1. Background
Non-alcoholic fatty liver disease (NAFLD) is the most frequent cause of chronic liver disease globally. In high-risk groups, the prevalence of this disease is estimated to vary from 25% to 40% worldwide, which is on the rise. According to a meta-analysis conducted by Moghaddasifar et al. (2016), Iran's estimated prevalence of NAFLD is 33.95% (1). Furthermore, NAFLD includes a wide variety of clinical diseases, ranging from non-alcoholic steatohepatitis (NASH) to simple hepatic steatosis. While NASH is defined by hepatocyte inflammation and degradation, which may develop into cirrhosis and hepatocellular cancer, simple steatosis is characterized by an excessive accumulation of triglycerides (TG) (above 5% of hepatocytes) in the liver (2). Also, NAFLD is most likely to develop in the context of abnormal metabolic processes in genetically predisposed individuals with metabolic disorders such as type 2 diabetes, obesity, dyslipidemia, metabolic syndrome, cardiovascular diseases, old age, and male gender. Also, dietary compositions such as high sucrose and fructose, which are associated with insulin resistance and, more recently, intestinal flora dysbiosis and inflammation, can increase the probability of contracting this disease (3, 4). Therefore, the cornerstone of NAFLD treatment is thought to be lifestyle changes, such as weight loss, exercise, and diet (5).
The Mediterranean lifestyle has been effective in reducing metabolic syndrome through anti-inflammatory actions, anti-oxidants, and blood lipid-lowering effects, as well as improving intestinal flora dysbiosis. Also, the diet is associated with low levels of aminotransferases and insulin resistance, reducing the severity of hepatic steatosis as a result of reducing the progression of NASH (3). Interestingly, several studies in recent years have revealed that dietary components or medicinal plants (with pharmacological capabilities) could be thought of as a substitute for traditional NAFLD management methods (6-10).
Portulaca oleracea, one of the most significant medicinal plants, is a good source of biologically active substances, including omega-3 fatty acids and -carotene (11), amino acids, -tocopherols, ascorbic acid, glutathione (12), and chemicals from flavonoids (13). Purslane's anti-inflammatory activity has been confirmed in several studies (14-18). Purslane has also been shown to reduce lung inflammation (19, 20). This plant also benefits from coumarins, polysaccharides, alkaloids, and anthraquinone glycosides (21). The side effects of this supplement occur in humans when more than 1 500 mg are taken per day, and these effects include hypoglycemia, hypotension, increased oxalate crystal deposits in the kidney, and decreased white blood cells (WBC) (22, 23).
Hepatoprotective (24-28) and anti-diabetic effects (29, 30) of P. oleracea extract have been reported in animal studies. In particular, in a study conducted by Guoyin et al. in 2018 on mice with liver damage, they observed that blood sugar and insulin levels, triglycerides (TG), total cholesterol (TC), aspartate aminotransferase (AST), alanine aminotransferase (ALT), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF- ɑ), and interleukin-1 beta (IL-1), were all significantly reduced by P. oleracea extract. Also, it improved the histopathological changes in the liver tissue (31, 32). Furthermore, in another study by Anusha et al. (2011), the extract of P. oleracea aerial parts significantly reduced AST, ALT, ALP (alkaline phosphatase), TC, and Total Bilirubin (TB) and improved steatosis, necrosis, and liver fibrosis in rats (25).
We plan to investigate the extract of P. oleracea aerial parts in this study due to the existing gap in the field of fatty liver treatment and the lack of research on the effects of this drug on liver steatosis or fibrosis in humans. Additionally, we observed beneficial effects from this plant on liver steatosis and fibrosis in animals.
