1. Background
Hepatitis, primarily caused by Hepatitis B (HBV) and Hepatitis C (HCV) viruses, affects millions of people worldwide and represents a significant health burden (1). Persistent HBV and HCV infections can lead to serious liver conditions such as cirrhosis, liver failure, and hepatocellular carcinoma (HCC) (2). According to estimates from the World Health Organization (WHO), 71 million people globally have chronic HCV infection, while 296 million people are living with chronic HBV infection (3).
Iran, with a population of over 80 million, has implemented several programs aimed at reducing the incidence of viral hepatitis (4). These initiatives include nationwide HBV vaccination campaigns and harm reduction strategies to curb the spread of HCV among people who inject drugs (PWID) (5). Despite these efforts, viral hepatitis remains a public health issue in Iran, underscoring the importance of understanding regional epidemiology to develop effective prevention and control programs tailored to specific areas. Studies show that the prevalence and risk factors of HBV and HCV infection vary across different regions of Iran (6), highlighting the need for localized data to guide public health interventions.
With a population of over 4 million (7), Fars province in southern Iran provides a significant case study for examining regional hepatitis epidemiology. Although numerous investigations have explored the incidence of HBV and HCV in Iran (8), a comprehensive analysis based on data from a large, dedicated registry has been lacking. This study aims to address that gap by analyzing data from the Fars hepatitis registry to assess the prevalence, demographics, and risk factors associated with HBV and HCV infections.
2. Objectives
Our objective is to offer new insights into the current hepatitis epidemiology in southern Iran, with the ultimate goal of reducing the burden of hepatitis through informed, targeted interventions.
3. Methods
3.1. Methods
In this cross-sectional descriptive-analytical study, we included a total of 6,690 adult patients with enzyme immunoassay-confirmed HBV and HCV infections, with a minimum of six months having elapsed since their diagnosis, from the Fars hepatitis registry. Patients with other known hepatic diseases, malignancies, co-infections of HBV and HCV, acute hepatitis, or severe comorbid conditions (e.g., heart failure, chronic kidney disease) were excluded from the study. The study protocol was thoroughly evaluated and approved by the Ethics Committee of Shiraz University of Medical Sciences, with the code IR.SUMS.REC.1396.S440.
The Fars hepatitis registry is affiliated with Shiraz University of Medical Sciences, based at the Gastroenterohepatology Research Center within the Motahhari Referral Clinic in Shiraz, Iran. All eligible subjects were referred to the clinic by gastroenterologists. Data collection commenced in 1995 and continued until 2023, with the first patient included in the records having been diagnosed in 1991. Before the patients’ admission to this facility, the goals of the study were explained to them, and informed consent was obtained from each participant. Subsequently, data regarding the timing of diagnosis, demographic characteristics, medical history, disease progression (including symptoms at onset), laboratory results, history of exposure to potential transmission routes and risk factors, and family history of hepatitis infection were collected, and anthropometric measurements were taken. The enrolled patients were followed up every six months through telephone interviews and in-person visits conducted by gastroenterologists. The aim of this study was to evaluate the course of the disease and its associated outcomes, including cirrhosis, hepatocellular carcinoma, liver transplantation, and mortality.
3.2. Statistical Analysis
The descriptive analysis presented the available data as the (mean ± standard deviation) for numerical variables and as frequencies and percentages for categorical variables. The association between each pair of categorical variables was assessed using either the chi-square test or Fisher's exact test. The relationship between categorical and quantitative variables was examined using an independent sample t-test. Statistical analyses were performed using SPSS software, version 25 (SPSS Inc., Chicago, IL). A P-value of less than 0.05 was considered statistically significant.
4. Results
Our database includes records of 6,690 adult patients with hepatitis, comprising 3,840 (57.4%) HBV and 2,820 (42.6%) HCV patients. Among these patients, 78.5% were male, with a mean age of 52.56 years (SD: 13.24). According to Table 1, male sex was more prevalent in HCV patients compared to HBV patients (88.1% vs. 66.6%, P-value < 0.001). Additionally, significant differences were observed between HBV and HCV patients in terms of marital status, education level, and family history of HBV and HCV (P-value < 0.001 for all variables). Body Mass Index was significantly higher in HBV patients compared to HCV patients (P-value < 0.001).
