seroepidemiology of HAV. Consistent with earlier studies that evaluated the seroprevalence of HAV in the general population and blood donors, the results of the present study are somewhat in line with the literature. The differences between the results might be due to variations in the population, age, sample size, and sensitivity and specificity of ELISA assay. In the present study, the seropositivity of anti-HAV antibodies was significantly correlated with the age, occupation, and marital status of blood donors. In the present study, we could not determine the seroprevalence of HAV among people aged < 18 years and > 63 years. Also, we could not separately detect anti-HAV IgM antibodies as indicators of recent infection.
5.1. Conclusions
A high percentage of blood donors in the present study had HAV antibodies and were immune to HAV infection. Generally, HAV was found to be endemic in the study area.