1. Context
Non-communicable diseases (NCDs) impose a heavy burden on health systems and are considered the leading cause of premature death and disability worldwide. Studies indicate that about 80% of NCD-related deaths occur in low- and middle-income countries (1). There are many risk factors for NCDs, such as smoking, alcohol consumption, unhealthy diets, physical inactivity, and obesity. Environmental, social, political, and commercial factors are also involved in the development of NCDs. Urbanization is considered one of the primary factors increasing the burden of NCDs. The increased consumption of processed, high-calorie, high-fat, and salty foods and sedentary lifestyles may establish a relationship between urbanization and the risk of NCDs. There is also a strong correlation between the socioeconomic status of individuals and the risk of NCDs in high-income countries (2). Since NCDs require longer-term care, healthcare systems should provide advanced equipment to patients with such diseases (3). Similar to other developing countries, Iran also suffers from a high burden of NCDs; a report by the World Health Organization (WHO) indicates that 76% of the 395,000 deaths registered in Iran in 2014 were caused by NCDs (4). Fatty liver disease (FLD) is a significant non-communicable disease (NCD) and a leading cause of chronic liver disease (CLD) globally, including in Iran. Its rising prevalence poses a major public health concern due to its association with other NCDs such as cardiovascular disease, type 2 diabetes, and obesity. Recent data indicate a steady increase in FLD cases in Iran, attributed to urbanization, sedentary lifestyles, and dietary shifts toward high-calorie processed foods. If left unaddressed, this trend could contribute to a significant rise in healthcare costs and NCD-related mortality, highlighting the urgent need for effective prevention policies (5). Those who do not consume alcohol may develop another condition in this category called non-alcoholic fatty liver disease (NAFLD), which is considered a serious health issue. Various studies have reported the global prevalence of FLD to be 10 - 24% in healthy individuals and 57 - 74% among obese and diabetic individuals; its prevalence in Iran is reported to be 2.09 - 2.90%. Considering the significant relationship between the prevalence of FLD and the mortality caused by cardiovascular and brain diseases, this condition should be viewed as a serious phenomenon resulting from urban and mechanical life. Moreover, there is a need for suitable treatment programs and interventions to reduce its prevalence (6). The global prevalence of FLD is about 20 - 30% in the general population and 70 - 90% among obese or diabetic individuals. However, it also affects 10 - 15% of the lean population (7). Iran is the second-largest country in the Middle East, with a population of over 80 million people, most of whom live in urban areas. This country has been undergoing a critical period of transition from the epidemic of communicable diseases to the epidemic of NCDs over the past few decades (8). Iran’s Ministry of Health and Medical Education established the National Committee for Prevention and Control of Non-communicable Diseases to address the growing burden of chronic conditions, including FLD. This committee aims to reduce the prevalence of NCDs by promoting health education, supporting early diagnosis, implementing preventive measures, and improving access to healthcare services. However, while the National Document for NCD Prevention outlines general strategies, there is limited clarity on specific FLD-focused policies, creating a gap in evidence-based strategies for FLD prevention and control. Conducting this systematic review is crucial as it synthesizes current policies addressing FLD prevention, offering insights that can inform future public health interventions. Identifying successful strategies will help policymakers and healthcare providers implement more effective, evidence-based measures to reduce FLD risk and improve public health outcomes in Iran. Such measures make it possible to control the burden of this epidemic in Iran by creating an inter-sectoral and intra-sectoral cooperation network (1). Considering the risks of FLD, as an NCD, to the health of Iranian society, it is necessary to adopt appropriate policies to reduce the risk of this disease and, thereby, improve the health system’s performance (9). However, no coherent and systematic studies have addressed the policies developed in Iran to reduce the risk of FLD.
2. Objectives
The present systematic review aims to identify the general policies adopted in Iran to reduce the risk of this disease.
