1. Background
Chronic hepatitis B (CHB) is a serious health issue affecting 300 million people worldwide (1). Chronic hepatitis B virus (HBV) infection increases the risk of liver cirrhosis, liver failure, and hepatocellular carcinoma, accounting for approximately one million deaths annually (2, 3). Therefore, CHB treatment aims to eradicate HBV or inhibit viral replication by administering appropriate antiviral agents and thereby improve the patient survival rate by preventing complications such as cirrhosis or hepatocellular carcinoma.
Lamivudine (LMV) is the first approved antiviral agent for chronic HBV infection and was shown to be efficacious in suppressing viral replication (4-6). Recently, lamivudine was reported to improve metabolic derangement in CHB patients (7). However, the long-term administration of LMV involves a high rate of drug resistance (up to 54% in three years, 70% or more in over five years) (8-11). The emergence of LMV-resistant mutations reduces the virological response to LMV and increases the risk of severe exacerbation of HBV infection and progression of liver cirrhosis (12-15).
Adefovir dipivoxil (ADV) is commonly used when a virological breakthrough occurs due to LMV-resistant HBV. The ADV administration in nucleos(t)ide analog (NA) treatment-naïve patients can be expected to show an antiviral effect and histological improvement similar to that obtained with LMV. Besides, ADV has also been shown to reduce serum HBV DNA levels of LMV-resistant mutant viruses, similar to that of wild-type viruses (16-18). However, when ADV is used in LMV-resistant patients, the incidence of ADV-resistant mutations is reportedly as high as 18% in one year and 25% in two years (19-21). To prevent ADV-resistant mutations, treatment with LMV and ADV combination in patients with the LMV-resistant mutant significantly reduces the incidence of ADV-resistant mutations to 1 - 2% over the same period (19-21). Therefore, a combination of LMV and ADV can be recommended to treat LMV-resistant CHB (19).
Tenofovir disoproxil fumarate (TDF) monotherapy was recently reported to be a highly effective treatment for LMV-resistant CHB (22), and clinical practice guidelines recommend it as first-line therapy in this population (23, 24). Unfortunately, TDF remains unavailable in several countries, including Asia-Pacific or South American countries. Therefore, ADV-based therapy should be considered for LMV-resistant CHB in areas of TDF unavailability.
Telbivudine (L-dT) is an L-nucleoside analog with an antiviral effect reportedly better than LMV and significantly lower incidence of resistance in treatment-naïve CHB patients (25). To date, there has been no well-designed clinical trial of combined treatment with L-dT and ADV in LMV-resistant CHB. Considering that L-dT was demonstrated to be superior to LMV in previous reports, L-dT and ADV combination therapy may have better antiviral efficacy than LMV and ADV combination therapy in patients with LMV-resistant CHB.
2. Objectives
This study was designed to investigate this hypothesis and suggest more appropriate treatment options for LMV-resistant CHB patients in areas with unavailable TDF.
3. Methods
3.1. Ethics Statement
The protocol was approved by the institutional review board at all clinical trial sites, and the study was conducted following the ethical principles of the Declaration of Helsinki (ClinicalTrials.gov Identifier: NCT01804387).
3.2. Study Design
This investigator-initiated, prospective, multicenter, randomized, comparative, open-label pilot study of the treatment of LMV-resistant CHB patients was designed in May 2011 and approved by the Ministry of Food and Drug Safety in June 2012 in Korea. Patients were recruited from 10 hospitals affiliated with eight universities. Patients with LMV-resistant CHB who met the inclusion and exclusion criteria were prospectively enrolled from January 2013 to May 2014. Written informed consent was obtained from all patients. Randomization tables were generated by the nQuery Advisor program (version 6.01; Statistical Solutions Ltd., Cork, Ireland) with a block size of 4. The randomization was performed by opening serially numbered sealed envelopes, which were stratified by the study site and distributed in advance. After enrolment, LMV + ADV or L-dT + ADV therapy was initiated according to a random sequence.