2. Objectives
The main goal is to investigate a new potential therapy for NAFLD by clarifying the effect of P. oleracea supplementation on clinical and laboratory findings. The specific objectives included the following:
1. Comparison of liver steatosis and fibrosis status by two-dimensional elastography device in each group and between the intervention and control groups before and after the intervention
2. Comparison of serum concentrations of lipid profile, including TC, HDL-C (high-density lipoprotein cholesterol), LDL-C (low-density lipoprotein cholesterol), TG, FBS (fasting blood sugar), and insulin between two intervention and control groups before and after the intervention
3. Comparison of serum concentrations of the liver profile, including ALT, ALP, GGT (gamma-glutamyl transferase), and AST, between two intervention and control groups before and after the intervention
4. Comparison of anthropometric data, including height, weight, body mass category, and body composition (body fat and lean body mass), in each group and between the intervention and control groups before and after the intervention
5. Comparison of serum concentrations of malondialdehyde (MDA) and superoxide dismutase between two intervention and control groups before and after the intervention
6. Comparison of the calorie intake and proportion of the macronutrients (protein, carbs, and fat) in each group's diets over the course of 3 days, as well as between the intervention and control groups, before and after the intervention
7. Comparison of hs-CRP, IL-6, ESR (erythrocyte sedimentation rate), and glutathione serum concentrations between two intervention and control groups before and after the intervention
8. Comparison of IPAQ physical activity questionnaire scores in each group and between the intervention and control groups before and after the intervention
3. Methods
3.1. Study Design and Setting
This is a randomized, double-blinded trial with parallel groups. It is an interventional study with two arms (intervention and placebo groups). The Research Ethics Committee of Mashhad University of Medical Sciences confirmed the study on November 3, 2021 (ref approval no. IR.MUMS.REC.1400.223). Block randomization will be employed to allocate eligible participants to the control or intervention groups. The study protocol followed the Standard Protocol Items: Recommendations for Clinical Interventional Trials (SPIRIT) guidelines (33). Table 1 shows the diagram of the study protocol. The Standard Protocol Items: Recommendations for Clinical Interventional Trials (SPIRIT) checklist is provided as an additional file [see Additional file 1].
| Time Point | Study Period | |||||
|---|---|---|---|---|---|---|
| Enrolment | Allocation | Intervention | Close-out | |||
| 0 to 24 h | 0 | Day 1 | Day 30 | Day 60 | ||
| Enrolment | ||||||
| Eligibility screen | x | |||||
| Informed consent | x | |||||
| Medical history | x | |||||
| Allocation | x | |||||
| Interventions | ||||||
| P. oleracea | x | x | x | |||
| Placebo | x | x | x | |||
| Assessments | ||||||
| Demographic data | x | |||||
| Liver elastography | x | x | ||||
| Hepatic enzymes | x | x | ||||
| Lipid profile | x | x | ||||
| FBS, Insulin, HbA1C | x | x | ||||
| CBC-diff | x | x | ||||
| Inflammatory markers | x | x | ||||
| Oxidative stress markers | x | x | ||||
| Weight | x | x | x | |||
| Body composition | x | x | x | |||
| 3-day record | x | x | x | |||
| IPAQ questionnaire | x | x | x | |||
| Follow-up | ||||||
| Asking patients if they want to continue their diets | x | x | ||||
Abbreviations: SPIRIT, Standard Protocol Items: Recommendations for Interventional Trials Checklist; CBC-diff, complete blood count with differential count; FBS, fasting blood sugar; IPAQ, International Physical Activity Questionnaire; HbA1C, Hemoglobin A1C.
3.2. Sample Size
Sample size estimations will be based on Soleimani et al.'s study (34), which showed that the treatment group's mean changes in hepatic steatosis were roughly 65%, whereas it was stable or up to 27% in the control group. Based on the formula for comparing two proportions of a qualitative attribute from two independent statistical populations (α = 0.05, β = 0.2, the power of 80%), the sample size was established at 26 individuals in each group. However, 30 patients in each group will be considered, including a maximum of 15% dropouts.
3.3. Participants
3.3.1. Inclusion Criteria
All NAFLD patients who are directly admitted or transferred to the nutrition clinic must have a confirmed diagnosis of hepatic steatosis with or without fibrosis and fatty liver with F0 and F1 grades and be between the ages of 18 and 65 to enter the randomized clinical trial (RCT).