3. Methodology
3.1. Method
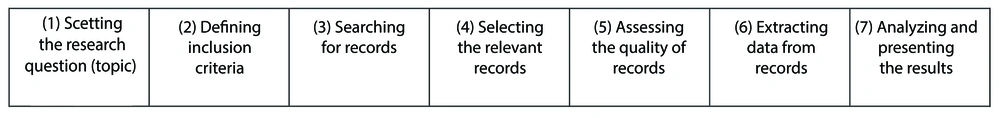
This study was conducted using the Cochrane systematic review methodology, a widely recognized and rigorous approach for synthesizing evidence in health research. This methodology is known for its structured process, which minimizes bias and ensures transparency by following a systematic and replicable process (10). The Cochrane approach was selected for its reliability in summarizing policy interventions related to FLD prevention, providing high-quality evidence for decision-making. The method consists of seven key steps: Identifying the research question, defining inclusion and exclusion criteria, searching for records, selecting relevant records, assessing study quality, data extraction, and synthesizing results (Figure 1).
The data in this systematic review were collected through library research. Because systematic reviews involve multiple steps, one of their key features is their high reliability or repeatability. This approach is an effective tool for searching and reviewing studies that can address research questions (11).
3.2. Handling Missing Data
In this systematic review, missing data in the included studies were managed as follows (12):
1. Studies with missing data: Any studies with incomplete information relevant to our research questions (e.g., missing policy details or outcomes) were carefully reviewed.
2. Contacting authors: When critical data were missing, attempts were made to contact the authors of the respective studies to obtain the necessary information.
3. Exclusion criteria: Studies with significant missing data that could not be clarified or supplemented were excluded during the selection process to ensure the integrity of the analysis.
3.3. Heterogeneity Analysis
To account for variations across the included studies, we assessed heterogeneity using the I2 statistic. This measure quantified the proportion of variance across studies attributable to heterogeneity rather than chance. An I2 value of 0% indicated no observed heterogeneity, while values of 25%, 50%, and 75% represented low, moderate, and high heterogeneity, respectively (13).
3.4. Certainty of Evidence
We evaluated the certainty of evidence using the grading of recommendations assessment, development, and evaluation (GRADE) approach. This framework considers factors such as study limitations, inconsistency, indirectness, imprecision, and publication bias to assess the quality of evidence as high, moderate, low, or very low (14). This assessment was included in the discussion of the findings to provide a clear understanding of the reliability of the conclusions.
3.5. Statistical Population
This systematic review searched and reviewed papers published in reputable journals from 2015 to 2024 to identify the policies developed worldwide to reduce the risk of FLD as an NCD. In other words, this study employed library research to extract qualitative data from papers on FLD and the policies to reduce its risk. As a result, the study population consisted of papers on FLD as an NCD, published from 2015 to 2024. The systematic review method was used for sampling, which will be explained in the findings section.
4. Results
This systematic review identified the policies developed worldwide to reduce the risk of FLD. For this purpose, the Cochrane systematic review methodology was employed to search and review the papers on this subject published from 2015 onwards.
Step 1: Setting the research question (topic): Since this systematic review focused on policies for reducing the risk of FLD, the research team needed to have the knowledge and expertise in the field of health and NCDs. As a result, the supervisors and advisors of the research greatly contributed to setting the research question or topic (the policies developed around the world for reducing the risk of FLD), given their significant experience in the health and medical fields.
Step 2: Defining the inclusion criteria: An important step in any systematic review is to set the inclusion criteria based on the topic and type of records. For example, one of the inclusion criteria in this systematic review was the presence of keywords in the title of studies. Table 1 presents the inclusion criteria used in this systematic review to search the relevant papers.
| Categories | Inclusion Criteria |
|---|---|
| English keywords (with equivalent Farsi terms for Farsi databases) | (1) NCDs; (2) FLD; (3) policies to reduce the risk of NCDs (especially FLD) |
| Methods | (1) Qualitative; (2) quantitative |
| Data collection | (1) Library research; (2) field study |
| Date of publication | Studies conducted during the past 9 years |
| Scientific-research | Papers published in scientific research journals |
Abbreviations: FLD, fatty liver disease; NCDs, non-communicable diseases.