3.3. Inclusion and Exclusion Criteria
Inclusion criteria were as follow: (1) age 18 - 70 years; (2) hepatitis B e antigen (HBeAg)-positive or negative CHB diagnosed based on a positive serum hepatitis B surface antigen (HBsAg) test for more than six months; (3) LMV treatment for at least six months and maintenance therapy by the time of screening; (4) LMV-resistant mutations (rtM204V or rtM204I) identified by a restriction fragment mass polymorphism assay; (5) virological breakthrough defined by an increase of HBV DNA level by more than 10 times the lowest level; (6) HBV DNA ≥ 20,000 IU/mL in HBeAg-positive or ≥ 2,000 IU/mL in HBeAg-negative patients at the time of screening; and (7) voluntary agreement to participate in this study. Exclusion criteria were as follow: (1) presence of ADV-resistant mutation (rtA181T, rtA181V, or rtN236T); (2) laboratory findings of serum AFP > 100 ng/mL, serum phosphorus < 2.4 mg/dL, serum creatinine > 1.5 mg/dL, or creatinine clearance < 50 mL/min; (3) decompensated liver cirrhosis with ascites, hepatic encephalopathy, esophagogastric variceal bleeding, jaundice, or Child-Pugh-Turcotte score exceeding 7 points; (4) history of more than four weeks of administration of an NA other than LMV acting on HBV; (5) history of immunomodulatory drug administration such as interferon or thymosin-alpha1 within 24 weeks of screening; (6) previous history of liver transplantation; (7) positive antibody test for human immune deficiency virus, hepatitis C virus, or hepatitis D virus; (8) concomitant metabolic liver disease with elevated Alanine Aminotransferase (ALT) levels; (9) consumption of alcohol more than 140 g/week for men and 70 g/week for women; (10) taking medications affecting ALT or HBV DNA level (corticosteroid, immunosuppressant, or nonsteroidal anti-inflammatory drugs); (11) women of childbearing age unwilling to use proper contraceptive measures; (12) women currently pregnant or lactating; and (13) history of hepatocellular carcinoma or other untreated malignancies.
3.4. Data Collection
We measured serum HBV DNA level using real-time polymerase chain reaction, HBeAg and antibody against HBeAg (anti-HBe) level, HBsAg level, serum ALT level, serum creatinine level, and Creatine Phosphokinase (CPK) level at 13, 26, 39, and 52 weeks of treatment. The incidences of virological and biochemical breakthroughs and any drug side effects were assessed at every visit.
3.5. Definitions
The virological response was defined as a decrease in the HBV DNA level to less than 20 IU/mL based on a real-time polymerase chain reaction. The biochemical response was defined as a decrease in serum ALT level to ≤ 40 IU/L in either sex. Serologic responses included HBeAg loss or seroconversion of HBeAg to anti-HBe. Besides, HBsAg loss was defined as a positive to negative HBsAg status shift regardless of the appearance of hepatitis B surface antibodies. Definitions of genotypic resistance, virological breakthrough, and biochemical breakthrough followed the guidelines given by the American Association for the Study of Liver Diseases (24).
3.6. Statistical Analysis
Statistical analyses were performed using Statistical Package for the Social Sciences (version 18.0; IBM Inc, Armonk, NY, USA). Categorical variables, such as HBV DNA undetectability, ALT normalization, HBeAg seroconversion, and HBsAg loss rates, were analyzed using the chi-square test or Fisher’s exact test as appropriate. Continuous variables, such as mean HBV DNA and ALT levels, were compared between the groups using the Student’s t-test or the Mann-Whitney U test as appropriate. Serum HBV DNA levels were converted to a logarithmic scale before analysis. Data are expressed as mean ± standard deviation.
