1. Background
The World Health Organization (WHO) defines complementary alternative medicine (CAM) as a broad set of health care practices that are not part of a country's own tradition or conventional medicine and are not fully integrated into the dominant health care system. The CAM has long been used, especially in the Far East, to treat viral hepatitis and various other diseases. Although many different products are used as CAM, herbal treatments are predominant. Vitamins and diet therapies are other commonly preferred preparations in CAM. This has led to a number of discussions between conventional medicine and alternative medicine. Western medicine in particular, which supports classical medicine, has distanced itself from CAM because of the lack of standardized production, the paucity of pharmacokinetic data, the small number of well-designed randomized, controlled trials of these products, and the evidence that some medicinal herbs have been obtained (1-4).
In a study conducted in the pediatric population, it was reported that CAM therapies were preferred by parents in patients with chronic hepatitis B (HBV) and hepatitis C (HCV). Herbal drugs and dietary supplements were the most common. In this age group, the most common reason for parents to use CAM was insufficient doctor's information (4). Another important issue is to clarify the benefit-harm status of alternative medicine. Studies on this subject are increasing day by day. In particular, the comparison of chronic hepatitis patients receiving antiviral therapy with the group of patients receiving CAM will provide concrete evidence for CAM therapy (5-7).
However, the situation is slightly different on the African continent. Unconscious CAM use is widespread due to the geographical conditions of the region and some difficulties brought about by the sociodemographic structure. Due to inadequate health infrastructure and financial constraints, accessing conventional medical care is not always possible. Therefore, various CAM therapies are preferred by chronic hepatitis patients. Studies in Africa are increasing in this area (8-10).
As Black Muslim immigrants, Somalis suffer 'triple jeopardy' of being ostracized based on religion, immigration status, and race. These factors contribute to various healthcare disparities like gender preferences in seeking and accepting care, modesty requirements, resettlement stresses, insufficient interpreter services, traditional beliefs, and limited health literacy. Most cultural practices are based on Islamic traditions (11).
2. Objectives
This study aimed to examine the CAM utilization status of patients admitted to the infection polyclinic of a training and research hospital in Somali-Mogadishu with chronic HBV, HCV, or both.
3. Methods
3.1. Study Design
This prospective, cross-sectional survey study was conducted in Somalia between January 1 and May 30, 2023. Individuals aged over 18 years with a history of chronic HBV, HCV, or both were included in the study.
3.2. Sample Selection
The formula used in similar survey studies was employed to determine the sample size (4). The minimum sample size was calculated as 300, with a 5% margin of error, a 95% confidence interval, and a 50% distribution of responses. The following formula was used to calculate the sample size (Equations 1 - 3): (4).
Where; n is the sample size, E is margin of error, N is the population size, r is the fraction of responses, and Z(c/100) is the critical value for the confidence level c.
3.3. Questionnaire
The questionnaire was prepared in Word format and administered to the participants during the polyclinic examination. Questions, adapted from similar publications, were designed specifically for this study. All participants were included in the survey voluntarily, and they were not asked for their names or identity information. The questionnaire was filled out in such a way that it was not clear which participant the responses belonged to.
The questionnaire consisted of two parts. In the first part, nine questions were prepared about sociodemographic characteristics (age, gender, educational status, marital status, number of spouses, region of residence, race). In the second part, nine questions were prepared about background (hepatitis type, duration of diagnosis, treatment status, etc.) and CAM. The questionnaire was developed and validated by referring to similar studies (12-14). The frequency of CAM usage among the cases included in the study was also assessed.
The methods used in CAM treatment are preferred by patients at various frequencies. For example, burning is preferred once, while honey is mixed in tea or water and taken every day. The consumption of camel milk varies based on availability. Somali people rarely prefer acupuncture to treat hepatitis. They use herbal remedies, such as chewing the Treem tree, chopping it up, mixing it with water, and then drinking it. In Somalia, rural people use camel urine as a drink to treat hepatitis because it is part of their culture and they believe it is therapeutic. Sheep meat and cupping, like acupuncture, are not widely used as alternative treatments for hepatitis in Somalia. Some people from southern Somalia use complementary and alternative medicine for hepatitis. Prayer is a common practice in Somalia as a treatment for any disease.
Side effects of CAM were common in Somalia. Burn scars on the skin of the abdomen and peripheral extremities are a common side effect in burn users. Those who used camel urine experienced gastrointestinal disturbances such as vomiting and nausea. No common side effects were reported with other types of CAM.
3.4. Statistical Analysis
SPSS version 23.0 (IBM, New York, USA) was used for the analysis of the study. The Kolmogorov-Smirnov test and histogram were used for normality analysis of the data. Frequencies and percentages were calculated for categorical variables, while means (standard deviation) and medians (interquartile range [IQR]) were calculated for continuous variables. Pearson's chi-square test, Fisher's exact test, and the adjusted Bonferroni method were used to compare categorical data. A P-value of less than 0.05 was considered statistically significant.
