1. Background
Hepatitis D virus (HDV), also known as delta factor, is an incomplete virus that requires the presence of hepatitis B virus (HBV) surface antigen (HBsAg) to enter cells and cause infection (1). Consequently, HDV is only observed in patients positive for HBsAg. The HDV infection can occur in two forms: Co-infection or super-infection, both in the presence of acute or chronic HBV infection, respectively. Co-infection with HBV and HDV results in a more severe disease course and higher mortality risk compared to HBV infection alone (2). The HDV exacerbates both acute and chronic HBV infections. Evidence suggests that while HBV, which integrates into the DNA of host cells, takes years to transform and cause liver cancer, the addition of HDV in these patients accelerates the progression of the disease to cirrhosis and liver cancer (3). Co-infection of HDV with HBV leads to fatal fulminant hepatitis in 20-30% of cases, compared to only 2% in patients with HBV without concurrent HDV infection (4). In a study following 69 chronic HBV carriers simultaneously infected with HDV for at least 36 months, 12% developed cirrhosis, and 9% developed liver cancer. In contrast, during the same follow-up period, among 1,058 patients without HDV infection, only 4% developed liver cirrhosis, and 3% developed liver cancer (5).
The routes of HDV transmission are similar to those of HBV, including injectable, mucosal, blood, perinatal, and sexual transmission (6). In the laboratory diagnosis of acute delta virus infection, IgM-anti HDV is helpful, while IgG-anti HDV is used to diagnose past delta virus infections (7). The ELISA method can detect Delta antigen in blood during acute HDV infection. Additionally, in cases with the chronicity of the disease, the gold standard for diagnosing delta hepatitis is liver biopsy and the detection of HDV antigen in liver cells (8).
Infections caused by HBV, hepatitis C virus (HCV), and HDV pose significant health challenges in low-income countries, particularly in Afghanistan (9). Studies on viral hepatitis in Afghanistan are limited and have yielded conflicting results (9). Despite the studies conducted in Iran, the risk factors for hepatitis D have not been thoroughly investigated in many regions of the country, especially in the eastern provinces of Iran, bordering the western provinces of Afghanistan. Given the more challenging treatment and more aggressive course of HBV/HDV co-infection, all patients with HBV must be screened for HDV infection. However, due to limited resources in developing countries like Iran and Afghanistan, it may not be feasible to perform HDV screening in all HBV patients.
2. Objectives
Considering the factors mentioned above, the present study aimed to investigate and compare the seroprevalence of HDV in patients with HBV in the border provinces of Iran and Afghanistan.
3. Methods
3.1. Study Design
This descriptive cross-sectional study aimed to assess the seroprevalence of HDV among HBVcarriers in the border provinces of Iran (Razavi Khorasan, South Khorasan, and Sistan and Baluchestan) and Afghanistan (Herat, Farah, and Nimroz).
3.2. Study Setting and Population
The study was conducted in the border provinces of Iran and Afghanistan. Participants were selected from healthcare centers, hospitals, and diagnostic laboratories in these regions, focusing on HBsAg-positive patients.
3.3. Sampling Method
A convenience sampling method was employed, including all eligible HBsAg-positive patients attending the healthcare facilities during the study period. Only patients who provided informed consent were included. Participants were from diverse backgrounds, with varying ages, genders, and risk factors related to HBV infection.
3.4. Sample Size Calculation
The sample size was calculated using the formula for prevalence studies:
Z: 1.96 (95% confidence level)
P: 0.031 [HDV seroprevalence in Iran (10)] and 0.021 [HDV seroprevalence in Afghanistan (11)]
d: 0.05 (margin of error)
The minimum sample size required was 45 for Iran and 32 for Afghanistan. The final sample size was increased to 350 to ensure statistical power. In Iran, samples were collected from the eastern provinces, including Sistan and Baluchestan (100 samples), South Khorasan (75 samples), and Razavi Khorasan (65 samples). In Afghanistan, 110 samples were collected from the provinces of Herat, Farah, and Nimroz.