3.3.2. Exclusion Criteria
Patients are categorized as potentially eligible for the trial if they meet all preliminary eligibility requirements. Patients are also assessed to see if they meet any specific exclusion criteria that would prevent them from taking part in the trial. These criteria are meant to keep out people whose involvement would be hazardous or patients with serious illnesses whose effects on surgical outcomes might obscure the importance of dietary, clinical, and inflammatory factors. These are compiled in Table 2.
| Pregnancy and Lactation |
|---|
| Morbid obesity: BMI a ≥ 40 |
| Alcohol consumption: greater than 20 g for women or 30 g for men |
| Having cancer or a history of it, as well as any liver or renal failure |
| Suffering from autoimmune disorders and HIV b/AIDS c |
| Having a history of known food allergies to P. oleracea or any herbal supplementation |
| Receiving hepatotoxic medications, including sodium valproate |
| History of bariatric surgeries for weight loss |
a Body mass index
b Human immunodeficiency virus
c Acquired immunodeficiency syndrome
Following randomization, patients will only be dropped from the trial for the following reasons: (1) The patient's or physician's request or a major change in the patient's medical condition, (2) the presence of any exclusion criteria, and (3) sensitivity to supplements.
3.4. Data Collection at the Outset
At baseline, data will be collected on anthropometric indices, blood sampling, and serum separation for observation of CBC-diff, liver enzymes, lipid profile, inflammatory and oxidative stress factors, blood pressure, and completing relevant questionnaires, food records, and the IPAQ physical activity survey.
3.5. Randomizing and Blinding
After an effective screening and baseline evaluation, eligible patients are randomly assigned in a 1:1 ratio to one of the intervention groups using block randomization (block sizes of 4). Using Randomaize.com to select random numbers, the classification is based on age (18 to 40 and 40 to 60 years old) and gender (male or female). We will randomly assign eligible patients to the control or intervention groups during registration using SNOSE (sequentially numbered, opaque, sealed envelopes). In this way, the envelopes will be prepared and printed by one of the team members, and random numbers will be placed inside the envelope. Then, the purpose of the study is explained to the person who meets the stated conditions, and if the person wishes, they sign the informed consent form and take an envelope. Based on the contents of the envelope, the person is assigned to the intervention or control groups. Due to the consumption of a placebo that is comparable to the interventional treatment, neither the participant nor the participant's doctor will be aware of the allocated treatment, and neither will the analyst. The researcher who created the packages will reveal the codes A and B after studying the data. None of the participants, researchers, or analysts-aside from the pharmacist-will be aware of the medicine or placebo until the trial is complete. In this way, the groups are identified only with the codes A and B. The drugs are prepared in the same packaging and the same form and are packaged by a person in the pharmaceutical company who is outside the research team in the form of packages coded A and B. The password for the codes is kept securely in the system so that the codes can be opened after collecting the data. This approach will be implemented to ensure proper randomization, blinding, and reduction of potential biases in the study.