4. Results
4.1. Baseline Characteristics
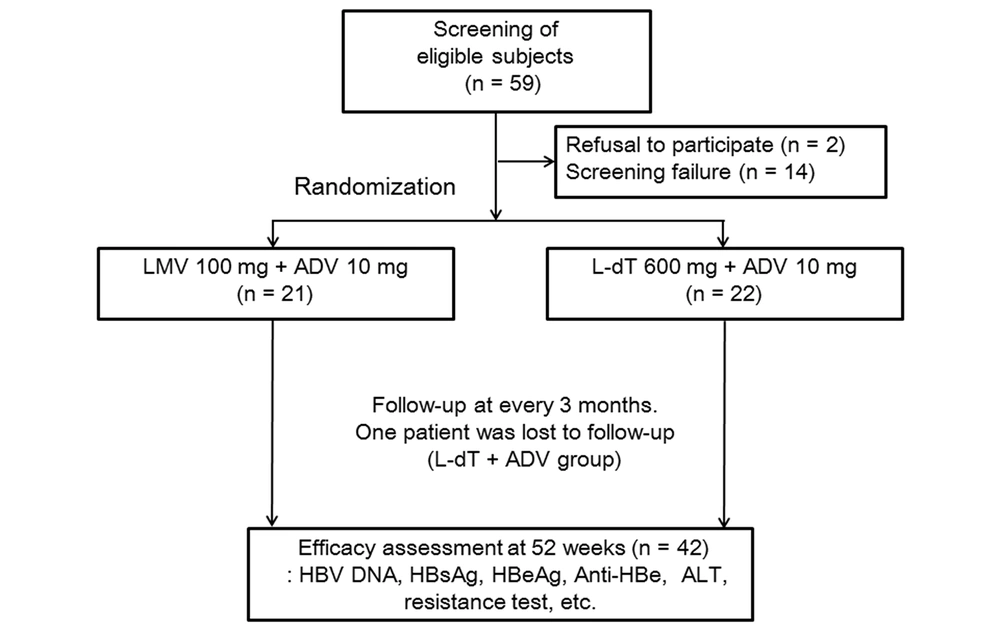
Forty-three patients who met the inclusion and exclusion criteria were included (Figrue 1). Twenty-one patients received LMV + ADV therapy, while 22 patients received L-dT + ADV therapy, with a mean patient age of 45.3 ± 8.7 and 49.3 ± 8.9 years, respectively. There were 13 (61.9%) males and eight (38.1%) females in the LMV + ADV group and 13 (59.1%) males and nine (40.1%) females in the L-dT + ADV group. The HBV DNA levels were 6.72 ± 1.48 log10 IU/mL and 6.53 ± 1.56 log10 IU/mL (P = 0.70) in the groups, respectively. Baseline lamivudine-resistant mutations were not significantly different between the groups (P = 0.37). besides, HBeAg-positive patients comprised 61.9% and 63.6% of the groups, respectively (P = 0.91). Serum ALT (86.5 ± 74.3 vs. 131.1 ± 214.0, p = 0.37) and creatinine (0.99 ± 0.22 mg/dL vs. 0.87 ± 0.22 mg/dL, P = 0.05) levels showed no significant intergroup differences (Table 1).
| Variables | Total (n = 43) | LMV + ADV (n = 21) | L-dT + ADV (n = 22) | P Value |
|---|---|---|---|---|
| Male | 26 (60.5) | 13 (61.9) | 13 (59.1) | 0.85 |
| Age (y) | 47.3 ± 9.4 | 45.3 ± 9.7 | 49.3 ± 8.9 | 0.60 |
| BMI (kg/m2) | 23.88 ± 2.50 | 23.70 ± 2.64 | 24.04 ± 2.42 | 0.67 |
| Glucose (FBS, mg/dL) | 100.88 ± 20.61 | 103.52 ± 18.54 | 98.36 ± 22.55 | 0.42 |
| Total cholesterol | 174.0 ± 34.4 | 176.44 ± 32.61 | 171.68 ± 36.67 | 0.68 |
| HBV DNA (log10 IU/mL) | 6.63 ± 1.52 | 6.72 ± 1.48 | 6.54 ± 1.56 | 0.70 |
| HBeAg positivity | 27/43 (62.8) | 13/21 (61.9) | 14/22 (63.6) | 0.91 |
| Platelet (× 103/µL) | 166.81 ± 49.78 | 180.81 ± 52.18 | 153.45 ± 44.49 | 0.07 |
| ALT (IU/L) | 109.3 ± 161.4 | 86.5 ± 74.3 | 131.1 ± 214.0 | 0.37 |
| CPK (mg/dL) | 96.0 ± 46.4 | 98.8 ± 56.50 | 93.05 ± 34.03 | 0.70 |
| Creatinine (mg/dL) | 0.93 ± 0.22 | 0.99 ± 0.20 | 0.87 ± 0.22 | 0.05 |
| Total bilirubin (mg/dL) | 0.84 ± 0.41 | 0.76 ± 0.29 | 0.92 ± 0.49 | 0.19 |
| Albumin (g/dL) | 4.37 ± 0.38 | 4.41 ± 0.37 | 4.33 ± 0.38 | 0.45 |
| INR | 1.05 ± 0.10 | 1.04 ± 0.08 | 1.07 ± 0.12 | 0.34 |
| Na (mmol/L) | 141.15 ± 2.24 | 140.76 ± 2.14 | 141.55 ± 2.33 | 0.27 |