3.5. Data Collection
Data were collected through a structured questionnaire, which captured demographic details (e.g., age, gender, marital status, and living status) and risk factors (e.g., history of cupping and tattoos). Serum samples were collected from each participant for subsequent HDV testing.
3.6. Laboratory Methods
The HDV antibodies were detected using an ELISA kit (DIA.PRO, Italy), following a two-step competitive incubation process. First, the serum sample is added, allowing anti-HDV antibodies to bind to the antigen. After washing, an enzyme-conjugated polyclonal antibody binds to any unoccupied antigen sites. Following the addition of a chromogen/substrate mixture, enzyme activity is inversely proportional to the concentration of anti-HDV antibodies. The kit’s sensitivity and specificity are greater than 98%. The concentration of HDV-specific antibodies was determined using a semi-quantitative cut-off value.
3.7. Data Analysis
Statistical analysis was performed using SPSS Statistics 27.0.1 software. The relative frequency of HDV seroprevalence across demographic and risk factor subcategories was determined. The relationship between categorical variables (e.g., age groups, gender, marital status, and living status) and HDV status (positive or negative) was analyzed using the chi-square test or Fisher's exact test, depending on expected cell counts. A P-value of less than 0.05 was considered statistically significant.
4. Results
4.1. Patient Characteristics
A total of 350 HBsAg-positive patients were included in the study, consisting of 200 men (57.14%) with a mean age of 46.46 ± 11.99 years and 150 women (42.86%) with a mean age of 40.77 ± 10.80 years. Among the 271 participants with recorded marital status, 231 (85.2%) were married, 23 (8.5%) were single, 12 (4.4%) were divorced, and 5 (1.8%) were in polygamous relationships. The participants' places of residence were distributed as follows: Sixty five (18.6%) in Mashhad (the capital of Razavi Khorasan province), 75 (21.4%) in Birjand (the capital of South Khorasan province), 100 (28.6%) in Zahedan (the capital of Sistan and Baluchestan province), and 110 (31.4%) in the three border provinces of Afghanistan (Table 1).
| Variables | Study Patients | P-Value | ||
|---|---|---|---|---|
| All | HDV Positive | HDV Negative | ||
| Gender | 0.51 | |||