3.6. Procedures
3.6.1. Dose Selection
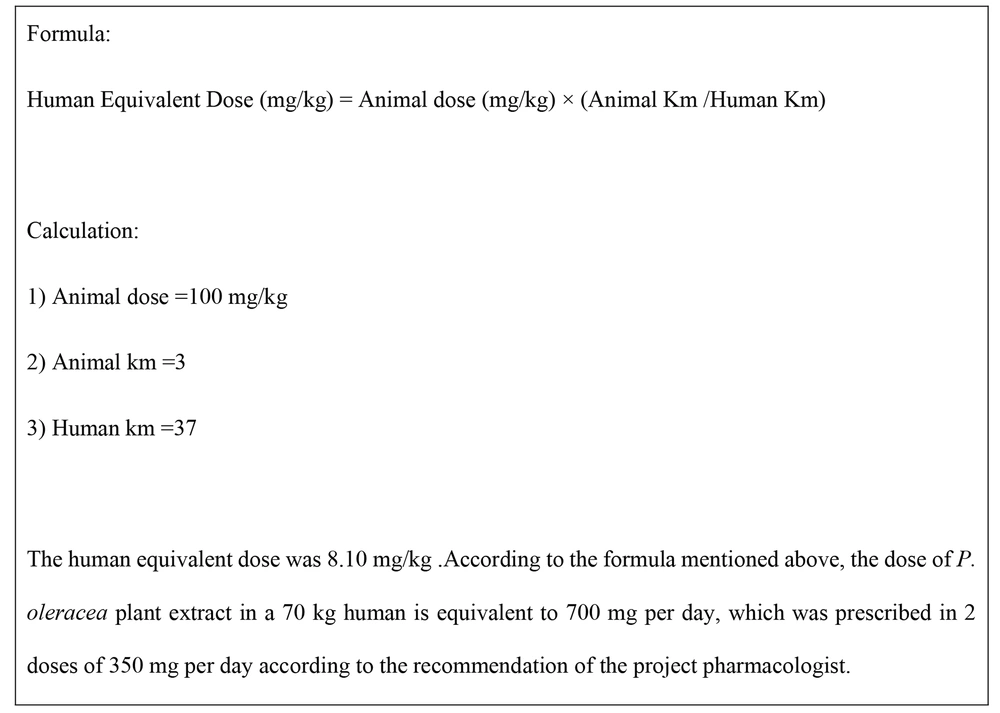
In this study, the supplemental dose of P. oleracea extract is prepared according to the study of Guoyin et al., who observed the effectiveness of the P. oleracea supplement at a dose of 100 mg/kg on the liver condition in rats under the supervision of the study pharmacologist. According to the following formula, 700 mg was determined to convert the optimum dose from animal to human (32). This formula calculates the safe human dose by considering the body ratios of the human and the studied animals (Figure 1). Also, no side effects have been reported with this dose in the studies. Also, to be sure, this project will be trialed on five people at first, and biochemical data, digestive evaluation questionnaires, and other items will be checked, and the project will proceed if no challenges or problems are reported.
3.6.2. Preparation of capsules
About 350 kg of P. oleracea plants are collected from Mashhad. After washing, they will be dried at a low temperature in the dryer. The dried powder will then be used to make a 70% hydroalcoholic extract. Also, 70% edible ethanol (without preservatives and bitters) will be used to prepare the extract. After mixing the powder with 70% ethanol, the resulting suspension will be placed on a shaker at a temperature of 37°C for 72 - 96 hours to separate the active ingredients from the P. oleracea aerial parts powder. Finally, after 96 hours, the dark liquid obtained will be concentrated with a rotary device and dried with a freeze-dryer. After obtaining the dry powder of the extract, it will be weighed, and the extract efficiency will be measured. In order to standardize, total phenol will be measured by the Folin Miran method. The LC-MS/MS method will also be used to determine the components of the extracts. To make capsules (the calculated dose per day is 700 mg), two capsules of 500 mg will be used, 350 mg of which will be the dried extract and 150 mg will be Avicel. Therefore, the final mixture will contain 70% extract and 30% Avicel, and finally, P. oleracea capsules will be prepared using a capsule filling machine. In the capsules of the placebo group, which should be similar in shape, color, and size to those of the intervention group, Avicel is used as a filler along with a small amount of green confectionery color to make the powder inside the capsule the same color as that in the intervention group. Placebo and control capsules have a matte coating, so the contents are not visible.
3.6.3. Intervention
We will enroll 60 patients admitted or transferred to the nutrition clinic in Mashhad, Iran. Each participant must provide the clinician with their informed consent before beginning any activity. Following randomization, the intervention group will receive 60 P. oleracea capsules (350 mg) in the first 30-day period and another 60 capsules at the beginning of the second 30-day period. Participants are asked to take the capsules twice daily, with breakfast and dinner. The control group will receive capsules similar in color and number with the same prescription.