| Basic Characteristics | Total | HBV | HCV | P-Value |
|---|---|---|---|---|
| Total | 6690 | 3840 (57.4) | 2850 (42.6) | |
| Gender | < 0.001 b, c | |||
| Male | 5068 (75.8) | 2556 (66.6) | 2512 (88.1) | |
| Female | 1622 (24.2) | 1284 (33.4) | 338 (11.9) | |
| Marital status | < 0.001 b, c | |||
| Single | 1448 (21.6) | 617 (16.1) | 831 (29.2) | |
| Married | 4979 (74.4) | 3132 (81.6) | 1847 (64.8) | |
| Separated/divorced | 170 (2.5) | 40 (1.0) | 130 (4.6) | |
| Widowed | 93 (1.4) | 51 (1.3) | 42 (1.5) | |
| Education | < 0.001 b, c | |||
| Illiterate | 885 (13.2) | 679 (19.5) | 206 (7.7) | |
| Elementary school | 2564 (38.3) | 1372 (39.5) | 1192 (44.8) | |
| High school | 853 (12.8) | 404 (11.6) | 449 (16.9) | |
| Diploma | 1337 (20.0) | 690 (19.9) | 647 (24.3) | |
| College | 497 (7.4) | 329 (9.5) | 168 (6.3) | |
| Family history of HBV | 1267 (18.9) | 1220 (31.8) | 47 (1.6) | < 0.001 b, c |
| Family history of HCV | 199 (3.0) | 37 (1.0) | 162 (5.7) | < 0.001 b, c |
| BMI (kg/m2) | 24.80 ± 4.49 | 25.32 ± 4.51 | 24.12 ± 4.38 | < 0.001 c, d |
| Age (y) | 52.56 ± 13.24 | 52.75 ± 14.28 | 52.31 ± 11.68 | 0.169 d |
Abbreviations: BMI, Body Mass Index; HBV, Hepatitis B virus; HCV, Hepatitis C virus; SD, standard deviation.
a Values are expressed as No. (%) or mean ± SD.
b Between-group differences were determined using chi-square test for qualitative.
c P < 0.05 was considered statistically significant.
d Between-group differences were determined using Independent sample t-test for qualitative data.
Table 2 also demonstrates significant differences in smoking status and drug usage between HBV and HCV patients (P-value <0.001).
| Basic characteristics | Total | HBV | HCV | P-Value d |
|---|---|---|---|---|
| Smoking | < 0.001 | |||
| No | 4483 (67.0) | 3252 (72.5) | 1231 (27.5) | |
| Current smoker | 1429 (21.4) | 307 (21.5) | 1122 (78.5) | |
| Ex-smoker | 778 (11.6) | 281 (36.1) | 497 (63.9) | |
| Water pipe | < 0.001 | |||
| No | 5806 (86.8) | 3418 (58.9) | 2388 (41.1) | |
| Current smoker | 382 (5.7) | 201 (52.6) | 181 (47.4) | |
| Ex-smoker | 502 (7.5) | 221 (44.0) | 281 (56.0) | |
| Chemical drugs | 54 (0.8) | 5 (0.1) | 49 (1.7) | < 0.001 |
| Traditional drugs | 99 (1.5) | 24 (0.6) | 75 (2.6) | < 0.001 |
Abbreviations: HBV, Hepatitis B virus; HCV, Hepatitis C virus.
a Values are expressed as No. (%).
b Between-group differences were determined using chi-square test.
c Chemical drugs included crack, crystal, methadone, and tamjizak, and traditional drugs included opium, burned opium, heroin, hashish, grass, marijuana, snus, and shire.
d P < 0.05 was considered statistically significant.
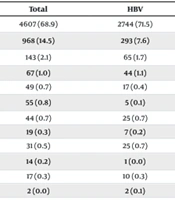
We identified dental procedures (68.9%), blood transfusion (14.5%), tattoos (2.1%), and war injuries (1.0%) as the most prevalent risk factors among the registered patients, respectively (Table 3).