| Phosphorus (mg/dL) | 3.37 ± 0.31 | 3.31 ± 0.32 | 3.42 ± 0.30 | 0.24 |
| Liver cirrhosis | 4/43 (9.3) | 1/21 (4.8) | 3/22 (13.6) | 0.61 |
| Baseline HBV mutation | 0.37 | |||
| rtM204I | 11 (25.6) | 7 (33.3) | 4 (18.2) | |
| rtL180M + rtM204V | 18 (41.9) | 9 (42.9) | 9 (40.9) | |
| rtL180M + rtM204I | 12 (27.9) | 5 (23.8) | 7 (31.8) | |
| rtL180M + rtM204I/V | 2 (4.7) | 0 (0) | 2 (9.1) |
Abbreviations: ADV, adefovir dipivoxil; ALT, alanine aminotransferase; BMI, body mass index; CPK, creatine phosphokinase; HBV, hepatitis B virus; HBeAg, hepatitis B e antigen; INR, international normalized ratio; L-dT, telbivudine; LMV, lamivudine; rtL180M, substitution of leucine to methionine on 180th amino acid of reverse transcriptase gene; rtM204I, substitution of methionine to isoleucine on 204th amino acid of reverse transcriptase gene; rtM204V, substitution of methionine to valine on 204th amino acid of reverse transcriptase gene.
a Values are expressed as mean ± SD or No. (%).
4.2. Virological and Biochemical Responses
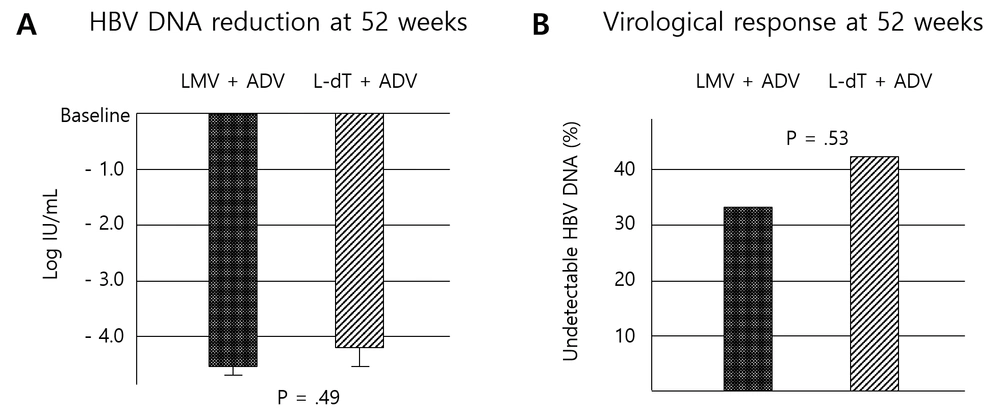
After 52 weeks of antiviral treatment, the LMV + ADV group showed a reduction in HBV DNA levels of -4.54 ± 1.23 log IU/mL, while the L-dT + ADV group showed a -4.24 ± 1.46 log IU/mL reduction. There was no significant difference between the two groups (p = 0.49) (Figure 2A). The virological response rate at 52 weeks showed no significant differences between the two groups (LMV + ADV group, 33.3%; L-dT + ADV group, 42.9%; P = 0.53) (Figure 2B). Further, the virological response rates at 13, 26, and 39 weeks of treatment did not differ significantly (Table 2). After 52 weeks of treatment, the mean HBV DNA levels were 2.18 ± 0.90 log IU/mL and 2.51 ± 1.45 log IU/mL in the LMV + ADV and L-dT + ADV groups, respectively (P = 0.384) (Table 3). None of the patients in either group showed HBeAg seroconversion or HBeAg or HBsAg loss (Table 2). Twenty (95.2%) patients showed ALT normalization in the LMV + ADV group versus 19 (90.5%) patients in the L-dT + ADV group. There was no significant intergroup difference (Table 2).