| Male | 200 (57.14) | 23 (11.5) | 177 (88.5) | |
| Female | 150 (42.86) | 14 (9.3) | 136 (90.7) | |
| Marital status | 0.37 | |||
| Single | 23 (8.5) | 2 (8.7) | 21 (91.3) | |
| Married | 231 (85.2) | 25 (10.8) | 206 (89.2) | |
| Divorced | 12 (4.4) | 3 (25) | 9 (75) | |
| Polygamy | 5 (1.8) | 0 | 5 (100) | |
| Living status | 0.004 | |||
| Mashhad | 65 (18.6) | 3 (4.6) | 62 (95.4) | |
| Birjand | 75 (21.4) | 2 (2.7) | 73 (97.3) | |
| Zahedan | 100 (28.6) | 13 (13) | 87 (87) | |
| Afghanistan | 110 (31.4) | 19 (17.3) | 91 (82.7) | |
| Age (y) | 0.48 | |||
| < 25 | 13 (4.7) | 1 (7.7) | 12 (92.3) | |
| 26 - 35 | 57 (20.7) | 5 (8.8) | 52 (91.2) | |
| 36 - 45 | 86 (31.3) | 7 (8.1) | 79 (91.9) | |
| 46 - 55 | 65 (23.6) | 11 (16.9) | 54 (83.1) | |
| > 56 | 54 (19.6) | 6 (11.1) | 48 (88.9) | |
General Characteristics of Chronic Hepatitis B Patients a
4.2. Hepatitis D Virus Status and Group Comparisons
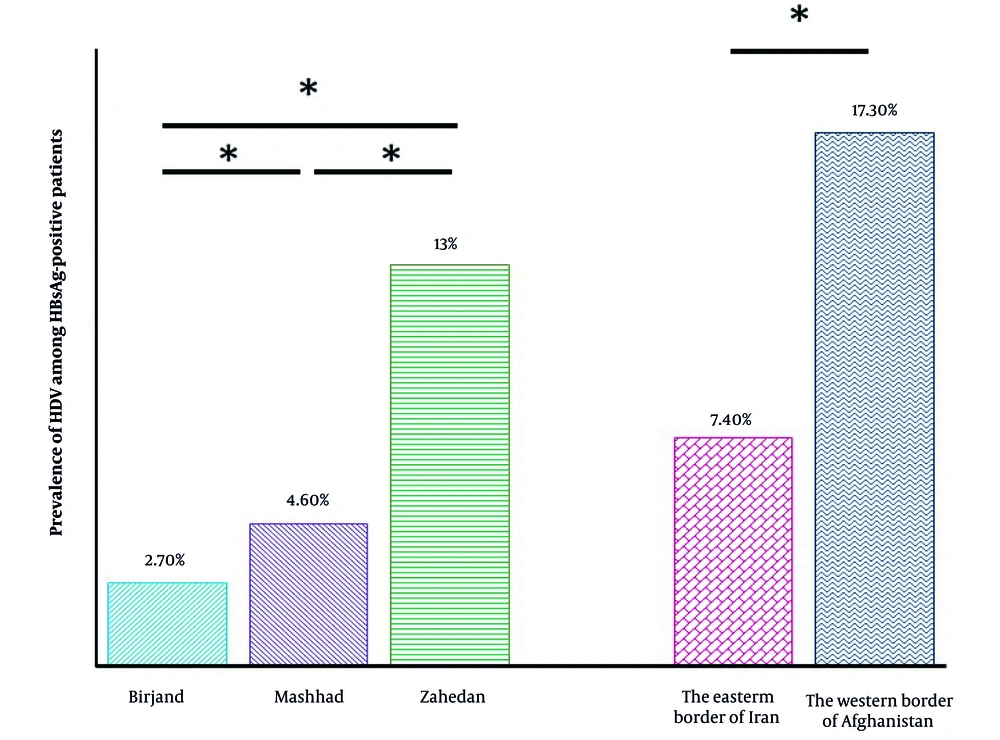
Based on HDV status, two groups were formed: Thirty seven patients (10.57%) with positive anti-HDV tests were classified as HDV positive, and 313 patients (89.43%) with negative anti-HDV tests were classified as HDV negative. Among men, the seroprevalence of HDV was 23 (11.5%), while among women, it was 14 (9.3%). Comparative analysis of the HDV-positive and HDV-negative groups revealed no statistical differences in male-to-female ratio (P = 0.51), marital status (P = 0.37), or age (P = 0.48). Our findings reveal that the seroprevalence of HDV among the HBsAg-positive patients in Iran is significantly lower (7.4%) than the seroprevalence of HDV among the HBsAg-positive patients in the three border provinces of Afghanistan (17.3%) (P = 0.023) (Figure 1). Finally, a significant difference was observed between the place of residence in the HDV-positive and HDV-negative groups (P = 0.004) (Table 1).
Percentage of the seroprevalence of hepatitis D virus (HDV) among hepatitis B surface antigen (HBsAg)-positive patients. The seroprevalence of HDV among the HBsAg-positive patients in Mashhad, Birjand, and Zahedan is significantly lower (4.6%, 2.7%, and 13% respectively) than the seroprevalence of HDV among the HBsAg-positive patients in the three border provinces of Afghanistan (17.3%). The graph shows significance levels with one star (*) for P-values less than 0.05.