| Risk Factors | Total | HBV | HCV | P-Value |
|---|---|---|---|---|
| Dental procedures | 4607 (68.9) | 2744 (71.5) | 1863 (65.4) | < 0.001 c |
| Blood transfusion | 968 (14.5) | 293 (7.6) | 675 (23.7) | < 0.001 c |
| Tattoo | 143 (2.1) | 65 (1.7) | 78 (2.7) | 0.004 c |
| War injuries | 67 (1.0) | 44 (1.1) | 23 (0.8) | 0.169 |
| Hemodialysis | 49 (0.7) | 17 (0.4) | 32 (1.1) | 0.001 |
| Intravenous drug injection | 55 (0.8) | 5 (0.1) | 50 (1.8) | < 0.001 c |
| Sharp trauma | 44 (0.7) | 25 (0.7) | 19 (0.7) | 0.938 |
| Prison | 19 (0.3) | 7 (0.2) | 12 (0.4) | 0.070 |
| Uncertain sexual contacts | 31 (0.5) | 25 (0.7) | 6 (0.2) | 0.009 |
| Major thalassemia | 14 (0.2) | 1 (0.0) | 13 (0.5) | < 0.001 c |
| Cupping | 17 (0.3) | 10 (0.3) | 7 (0.2) | 0.905 |
| Surgery | 2 (0.0) | 2 (0.1) | 0 (0.0) | 0.223 |
Abbreviations: HBV: Hepatitis B virus; HCV: Hepatitis C virus.
a Values are expressed as No. (%).
b Between-group differences were determined using chi-square test.
c P < 0.05 was considered statistically significant.
Upon comparing the frequency of potential risk factors between HBV and HCV patients, we observed that the prevalence of dental procedures (71.5% vs. 65.4%, P-value < 0.001) and uncertain sexual contacts (0.7% vs. 0.2%, P-value = 0.009) were significantly higher in HBV patients compared to those with HCV. Conversely, blood transfusion (23.7% vs. 7.6%, P-value < 0.001), tattoos (2.7% vs. 1.7%, P-value = 0.004), hemodialysis (1.1% vs. 0.4%, P-value = 0.001), intravenous drug injection (1.8% vs. 0.1%, P-value < 0.001), and major thalassemia (0.5% vs. 0.0%, P-value < 0.001) were more common in patients with HCV compared to those with HBV.
According to Table 4, patients with HCV exhibited significantly higher levels of aspartate transaminase (P-value < 0.001), alanine transaminase (P-value <0.001), alkaline phosphatase (P-value < 0.001), and total bilirubin (P-value = 0.002), but lower levels of albumin (P-value < 0.001) and prothrombin time (P-value = 0.034) compared to HBV patients.
| Variables | Total | HBV | HCV | P-Value |
|---|---|---|---|---|
| Hemoglobin (g/dL) | 14.62 ± 2.14 | 14.60 ± 1.94 | 14.65 ± 2.35 | 0.423 b |
| Protein (g/dL) | 7.60 ± 0.81 | 7.60 ± 0.77 | 7.60 ± 0.86 | 0.954 b |
| Albumin (g/dL) | 4.38 ± 0.59 | 4.44 ± 0.57 | 4.31 ± 0.60 | < 0.001 b, c |
| AST (IU/L) | 33.00 (23.00 - 57.00) | 27.00 (21.00 - 39.00) | 47.00 (30.00 - 79.00) | < 0.001 c, d |
| ALT (IU/L) | 40.00 (23.00 - 74.00) | 30.00 (20.00 - 53.00) | 58.00 (33.00 - 99.00) | < 0.001 c, d |
| ALP (IU/L) | 202.00 (156.00 - 260.75) | 194.00 (148.00 - 251.00) | 213.00 (167.00 - 273.00) | < 0.001 c, d |
| Total bilirubin (mg/dL) | 0.80 (0.60 - 1.20) | 0.80 (0.60 - 1.20) | 0.90 (0.60 - 1.26) | 0.002 c, d |
| BUN (mg/dL) | 13.00 (11.00 - 17.00) | 13.00 (11.00 - 17.00) | 13.00 (11.00 - 16.30) | 0.709 d |
| INR | 1.05 (1.00 - 1.20) | 1.05 (1.00 - 1.20) | 1.05 (1.00 - 1.20) | 0.589 d |
| PT | 13.28 ± 1.54 | 13.29 ± 1.51 | 13.26 ± 1.58 | 0.034 b, c |
| TSH (mIU/L) | 1.87 (1.08 - 2.80) | 1.79 (1.10 - 2.57) | 1.94 (1.06 - 3.00) | 0.104 d |
Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate transaminase; BUN, blood urea nitrogen; HBV, Hepatitis B virus; HCV, Hepatitis C virus; INR, international normalized ratio; IQR, interquartile rage; PT, prothrombin time; SD, standard deviation.
a Values are expressed as mean ± SD or median (IQR).
b Between-group differences were determined using independent sample t-test.
c P < 0.05 was considered statistically significant.
d Between-group differences were determined using Mann-Whitney U test.