In this study, all participants will be placed on a hypocaloric diet, following the recommendations of the American Dietetic Association (ADA), with the aim of achieving a weight loss of approximately 0.5 to 1 kilograms per week. Accordingly, 500 to 1000 kilocalories (depending on the calculated daily energy requirement based on the Harris-Benedict formula adjusted for body weight) will be reduced from their daily energy intake. This diet consists of 55% carbohydrates, 15% protein, and 30% fat. Additionally, all participants will be advised to engage in physical activity in accordance with the EASL-EASD-EASO guidelines, which recommend a minimum of 3 sessions per week, each lasting 60 minutes, of moderate-intensity aerobic physical activity, alongside the Mediterranean dietary recommendations.
Lifestyle modification, including dietary changes and physical activity with the goal of gradual weight loss, serves as the cornerstone of managing and treating NAFLD. To maintain ethical considerations and reduce potential confounding effects, both intervention and control groups will be provided with these lifestyle modifications.
3.6.4. Follow-up
The follow-up of the patients in this research will be done by telephone weekly by the researcher to check the patient's condition. Participants will be scheduled for their follow-up visits during the last week of the 30-day period.
3.7. Safety Considerations
A trained medical professional involved in the study will promptly discuss any medical issues or anomalies discovered during the intervention and follow-up procedures with the subject. Participants may receive treatment, be sent to a specialist, or be instructed to make an appointment with their primary practitioner as needed. However, participants will receive routine biochemical and clinical assessments, and liver function tests, including ALT (alanine aminotransferase) and AST (aspartate aminotransferase) serum levels, will be examined. Supplementation will be stopped right once if any potential issues arise from the intervention or if the doctor decides it should be stopped altogether.
3.8. Anthropometric Assessments
For anthropometric assessments, a digital floor scale, the Seca model 813 (Germany), with an accuracy of 0.1 kilograms, will be used to measure weight (without shoes and with minimal clothing). Height will be measured using a wall-mounted stadiometer, the Seca model 206 (Germany), with an accuracy of 0.1 centimeters. Waist circumference (the distance between the lowest rib and the top of the iliac crest, with light clothing) will be measured using a flexible, non-compressing tape measure.
Body composition assessments, including body fat percentage, fat mass, and fat-free mass, will be conducted using the bioelectrical impedance analysis (BIA) technique. This will be performed with the Tanita body composition analyzer, model BC-418 (Tanita Corporation), in the nutrition clinic. Bioelectrical impedance analysis is a method that estimates body composition by considering the electrical conductivity of various body tissues. The BIA, compared to other body composition assessment methods such as skinfold thickness, height, and weight, is known for its higher precision and accuracy.
Following the protocol of this method, the participants will be instructed to fast for 2 to 3 hours before measurements, refrain from intense physical activity or exercise for 4 to 6 hours earlier, ensure an empty bladder, and maintain hydration of the body to minimize measurement errors (2).
It will be advisable for participants to remove metallic objects and accessories, such as rings and watches when using the device. The individual stands still on the device for approximately 60 seconds, and upon completion, the analysis result (body composition data) is displayed on the monitor and can be printed.
The Body Mass Index (BMI), defined as weight in kilograms divided by the square of height in meters, will be recorded based on the information obtained from the body composition data. All these measurements will be carried out by a single person (researcher) until the end of the study.
3.9. Assessment of Liver Stiffness
Imaging of liver tissue and assessment of liver stiffness will be conducted using two-dimensional elastography, utilizing the Aixplorer ultrasound system (Aixplorer; SuperSonic Imagine S.A., Aix-en-Provence, France). The hepatic evaluation of participants will be performed by a radiologist employing a convex, wide probe (SXC6-1), following the manufacturer's guidelines for the device. During patient measurement, they will be required to lie in a supine position with their right arm maximally extended, and the examination will be conducted after a fasting period of 3 hours.