As shown in the above table, the main inclusion criteria in this systematic review were the presence of research keywords (NCDs, FLD, and policies to reduce the risk of FLD) in the title of studies, qualitative and quantitative methods, library and field research as data collection methods, papers published between 2015 to 2024, and papers published in scientific-research journals. The papers that met these criteria were selected for further review and analysis. With the inclusion criteria established, the next phase involved a comprehensive search for relevant studies across multiple databases to ensure thorough coverage of the literature.
Step 3: Searching for papers: The table below shows the main databases where the relevant Farsi and English papers were searched in this systematic review.
Table 2 shows that the papers were searched on various databases using common indices. While many recently published papers are indexed in different databases, newer papers are indexed relatively earlier in SID, whereas dissertations and theses can be more easily found on IranDoc. The systematic review employed a comprehensive search strategy tailored to each database. The systematic search was conducted using both free-text keywords and medical subject headings (MeSH) terms to ensure comprehensive literature coverage. The following MeSH terms were used in combination with Boolean operators: "Non-Communicable Diseases", "Fatty Liver Disease", and "Non-Alcoholic Fatty Liver Disease", with equivalent Farsi terms for Farsi databases. The search was conducted in English-language databases (Medline, Embase, Google Scholar, Cochrane Library) and Farsi-language databases (SID, IranDoc, Magiran) from 2015 to 2024. Filters were applied to limit results to peer-reviewed journal articles and exclude gray literature. After completing the database searches, the next step was the selection of relevant studies based on the inclusion criteria.
| Language of Records | Databases |
|---|---|
| Farsi | SID |
| IranDoc | |
| Magiran | |
| English | Medline |
| Embase | |
| Google Scholar | |
| Cochrane |
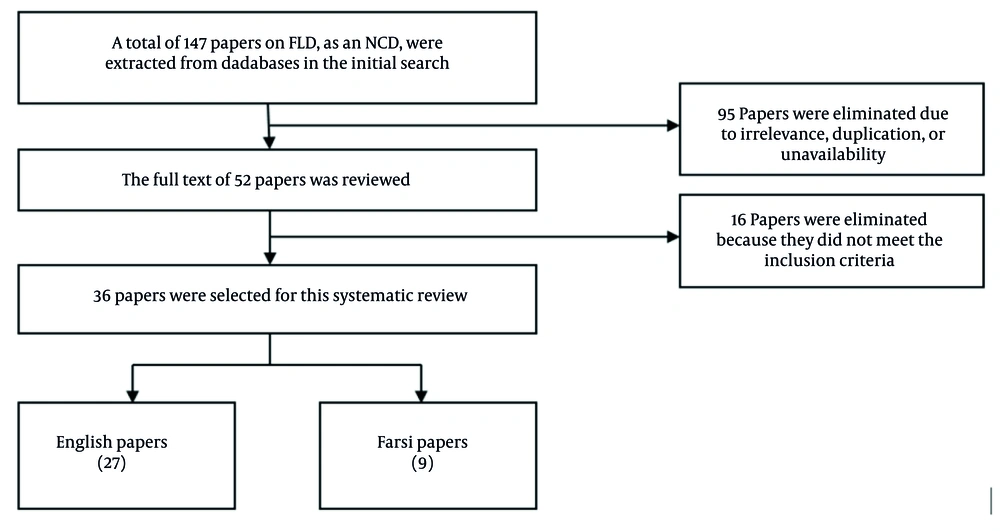
Step 4: Selecting the relevant studies: To find the most relevant papers, the keywords were searched in the abstract of the extracted papers. After irrelevant papers were eliminated, the full text of the papers was prepared for analysis. It was crucial to select the relevant papers and eliminate the irrelevant ones. Initially, 147 records (including 54 Farsi and 93 English records) were extracted based on the searched keywords. Figure 2 flowchart depicts the stepwise selection process of articles included in this systematic review, demonstrating the rigorous filtering of studies from initial identification through final inclusion based on predefined criteria.