A comparison of the outcomes among registered patients revealed 452 (6.8%) cases of cirrhosis, 4 (0.1%) cases of liver transplantation, 1 (0.0%) case of hepatocellular carcinoma, and 20 (0.3%) deaths. The majority of patients with cirrhosis were male (87.4% vs. 15.3%, P-value < 0.001), while no significant differences were observed between males and females for other outcomes (P-value > 0.999 for liver transplantation and hepatocellular carcinoma, and P-value = 0.798 for death, see Table 5). Cirrhosis was significantly more prevalent among HCV patients (66.2% vs. 33.8%, P-value < 0.001).
Abbreviations: HBV, Hepatitis B virus; HCV, Hepatitis C virus.
a Values are expressed as No. (%).
b Between-group differences were determined using Chi-square
c P < 0.05 was considered statistically significant.
d Between-group differences were determined using Fisher Exact tests.
5. Discussion
The study provides important insights into the epidemiology of hepatitis, specifically analyzing the prevalence, risk factors, clinical features, and outcomes among adult patients in southern Iran. The findings reveal notable differences between HBV and HCV, highlighting the need for tailored prevention and treatment strategies. Our research identified a higher proportion of HCV patients being male compared to HBV patients, suggesting the need for further investigation into potential sex-specific risk factors or healthcare-seeking behaviors (9). The literature presents conflicting evidence regarding sex differences in hepatitis prevalence. While some studies suggest that HCV is more prevalent and progresses more rapidly in men, potentially linked to higher rates of intravenous drug use, others have reported contradictory findings (10, 11).
The mean age of patients in our study was 52.56 years, indicating that hepatitis infections disproportionately affect older individuals in this region (12). This underscores the importance of targeted screening and immunization efforts in older age groups to mitigate the impact of viral hepatitis-related complications (13).
5.1. Risk Factors
Our analysis identified various risk factors associated with hepatitis transmission, including dental procedures, blood transfusion, tattooing, and war injuries. Notably, dental procedures emerged as the most prevalent risk factor among registered patients, emphasizing the importance of infection control measures in dental settings to prevent disease transmission (14). Additionally, significant disparities were reported between HBV and HCV patients in terms of the incidence of specific risk factors. In line with our findings, a substantial correlation was observed between dental procedures and sexual risk behaviors with HBV in Morocco (15). Another study found that multiple heterosexual partnerships, longer periods of imprisonment, body tattoos, and the sharing of sharp objects in prison were risk factors associated with HBV. Moreover, the presence of body tattoos, a prior history of surgery, and imprisonment were linked to HCV infection (16). Hepatitis B virus patients exhibited a higher prevalence of dental procedures, while HCV patients were more commonly associated with blood transfusions, tattooing, and intravenous drug injection (17). These findings underscore the diverse transmission routes for HBV and HCV and highlight the importance of targeted prevention efforts tailored to specific risk profiles (3).
5.2. Clinical Characteristics and Outcomes
In terms of clinical parameters, HCV patients exhibited significantly higher levels of liver enzymes compared to HBV patients (18). This finding reflects the distinct pathophysiological mechanisms underlying HBV and HCV infections, with HCV often resulting in more severe liver damage and elevated hepatic biomarkers (19). Additionally, our study revealed a higher prevalence of cirrhosis among HCV patients compared to HBV patients, highlighting the chronic and progressive nature of HCV infection (20). Given the significant burden of cirrhosis on healthcare resources and patient outcomes, enhancing HCV screening, early diagnosis, and access to antiviral therapy is critical for reducing cirrhosis-related complications and mortality (21).
5.3. Limitations and Future Directions
It is important to acknowledge several limitations in our study. First, the study design may introduce biases related to data collection and patient selection. Additionally, the reliance on electronic health records could have led to incomplete or inaccurate documentation of certain variables. Future studies using prospective methodologies and more comprehensive data collection protocols are needed to validate our findings and further clarify the underlying mechanisms of hepatitis transmission and disease progression in this population.
5.4. Conclusions
Our study provides a comprehensive analysis of the epidemiology of hepatitis in southern Iran, highlighting significant differences in demographic, clinical, and risk factor characteristics between HBV and HCV infections. These findings have important implications for public health initiatives, including targeted screening, vaccination, and harm reduction strategies, aimed at reducing the burden of viral hepatitis and its associated complications in this region.