As per the guidelines outlined in this method, only reliable measurements are considered, requiring a minimum of 10 consecutive, valid measurements of liver stiffness (LSMS) for each individual, along with a ratio of interquartile range to the median (IQRLSM) less than 0.30. The results obtained from liver tissue elastography will be reported as the median LSMS in kilopascals.
This device, through quantification of liver echogenicity, is capable of assessing the severity of liver steatosis using the hepatorenal sonographic index (HSI). According to the cutoff points determined by Webb et al. (35), liver steatosis is classified as follows:
Mild steatosis (grade 1): 1.4 ≤ HSI < 1.86
Moderate steatosis (grade 2): 1.86 ≤ HSI < 2.23
Severe steatosis (grade 3): HSI ≥ 2.23
Similarly, the determined cutoff points using liver elasticity values to determine the degree of liver fibrosis are as follows (35):
• Stage 0 fibrosis (F0): Liver elasticity < 6 kilopascals
• Stage 1 fibrosis (F1): 6 ≤ Liver elasticity < 7 kilopascals
• Stage 2 fibrosis (F2): 7 ≤ Liver elasticity < 8 kilopascals
• Stage 2-3 fibrosis (F2-F3): 8 ≤ Liver elasticity < 8.8 kilopascals
• Stage 3 fibrosis (F3): 8.8 ≤ Liver elasticity < 10.2 kilopascals
• Stage 3 - 4 fibrosis (F3-F4): 10 ≤ Liver elasticity < 11.6 kilopascals
• Stage 4 fibrosis (F4): Liver elasticity ≥ 11.6 kilopascals
3.10. Measurement of Blood Pressure
The measurement of blood pressure will be conducted accurately using a mercury sphygmomanometer (ALPK2) with a standard cuff size of 12×25 centimeters, which will be precisely calibrated and standardized, along with a medical stethoscope. Patients will be required to sit comfortably on a chair for 5 - 10 minutes and abstain from smoking, consuming tea or coffee, or engaging in physical activity for at least 30 minutes prior to the measurement. Blood pressure assessments will be performed by the research project student during each visit, with two readings taken and their average calculated and recorded.
Blood pressure classification will follow the criteria of JNC-VII. Specifically, normal blood pressure is defined as systolic blood pressure less than 120 mmHg and diastolic blood pressure less than 80 mmHg. Prehypertension involves systolic blood pressure between 120 and 139 mmHg or diastolic blood pressure between 80 and 89 mmHg. Hypertension is categorized as systolic blood pressure equal to or exceeding 140 mmHg or diastolic blood pressure equal to or exceeding 90 mmHg.
3.11. Dietary Intake Assessment
In this study, a dietary intake assessment will be performed using a three-day food record questionnaire. These records will be preferably completed over two working days and one non-working day, selected at random.
During the initial visit, patients will complete the aforementioned questionnaire to precisely evaluate their dietary habits, including both macronutrient and micronutrient intake. After providing the necessary instructions, patients will be requested to complete the three-day food record questionnaire at both the beginning and the end of the study.
To assess dietary intake, the quantities recorded by patients were converted into grams per day using household measurement guides. Subsequently, the Nutritionist IV software (N-Squared Computing, Salem, OR, USA) will be employed to determine calorie intake as well as macronutrient and micronutrient values from the recorded dietary data.
3.12. Physical Activity Assessment
To assess the daily physical activity levels of the participants, the International Physical Activity Questionnaire (IPAQ) will be utilized. This questionnaire will be completed by participants both at the beginning and end of the study. The reliability of this questionnaire has been reported to be between 78% and 84% (36, 37). The IPAQ is designed for individuals aged 18 to 65 and includes questions regarding the number of hours of physical activity at various intensities in the past seven days (37, 38).