As illustrated in Figure 2, a total of 147 papers on the research subject were extracted from databases in the initial search, of which 90 papers were eliminated due to irrelevance and duplication, and 5 papers due to unavailability. As a result, the full text of 52 papers was reviewed. Among them, 16 papers that did not meet the inclusion criteria were excluded from the study. Finally, 36 papers were selected for this systematic review.
Step 5: Assessing the quality of papers: Based on the Cochrane systematic review methodology, the quality of selected papers was assessed through a dual-reviewer system to ensure methodological rigor. One reviewer was from the research team, while the second was an independent expert not involved in the study, adding layer of objectivity and reducing the risk of selection bias. Discrepancies were resolved through discussion, ensuring consistency and minimizing subjective influences. This systematic approach reinforced the credibility of the study selection process and ensured that only high-quality studies were included, directly contributing to the reliability and validity of the overall findings. Finally, all the papers selected for this systematic review were checked and confirmed by the research supervisor, who specialized in the research subject, i.e., policies for reducing the risk of non-communicable FLD.
Step 6: Extracting data from articles: In this step, the policies for reducing the risk of non-communicable FLD were extracted from the selected papers. Table 3 presents the general information of the reviewed papers and the relevant policies extracted from them.
| Policies | Frequency | Study Titles and References |
|---|---|---|
| Health education | 7 | Prevalence of non-alcoholic fatty liver disease in Iranian children and adolescents: A systematic review (15) |
| The burden of non-communicable diseases and its associated economic costs in India (3) | ||
| Urban social determinants of non-communicable disease risk factors in argentina. health and place (2) | ||
| Implementation status of non-communicable disease control program at primary health care level in Bangladesh: Findings from a qualitative research (16) | ||
| Effect of brief interventions to promote behavior change on clinical outcomes of selected non-communicable diseases: The World Health Organization package of essential non-communicable disease interventions for primary health care settings: Protocol of a quasi-experimental study (17) | ||
| Assessment of health education in the prevention of non-communicable chronic disease complications: Systematic review (18) | ||
| Relationships between education and non-alcoholic fatty liver disease (19) | ||
| Promotion of healthy behavioral patterns | 7 | Lifestyle and non-alcoholic fatty liver disease: A review study (20) |
| Assessing the association between corporate financial influence and implementation of policies to tackle commercial determinants of non-communicable disease: A cross-sectional analysis of 172 countries (21) | ||
| Non-communicable disease comorbidity and associated factors in tuberculosis patients: A Cross-sectional study in Gabon (22) | ||
| Lignosus rhinoceros attenuates non-alcoholic fatty liver induced by plant-based high-fat diet in Hamsters (23) | ||
| Is fatty liver associated with increased mortality and morbidity in coronavirus disease? (24) | ||
| Nutrition could prevent or promote non-alcoholic fatty liver disease: An opportunity for intervention (25) | ||
| Risk prevention and health promotion for non-alcoholic fatty liver diseases (NAFLD) (26) | ||
| Increasing tariffs on harmful products | 1 | Toward a third term of health Japan 21 – implications from the rise in non-communicable disease burden and highly preventable risk factors (27) |
| Integration of health services | 5 | Primary health care system responses to non-communicable disease prevention and control: A scoping review of national policies in Mainland China since the 2009 health reform (9) |
| Assessing the association between corporate financial influence and implementation of policies to tackle commercial determinants of non-communicable disease: A cross-sectional analysis of 172 countries (21) | ||
| A model of integrated prevention and control of non-communicable diseases in Iran (28) | ||
| Implementation status of non-communicable disease control program at primary health care level in Bangladesh: Findings from a qualitative research (16) | ||