4.3. Risk Factors
Various risk factors were investigated, including a history of jaundice, cupping, alcohol consumption, tattooing, major surgery, injection addiction, accident or trauma, endoscopy, front, and life or travel abroad. The results showed that among the participants with a positive anti-HDV test, 1 out of 31 (3.2%) had a history of jaundice (P = 0.16), 4 out of 44 (9.1%) had a history of cupping (P = 0.72), 4 out of 20 (20%) had a history of tattooing (p = 0.16), 12 out of 80 (15%) had a history of major surgery (P = 0.15), 7 out of 36 (19.4%) had a history of endoscopy (P = 0.07), and 18 out of 56 (32.1%) had a history of living or traveling abroad (P < 0.001). Notably, none of the participants with a history of alcohol consumption (n = 4) (P = 1), history of injecting drug addiction (n = 4) (P = 0.44), trauma (n = 5) (P = 0.66), or war (n = 12) (p = 0.22) tested positive for anti-HDV. Comparative analysis of the HDV positive and HDV negative groups revealed no statistically significant differences in any of the risk factors, except for the history of living or traveling abroad (P < 0.001) (Table 2).
| Variables | Study Patients | P-Value | ||
|---|---|---|---|---|
| HDV Positive | HDV Negative | All | ||
| Jaundice history (yes) | 1 (3.2) | 30 (96.8) | 31 (8.9) | 0.16 |
| Cupping history (yes) | 4 (9.1) | 40 (90.9) | 44 (12.7) | 0.72 |
| Alcohol consumption history (yes) | 0 | 4 (100) | 4 (1.14) | 1 |
| History of tattooing (yes) | 4 (20) | 16 (80) | 20 (5.7) | 0.16 |
| History of major surgery (yes) | 12 (15) | 68 (85) | 80 (22.98) | 0.15 |
| History of injection addiction (yes) | 0 (0) | 4 (80) | 4 (1.15) | 0.44 |
| History of accident and trauma (yes) | 0 | 5 (100) | 5 (1.43) | 0.66 |
| History of endoscopy (yes) | 7 (19.4) | 29 (80.6) | 36 (10.35) | 0.07 |
| History of the Front (yes) | 0 | 12 (100) | 12 (3.45) | 0.22 |
| Living or traveling to another country (yes) | 18 (32.1) | 38 (67.9) | 56 (16.1) | < 0.001 |
Risk Factors in Chronic Hepatitis B Patients a
5. Discussion
This study aimed to assess the seroprevalence of HDV among carriers of HBV in the border provinces of Iran and Afghanistan. Additionally, our study highlighted various demographic and behavioral factors that may influence HDV infection. Studies have reported HDV seroprevalence among HBsAg-positive patients in neighboring countries like Turkey (9.6%) (12), Iraq (6.6%) (13), and Pakistan (14.66%) (14). Among Afghan immigrants in Iran, the rate was 26.6% (15). Our findings indicated that the seroprevalence of HDV in Afghanistan's border provinces was significantly higher at 17.3%, compared to 7.4% in Iran. This result aligns with the systematic review by Amini et al., which reported a lower overall HDV rate in Iran at 6.61% (16). However, it contrasts with another report that presented HDV rates of 3.9% in Iran (11) and 2.1% in Afghanistan (11).
The differences in seroprevalence rates across studies may be due to the regions examined or the inclusion of patients from facilities focused on severe HBV cases in this study. However, the discrepancy in seroprevalence rates between Iran and Afghanistan likely reflects Iran's effective HBV vaccination programs, which have reduced HDV seroprevalence compared to Afghanistan, where limited healthcare infrastructure and socio-political challenges hinder vaccination efforts.