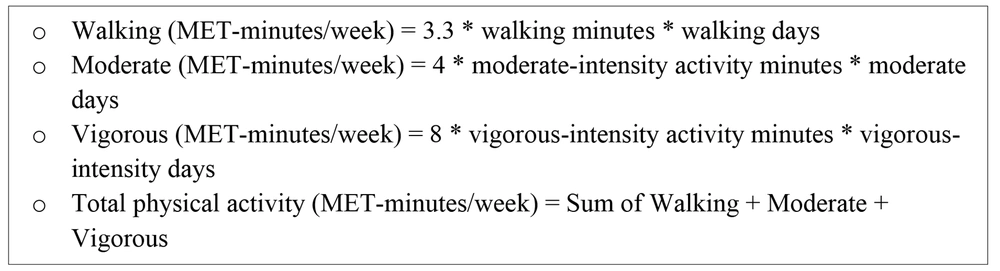
To analyze participants' responses to this questionnaire and categorize them into three groups: low physical activity, moderate physical activity, and high physical activity, MET (metabolic equivalent of task) values will be calculated for each activity category using specific formulas (Figure 2). The total METs will be considered as the individual's "total physical activity." Individuals with total physical activity less than 600 MET-minutes/week will be classified as having low physical activity, those with activity between 600 and 3 000 MET-minutes/week will be classified as having moderate physical activity, and those with activity exceeding 3 000 MET-minutes/week will be classified as having high physical activity (39).
3.13. Data Collection and Analysis
Data will be gathered three times in particular: at the baseline, on day 30 of the intervention, and on day 60 of the follow-up visit. A questionnaire is used to collect demographic data at the beginning. Additionally, blood pressure (via a Riester Nova.1032), body mass index and body composition (via a bioimpedance device, "TANITA"), height (via a standard meter), weight (via a portable scale, "Balas"), gastrointestinal complications, and blood pressure will be measured at baseline, on the 30th day, and at the end of the intervention. Transient elastography will be carried out at the beginning and end of the trial to assess the liver's state. At baseline, on the 30th day, and at the end of the intervention, the participants will also fill out a 3-day food diary and the International Physical Activity Questionnaire (IPAQ). In order to lessen bias, the responder will be requested to clarify any inconsistent answers. Also, 10 ml of venous blood will be taken at the start and finish of the research from each patient in order to assess biochemical factors like CBC-diff (by using Sysmex KX21), lipid profiles, FBS, serum insulin, hepatic enzymes like ALP, AST, ALT, GGT, total and direct bilirubin (via Auto analyzers), as well as inflammatory and oxidative stress markers like hs-CRP, ESR, GPX, and MDA (by using colorimetrya). The serum samples will be isolated, and ELISA kits will be used to measure the markers.
3.14. Data Management
At each time point, the study team will complete specifically the designed forms that will be scanned, reviewed, and committed to a local database within 48 hours of completion. Data cleansing is ongoing throughout this process. The completed forms will be kept in a locked cabinet as the study team's source documentation. The forms will be identifiable by a unique participant ID number and will not contain any information that might be used to identify a specific patient. A Microsoft Access database is used to store the majority of the data (Microsoft, Redmond, WA, USA). Daily queries will be generated based on database data, including date, range, and logic checks.
3.15. Statistical Methods
The statistical analysis will be carried out using SPSS 26 (SPSS Institute, Chicago, IL, USA). Data normality will be evaluated using graphical techniques, numerical properties, and the Shapiro-Wilk test. For the comparison of categorical variables, the chi-square will be employed. Between-group comparisons and within-group analyses of quantitative variables assumed to follow a normal distribution were conducted using the independent two-sample t-test and paired t-test, respectively. For variables not conforming to a normal distribution, the Mann-Whitney U test and Wilcoxon signed-rank test were applied for between-group and within-group comparisons, respectively. For each variable, baseline measurements will be taken into account using an analysis of covariance (ANCOVA). The R software will be used to run a nonparametric ANCOVA. Data will be reported as numbers (%) and means ± SD. Also, P < 0.05 will be considered statistically significant.
4. Discussion
Our findings provide evidence that the most effective underlying causes of fatty liver are insulin resistance, inflammation, and oxidative stress (40). Pro-inflammatory mediators such as TNF- α, IL-6, and IL-1 β are increased during NAFLD progress through the inducement of the NF-κB pathway (4).