| Expanding public health responses to non-communicable diseases: The NAFLD model of India (29) | ||
| Early diagnosis | 7 | Effect of brief interventions to promote behavior change on clinical outcomes of selected non-communicable disease: The World Health Organization package of essential non-communicable disease interventions for primary health care settings: Protocols of a quasi-experimental study (17) |
| Is fatty liver associated with increased mortality and morbidity in coronavirus disease? (24) | ||
| Non-alcoholic fatty liver disease development: A multifactorial pathogenic phenomenon (7) | ||
| American association of clinical endocrinology clinical practice guideline for the diagnosis and management of non-alcoholic fatty liver disease in primary care and endocrinology clinical settings (30) | ||
| The importance of population studies in the control of non-communicable diseases: Achievements of non-communicable Diseases Research Center- Endocrine and Metabolism Research Institute (1) | ||
| Nonalcoholic fatty liver disease: Disease burden and disease awareness (31) | ||
| Incidence and early detection of patients with nonalcoholic fatty liver disease: A QI project (32) | ||
| Health justice | 6 | An overview of non-alcoholic fatty liver disease (33) |
| Toxoplasmosis in patients with chronic Hepatitis C and fatty liver disease (34) | ||
| Human development index adjusted based on inequality: an important predictor of deaths caused by non-communicable diseases in the world and Iran: An ecological study (4) | ||
| Primary health care system responses to non-communicable disease prevention and control: A scoping review of national policies in Mainland China since the 2009 health reform (9) | ||
| Expanding public health responses to non-communicable diseases: The NAFLD model of India (29) | ||
| Nutrition could prevent or promote non-alcoholic fatty liver disease: An opportunity for intervention (25) | ||
| Intervention in critical leverage points | 5 | A protocol for a systematic review of inter-sectoral interventions to reduce non-communicable disease risk factors in African cities (35) |
| The importance of population studies in the control of non-communicable diseases: Achievements of Non-Communicable Diseases Research Center-Endocrine and Metabolism Research Institute (1) | ||
| Classification of risk factors for non-communicable diseases in different provinces of Iran using multivariate factorial methods (36) | ||
| A global action agenda for turning the tide on fatty liver disease (37) | ||
| Lifestyle interventions for non-obese patients both with, and at risk, of non-alcoholic fatty liver disease (38) | ||
| Individual interventions | 4 | Effect of brief interventions to promote behavior change on clinical outcomes of selected non-communicable disease: The World Health Organization package of essential non-communicable disease interventions for primary health care settings: Protocols of a quasi-experimental study (17) |
| Lifestyle and non-alcoholic fatty liver disease: A review study (20) | ||
| Lifestyle changes in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis (39) | ||
| Lifestyle interventions for non-obese patients both with, and at risk, of non-alcoholic fatty liver disease (38) | ||
| Medical and insurance services | 3 | Study on the effect of different types of sugar on lipid deposition in goose fatty liver (40) |
| Primary health care system responses to non-communicable disease prevention and control: A scoping review of national policies in Mainland China since the 2009 health reform (9) | ||
| Healthcare and socioeconomic costs of NAFLD: A global framework to navigate the uncertainties (41) | ||
| Investment in health and hygiene infrastructure | 3 | Implementation status of non-communicable disease control program at primary health care level in Bangladesh: Findings from a qualitative research (16) |
| Non-alcoholic fatty liver disease and the impact of genetic, epigenetic, and environmental factors in the offspring (42) | ||
| Healthcare and socioeconomic costs of NAFLD: A global framework to navigate the uncertainties (41) | ||
| Promotion of healthy nutritional patterns and eating habits | 5 | Effects of artichoke on risk factors for fatty liver disease (6) |