Previous seroepidemiological studies in Iran have reported varying rates of HDV positivity among patients across different regions (17). The rates of HDV among HBsAg-positive patients in various provinces are as follows: Mazandaran (0%) (18), Kermanshah (1.7%) (19), Qom (2%) (20), Isfahan (2.9%) (21), Golestan (5.8%) (4), Tehran (7.7%) (22), Khuzestan (11.5%) (23), and Hamadan (17.3%) (24). Various surveys conducted on the three provinces bordering Iran confirm our results. In our study, we found the seroprevalence of HDV among HBsAg-positive patients to be 4.6% in Razavi Khorasan (Mashhad), 2.7% in South Khorasan (Birjand), and 13% in Sistan and Baluchestan (Zahedan). These results align closely with various surveys. For instance, Bakshipour et al. reported a 17% seroprevalence of HDV among HBsAg-positive patients in Sistan and Baluchestan (25). Similarly, Ghezeldasht et al. found a 5.8% seroprevalence of HDV among HBsAg-positive patients at the educational and research laboratory of the University of Mashhad (26), while Ziaee and Azarkar reported a 3.1% seroprevalence in Birjand (10). All of these findings are consistent with the results of our study.
Our findings show no significant association between gender and HDV positivity, consistent with studies by Tahaei et al. (22) and Sayad et al. (19). While some research has indicated a higher seroprevalence of HDV in men due to their engagement in high-risk behaviors (24, 25), this was also evident in our study. Most participants were male (57.14%), with an average age of 46 years, reflecting the broader demographic trend of HBV seroprevalence among middle-aged men; however, there was no statistical significance.
Similarly, marital status was not significantly associated with HDV positivity, a finding consistent with Ghezeldasht et al. (26). While most participants were married (85.2%), the lack of correlation suggests that marital status alone may not determine HDV risk. However, cultural practices and social factors could indirectly influence infection rates, particularly in settings where multi-partner relationships or polygamy are prevalent.
The study investigated various risk factors for HDV infection, such as a history of jaundice, cupping, tattooing, major surgery, and endoscopy. Among these, only a history of living or traveling abroad showed a significant association with HDV positivity (P < 0.001). This highlights the role of migration in the transmission of infectious diseases, as individuals exposed to regions with higher HDV endemicity are at greater risk (2). These findings suggest a need for targeted interventions, such as screening and vaccination, for populations with significant travel history.
Contrary to expectations, no significant associations were found between HDV positivity and injection drug use, alcohol consumption, trauma, or war-related activities. While injection drug use is a well-documented risk factor for HDV (7), the low number of participants reporting such behaviors in this study may have limited the ability to detect significant associations. Similarly, the low number of participants with histories of alcohol consumption (n = 4) or injecting drug use (n = 4) limits the generalizability of these findings. Future studies with larger samples and detailed behavioral data are needed to explore these relationships further.
The significant regional variation in HDV seroprevalence emphasizes the importance of local healthcare conditions and policies. The higher seroprevalence in Afghan provinces reflects the challenges faced by Afghanistan's healthcare system, including lower vaccination rates and limited access to clean medical equipment. By contrast, Iran's extensive vaccination efforts and improved healthcare infrastructure have likely contributed to lower HDV rates. The findings suggest that HDV infection is more common in border regions, where migration and healthcare access disparities exacerbate disease spread.
5.1. Limitations
This study has notable limitations. Convenience sampling may cause selection bias, as patients from larger healthcare centers are overrepresented. Self-reported data on risk factors like drug use and alcohol consumption might be underreported due to social stigma. Furthermore, the cross-sectional design limits the ability to establish causal relationships between risk factors and HDV infection. Future longitudinal studies are needed to clarify HDV transmission dynamics and evaluate intervention effectiveness.
5.2. Conclusions
This study reveals significant differences in HDV seroprevalence among HBsAg-positive patients in eastern Iran and western Afghanistan, with a particularly high seroprevalence in Afghan provinces. This highlights the need for improved screening and vaccination programs in these areas. While no demographic factors, such as gender or age, were significantly associated with HDV positivity, international travel was linked to increased transmission. Targeted public health interventions in high-risk border regions are crucial to reduce the burden of HDV and improve healthcare outcomes in these underserved populations.

.jpg)