| Variables | LMV + ADV; No. (%) | L-dT + ADV; No. (%) | P Value |
|---|---|---|---|
| Virological response | |||
| 13 weeks | 4/21 (19.0) | 6/22 (27.3) | 0.52 |
| 26 weeks | 4/21 (19.0) | 5/21 (23.8) | 0.71 |
| 39 weeks | 8/21 (38.1) | 7/21 (33.3) | 0.75 |
| 52 weeks | 7/21 (33.3) | 9/21 (42.9) | 0.53 |
| HBeAg loss | |||
| 13 weeks | 0/12 | 0/12 | - |
| 26 weeks | 0/12 | 0/12 | - |
| 39 weeks | 0/12 (0.0) | 1/12 (8.3) a | > 0.99 |
| 52 weeks | 0/12 | 0/12 | - |
| HBsAg loss | |||
| 13 weeks | 0/21 | 0/22 | - |
| 26 weeks | 0/21 | 0/21 | - |
| 39 weeks | 0/21 | 0/21 | - |
| 52 weeks | 0/21 | 0/21 | - |
| Biochemical response | |||
| 13 weeks | 14/21 (66.7) | 15/22 (68.2) | 0.92 |
| 26 weeks | 18/21 (85.7) | 18/21 (85.7) | > 0.99 |
| 39 weeks | 19/21 (90.5) | 18/21 (85.7) | 0.96 |
| 52 weeks | 20/21 (95.2) | 19/21 (90.5) | 0.55 |
Abbreviations: ADV, adefovir dipivoxil; L-dT, telbivudine; LMV, lamivudine; No., number of patients with virological response or number of patients treated.
a HBeAg negative to positive seroreversion occurred at 52 weeks.
| Variables | LMV + ADV (Log IU/mL) | L-dT + ADV (Log IU/mL) | P Value |
|---|---|---|---|
| Baseline | 6.72 ± 1.48 | 6.54 ± 1.56 | 0.70 |
| 13 weeks | 3.27 ± 1.51 | 3.14 ± 1.91 | 0.82 |
| 26 weeks | 2.56 ± 1.05 | 2.74 ± 1.54 | 0.66 |
| 39 weeks | 2.27 ± 1.03 | 2.78 ± 1.72 | 0.25 |
| 52 weeks | 2.18 ± 0.90 | 2.51 ± 1.45 | 0.38 |
Abbreviations: ADV, adefovir dipivoxil; L-dT, telbivudine; LMV, lamivudine.
a Values are expressed as mean ± SD.
4.3. Antiviral Resistance and Safety
No patients showed virological breakthrough in the LMV + ADV group while two (9.5%) patients did in the L-DT + ADV group during 52 weeks, but the difference was insignificant (P = 0.488). No newly developed ADV-resistant mutation was observed in either group.
Finally, ADV combination therapy caused renal injury and hypophosphatemia. In addition, LMV and L-dT induced muscle injury and increased creatine phosphokinase. Changes in serum creatinine levels from baseline to week 52 did not differ between the groups. However, the mean changes in the serum CPK level from baseline to week 52 were significantly higher in the L-dT + ADV group than in the LMV + ADV group (1.00 ± 38.69 vs. 119.39 ± 207.90, p = 0.03) (Table 4).
| Variables | LMV + ADV | L-dT + ADV | P Value |
|---|---|---|---|
| Change in Cr (mg/dL) | 0.013 ± 0.100 | -0.006 ± 0.100 | 0.55 |
| Change in CPK (mg/dL) | 1.00 ± 38.69 | 119.39 ± 207.90 | 0.03 |
Abbreviations: ADV, adefovir dipivoxil; CPK, creatine phosphokinase; Cr, creatinine; L-dT, telbivudine; LMV, lamivudine.
a Values are expressed as mean ± SD.