| Human Development Index adjusted based on inequality: An important predictor of deaths caused by non-communicable diseases in the world and Iran: An ecological study (4) | ||
| American association of clinical endocrinology clinical practice guideline for the diagnosis and management of non-alcoholic fatty liver disease in primary care and endocrinology clinical settings (30) | ||
| Nutrition could prevent or promote non-alcoholic fatty liver disease: An opportunity for intervention (25) | ||
| The association between major dietary patterns with the risk of non-alcoholic fatty liver disease, oxidative stress and metabolic parameters: A case-control study (43) |
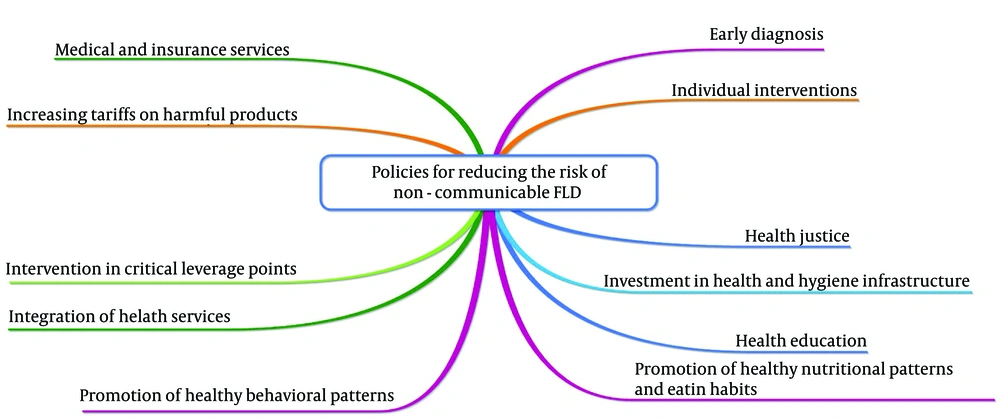
To enhance the clarity of the findings, a visual summary has been included to present the key policies identified in the systematic review. Figure 3 provides an overview of the most frequently cited strategies, offering a clearer understanding of the distribution and emphasis of various FLD prevention policies.
Step 7: Analyzing and presenting the data: The results of this systematic review indicated that the policies generally adopted around the world for reducing the risk of NCDs, especially FLD, included health education, promotion of healthy behavioral patterns, increasing tariffs on harmful products, integration of health services, early diagnosis, health justice, intervention in critical leverage points, individual interventions, medical and insurance services, investment in health and hygiene infrastructure, and promotion of healthy nutritional patterns and eating habits. These results will be discussed in detail, and some recommendations will be presented in the next section of this study.
Furthermore, the heterogeneity analysis indicated an I2 value of 30%, suggesting moderate heterogeneity across the included studies. This level of heterogeneity is considered acceptable, given the diversity in study designs and populations, and does not compromise the overall validity of the findings. Additionally, the GRADE assessment rated the certainty of evidence as moderate to high, affirming the reliability of the data and its suitability for informing policy recommendations.
5. Discussion
This systematic review identified the policies adopted worldwide for reducing the risk of FLD as an NCD. A systematic review is a method used to find an answer to the research questions based on the evaluation of all available studies about the questions. One of the reasons why this study employed the systematic review methodology is that health managers and professionals may lack enough time or skills to collect, evaluate, and integrate all relevant papers. The relevant papers were collected by searching keywords (NCDs, FLD, and policies to reduce the risk of FLD) on both Farsi and English databases.
As shown in the flowchart of selecting relevant papers for this systematic review (Figure 2), a total of 147 papers on the research subject were extracted from databases in the initial search, of which 90 papers were eliminated due to irrelevance and duplication, and 5 papers due to unavailability. As a result, the full text of 52 papers was reviewed. Among them, 16 papers that did not meet the inclusion criteria were excluded from the study. Finally, 36 papers were selected for the systematic review.
The results of this systematic review indicated that the policies generally adopted around the world for reducing the risk of NCDs, especially FLD, included health education (2, 3, 15-19), promotion of healthy behavioral patterns (20-26), increasing tariffs on harmful products (27), integration of health services (9, 16, 21, 28, 29), early diagnosis (1, 7, 17, 24, 30-32), health justice (4, 9, 25, 29, 33, 34), intervention in critical leverage points (1, 35-38), individual interventions (17, 20, 38, 39), medical and insurance services (9, 40, 41), investment in health and hygiene infrastructure (16, 41, 42), and promotion of healthy nutritional patterns and eating habits (4, 6, 25, 30, 43). Implementing these strategies can lead to significant health improvements by raising awareness, encouraging preventive behaviors, and facilitating early detection. In Iran, where the burden of NCDs like FLD is rising, these measures could reduce healthcare costs and lower FLD-related morbidity. On a global scale, the adoption of similar policies has shown positive health outcomes, emphasizing the importance of a multi-faceted approach to FLD prevention.