As known, P. oleracea has anti-oxidant effects due to compounds such as omega-3, alpha-tocopherol, ascorbic acid, beta-carotene, glutathione, flavonoid, terpenoid, and alkaloid compounds. Purslane flavonoids exert lipid-lowering effects by reducing fatty acid synthase (FAS) mRNA and protein levels and inhibiting pancreatic lipase. Omega-3 fatty acids can improve hyperlipidemia by inhibiting FAS and acyltransferase (41). On the other hand, purslane contains high levels of phenolic alkaloids, which inhibit cholesterol synthesis by increasing unsaturated fatty acids (42). It also has anti-inflammatory properties due to its effects on the Nf-kB and PI3K (Phosphoinositide 3-kinases) pathways, which result in lower levels of IL-6, IL-1 β, TNF- α, and prostaglandin E2 (43-45). It possesses anti-steatosis and anti-liver fibrosis benefits because of its anti-inflammatory and anti-oxidant qualities, as well as its effects on lowering the expression of pro-fibrogenic cytokines and collagenolytic activity (43, 46). Due to the high quantity of polyunsaturated fatty acids and its effect on the gene expression of peroxisome proliferator-activated receptor gamma and LDL receptor, respectively, P. oleracea consumption may also affect the glucose and lipid profile parameters of individuals with NAFLD (47). In a study conducted by Sousou et al. on rats with liver fibrosis, supplementing with purslane aerial part extract caused a significant decrease in AST, ALT, ALP, GGT, TB, MDA, and TNF and a substantial increase in SOD (super oxide dismutase), CAT, GPx, and GSH (48). The current RCT seeks to determine the effects of a hydro-ethanolic extract of P. oleracea aerial parts on clinical and paraclinical findings in patients with NAFLD admitted to Imam Reza Hospital's Gastroenterology Clinic. Despite the promising results in animal studies, to our knowledge, no clinical trial has yet evaluated the effect of P. oleracea extract in combination with a low-calorie diet on metabolic parameters in patients with NAFLD except for the study by Darvish Damavandi et al., which showed that P. oleracea extracts at a dose of 300 mg/day for 12 weeks had no significant effect on hepatic enzymes, lipid profiles, or glycemic indices in patients with NAFLD. They also declared that the dose of P. oleracea extract used in their study might have been insufficient to affect the clinical results (41).
The various clinical applications and the general lack of knowledge regarding the benefits and drawbacks of P. oleracea in patients with NAFLD make this study extremely pertinent. The study's advantages include a randomized, double-blinded design, the publication of the protocol, the evaluation of dietary outcomes and level of physical activity, and the documentation of any potential issues that patients may have reported.
4.1. Conclusions
We provide the methodology for a clinical study design to evaluate the effects of a hydro-ethanolic extract of aerial parts of Portulaca oleracea supplementation on clinical and paraclinical findings in patients with non-alcoholic fatty liver disease. We anticipate that oral P. oleracea supplementation of 700 mg/day for two months will enhance clinical outcomes and reduce inflammation and oxidative stress in NAFLD patients. The current study's findings, whether positive or negative, could provide a significant shift in the evidence guiding current and future policy on the use or non-use of Portulaca oleracea extract as a supplemental treatment for NAFLD patients.
4.2. Study Limitations
• Incomplete adherence to the dietary regimen by some participants is one of the limitations of this research. However, it is important to note that this issue is not considered a weakness but rather one of the limitations inherent in lifestyle modification studies. Based on the results of published studies, only 30% of participants in lifestyle modification programs for non-alcoholic fatty liver disease were able to achieve the desired weight reduction of more than 5% after one year (52).
• Another limitation of this study is the provision of dietary plans based on a substitution list of food items and the assessment of patients' diets using the Nutritionist IV software. This can make it challenging to assess patients' compliance with the dietary plans.
• Lack of long-term follow-up is another limitation of this study. It is recommended that future studies extend the follow-up period to address this limitation.