5. Discussion
Recently, European and American clinical practice guidelines for managing CHB have recommended entecavir and tenofovir (TDF or tenofovir alafenamide) as first-line antiviral agents for treatment-naïve patients (23, 24). Tenofovir is recommended as the best option in the case of antiviral-resistant CHB, such as LMV resistance. As a result, the use of LMV, ADV, and L-dT for treatment-naïve CHB patients has decreased worldwide, and the usefulness of ADV for LMV-resistant CHB has also diminished. However, LMV + ADV remains an important treatment option for LMV-resistant CHB in countries where tenofovir is not approved or unavailable (e.g., Argentina, Malaysia, Indonesia, and Myanmar). Hence, clinical practice guidelines in the Asia-Pacific region on managing HBV infection reserved the combination of LMV and ADV as a second treatment option to a switch to TDF for LMV resistance (26). Although entecavir (ETV) monotherapy is not recommended as a rescue therapy since LMV-resistant mutations confer cross-resistance to ETV (27), switching ETV + ADV combination therapy is an effective treatment option in LMV-resistant HBV infection (28), although it is more expensive and thus, has not been recommended strongly.
Previous studies revealed that LMV + ADV showed a favorable effect in LMV-resistant chronic HBV infection (16-18). However, according to a recent study, LMV + ADV showed a low virological response rate of 38.4% at 12 months of treatment, especially in patients with high viral concentrations (19, 20). Nonetheless, research on new combination therapies to overcome this problem is lacking.
Few studies have examined the effect of L-dT and ADV combination treatment for LMV-resistant CHB. Lin et al. reported that L-dT + ADV showed a reasonable virological response rate compared to LMV + ADV treatment (29). However, the study was not randomized and had limited participants. On the other hand, Xu and Nie reported that L-dT and ADV combination therapy improved renal function of CHB patients (30). Hence, we expected a beneficial effect of L-dT + ADV on virological response and renal safety.
L-dT is generally a well-tolerated and safe drug for CHB treatment. Furthermore, it is effective for preventing HBV reactivation during immunosuppression or chemotherapy and mother-to-child transmission of hepatitis B, although the influence of prenatal L-dT exposure on neonates is under debate (31-34). The CPK level elevation (asymptomatic), myopathy, and neuropathy are the well-known side effects of L-dT (35). Many studies reported that the male sex and a low estimated glomerular filtration rate were significant risk factors for CPK level elevation during L-dT treatment (35, 36). However, few studies have been on the effects of L-dT and ADV combination therapy on CPK levels. In this study, the L-dT + ADV group showed a significant CPK level elevation compared to baseline, although most patients were asymptomatic. Further, none of the patients stopped taking their medication due to this side effect; however, CPK monitoring was necessary.
In the present study, the degree of HBV DNA level reduction and virological responses did not differ significantly between the groups. Creatinine levels tended to be lower in the L-dT + ADV group after 52 weeks of treatment, but there was no significant difference from the LMV + ADV group. Therefore, L-dT + ADV therapy showed no advantages concerning virological response or renal function and carried a risk of muscle-related problems.
This study is the first randomized controlled trial to evaluate the effect of L-dT and ADV combination therapy on LMV-resistant CHB. The major limitation of the present study would be the small number of patients, which limited the study's strength. Despite such a limitation due to the nature of a pilot study, the results showed that L-dT and ADV did not exhibit a better effect than LMV and ADV combination therapy and that side effects such as elevated CPK levels were observed. At the same time, there were no significant muscle-related symptoms that required discontinuation of therapy. However, both rescue regimens are not the current first-line treatment options in the current international guidelines. The recommended antiviral agents, which had excellent efficacy and high genetic barriers, such as ETV, TDF, and tenofovir alafenamide, were widely available in most countries. This is another major limitation of the present study. However, LMV, ADV, and L-dT are still being produced and prescribed to some CHB patients. Hence, both regimens can only be considered in limited situations of tenofovir unavailability.
In summary, the combination of L-dT and ADV showed no significant differences from the combination of LMV and ADV concerning HBV DNA reduction, virological response, viral breakthrough rate, and serologic and biochemical response rates at 52 weeks of LMV-resistant CHB treatment. Conversely, the level of muscle enzymes, such as CPK, increased more in the L-dT + ADV group.
In conclusion, the combination of L-dT and ADV for the treatment of LMV-resistant CHB showed no clinical benefit over the combination of LMV and ADV, and the additional monitoring of CPK levels was considered necessary during combination therapy with L-dT and ADV. Hence, combining LMV and ADV for LMV-resistant CHB patients in regions with unavailable tenofovir would be more appropriate.