5.1. Conclusions
Some of the above-mentioned policies for reducing the risk of non-communicable FLD are macro-level, whereas others are considered individual. In other words, people can reduce the risk of such diseases by following a series of behavioral patterns (e.g., avoiding high-fat foods and smoking) and individual interventions. However, other policies should be adopted and managed by health organizations and governments, such as medical and insurance services, health education, increasing tariffs on harmful products, intervention in critical leverage points, and investment in health and hygiene infrastructure.
To ensure successful implementation, collaboration among government officials, healthcare providers, policymakers, and community organizations is essential. Stakeholders should work together to implement these strategies, monitor their effectiveness, and adjust interventions based on evolving public health needs. A collective and sustained effort will be crucial to combating the rising burden of FLD and other NCDs, ultimately contributing to long-term health improvements and reduced healthcare costs.
Based on the study findings, the following practical recommendations can be proposed to relevant officials:
1. Health education: Health officials are recommended to develop comprehensive educational programs and interventions to raise people’s awareness of the risk factors for FLD and strategies to control them effectively. Such programs and interventions should be presented to different target groups, such as young people, adults, and older people, in an attractive and interactive manner.
2. Promotion of healthy behavioral patterns: Promotion of healthy behavioral patterns, such as proper nutrition and regular exercise, can also help reduce the risk of non-communicable FLD. Such programs should emphasize the cultural and social principles of the target community and propose practical solutions.
3. Higher tariffs on harmful products: Another policy that can reduce the risk of FLD is to impose higher tariffs on unhealthy products such as soft drinks containing synthetic sweeteners, high-fat and low-quality foods, and other unhealthy food products. However, it is necessary to investigate how such a policy is implemented and what its consequences are.
4. Integration of healthcare services: Developing an integrated and coordinated healthcare system for early diagnosis and management of FLD is crucial. There is a need for programs and policies that aim to establish effective coordination and communication between different levels of the healthcare system, provide comprehensive and timely services, and facilitate access to diagnostic and therapeutic services for patients with FLD.
5. Early diagnosis: The development and implementation of programs for the early diagnosis of FLD can help identify the disease in its early stages and initiate therapeutic measures promptly. Such programs should involve training both the community and health professionals and include applying effective diagnostic methods such as blood tests and ultrasound.
6. Health justice: One of the main goals of any health system is to ensure equal access to health services for all, especially low-income groups. The adoption of policies that facilitate equal access to the health and medical services necessary for the prevention and treatment of FLD will effectively reduce the risk of this disease.
7. Intervention in critical leverage points: It is important to identify areas where FLD is more prevalent. The FLD incidence can be reduced by programs and policies that specifically target these areas and provide measures to improve the health status and nutritional conditions of people there.
8. Individual interventions: Encouraging individuals to engage in appropriate interventions and health-promoting behaviors is a key strategy to reduce the risk of FLD. Training people on the benefits of a healthy diet, regular exercise, and self-care practices, as well as the disadvantages of harmful products, can help promote healthy lifestyle choices and reduce the risk of FLD.
9. Medical and insurance services: Providing appropriate and accessible medical services to people with FLD is another strategy for lowering the risk. Since the number of papers related to studies conducted in countries other than Iran outnumbered those related to domestic studies in this systematic review, future studies are recommended to investigate this subject using interview-based approaches, such as grounded theory, to identify the localized policies adopted to reduce the risk of FLD.
The findings suggest that comprehensive educational initiatives, economic policies, and health service integration can effectively reduce the risk of FLD. However, this study has certain limitations. As a systematic review, it relies on previously published data, which may vary in quality and scope across the included studies. Additionally, the lack of long-term outcome data on policy effectiveness limits the ability to draw causal conclusions. Future research should explore the real-world impact of these policy interventions through longitudinal studies and consider qualitative approaches, such as expert interviews or focus groups, to gain deeper insights into policy implementation challenges and successes.