4. Results
4.1. Sociodemographic
A total of 300 patients were included in the study, with 51.3% of the cases being male. The majority (56%) were in the age range of 40 to 54 years. Forty-eight percent of the patients were illiterate, and the majority (71%) were married. When the monthly income status of the cases was questioned, 70% of them had an income of less than $500. About half of the participants resided in the city center. Four non-Somali cases were also included in the study. When the marital status of the participants was questioned, the majority were single-married (Table 1).
| Questions and Responses | No. (%) |
|---|---|
| Gender | |
| Male | 154 (51.3) |
| Female | 146 (48.7) |
| Age group | |
| 18 - 24 | 30 (10) |
| 25 - 39 | 100 (33.3) |
| 40 - 54 | 168 (56) |
| ≥ 55 | 2 (0.7) |
| Educational status | |
| Illiterate | 144 (48.0) |
| Primary | 49 (16.3) |
| Secondary | 50 (16.7) |
| University | 57 (19.0) |
| Marriage | |
| Married | 213 (71) |
| Single | 45 (15) |
| Divorced | 24 (8) |
| Widowed | 18 (6) |
| Income status ($) | |
| < 500 | 211 (70.3) |
| 500 - 1000 | 79 (26.3) |
| > 1000 | 10 (3.3) |
| Area of residence | |
| Rural | 151 (50.3) |
| Urban | 149 (49.6) |
| Ethnicity | |
| Somalia | 296 (98.7) |
| Non-Somalia | 4 (1.3) |
| Number of wives | |
| None | 143 (47.6) |
| One | 117 (39) |
| Two | 33 (11) |
| Three | 6 (2) |
| Four | 1 (0.4) |
Sociodemographic Parameters
4.2. Personal Background and Complementary Alternative Medicine
When the history of the cases was questioned, 85% had chronic HBV. The majority (45%) had a diagnosis and follow-up period of less than 5 years. Eighty-seven percent of the cases declared that they did not receive any antiviral treatment. When regular polyclinic check-ups were questioned, 44% did not pay any attention. The majority of cases (77.9%) reported using CAM. Complementary therapy was generally recommended by families (60.7%). When the benefit of the treatment was questioned, only 56% of CAM users believed in the benefit of the treatment. Of those who used the treatment, 21% reported experiencing side effects from the treatment (Table 2).
| Questions and Responses | No. (%) |
|---|---|
| Hepatitis type (N = 300) | |
| HBV | 255 (85.0) |
| HCV | 43 (14.3) |
| HBV + HCV | 2 (0.7) |
| Diagnosis period (N = 300) | |
| Newly diagnosed | 79 (26.3) |
| < 5 years | 135 (45.0) |
| 6 - 10 years | 41 (13.7) |
| > 10 years | 45 (15.0) |
| Antiviral therapy period (N = 300) | |
| Never taken | 261 (87.0) |
| Yes | 29 (9.7) |
| Yes but I stopped the treatment | 10 (3.3) |
| Regular polyclinic control (N = 300) | |
| Yes | 168 (56.0) |
| No | 132 (44.0) |
| CAM (N = 300) | |
| Yes | 234 (77.9) |
| No | 66 (22.1) |
| CAM recommendation (N = 234) | |
| Family/friends | 142 (60.7) |
| TV, radio, or internet | 3 (1.3) |
| Health worker | 55 (23.5) |
| Religious official | 27 (11.5) |
| Others | 7 (3.0) |
| Belief in CAM treatment (N = 234) | |
| Yes | 131 (56) |
| No | 20 (8.6) |
| I'm not sure | 83 (35.4) |
| Side-effects of CAM (N = 234) | |
| Yes | 49 (21.0) |
| No | 106 (45.1) |
| I'm not sure | 79 (33.9) |
Chronic Hepatitis and Complementary Alternative Medicine Usage
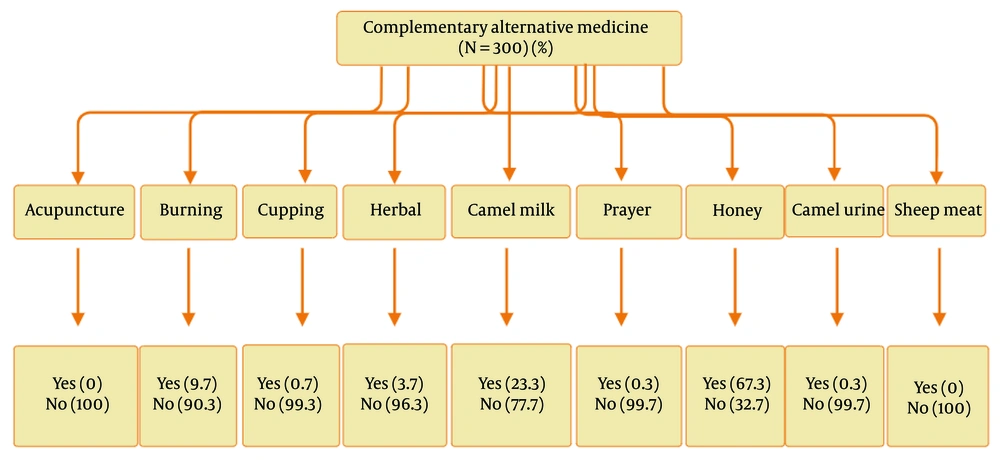
4.3. Types of Complementary Alternative Medicine
When asked about the nine different treatment methods used by the cases for CAM, it was found that honey was the most common, followed by camel's milk. Burning the body by cauterizing it at specific locations was identified as another common method. Drinking camel urine is another method believed to be curative in Somali cases of chronic hepatitis. In addition, sheep meat, acupuncture, prayer, and herbal therapy are among the preferred methods. However, none of our cases reported the use of sheep meat or acupuncture. Although prayer is a common method due to regional religious beliefs and culture, the rate of positive responses was quite low (Figure 1).
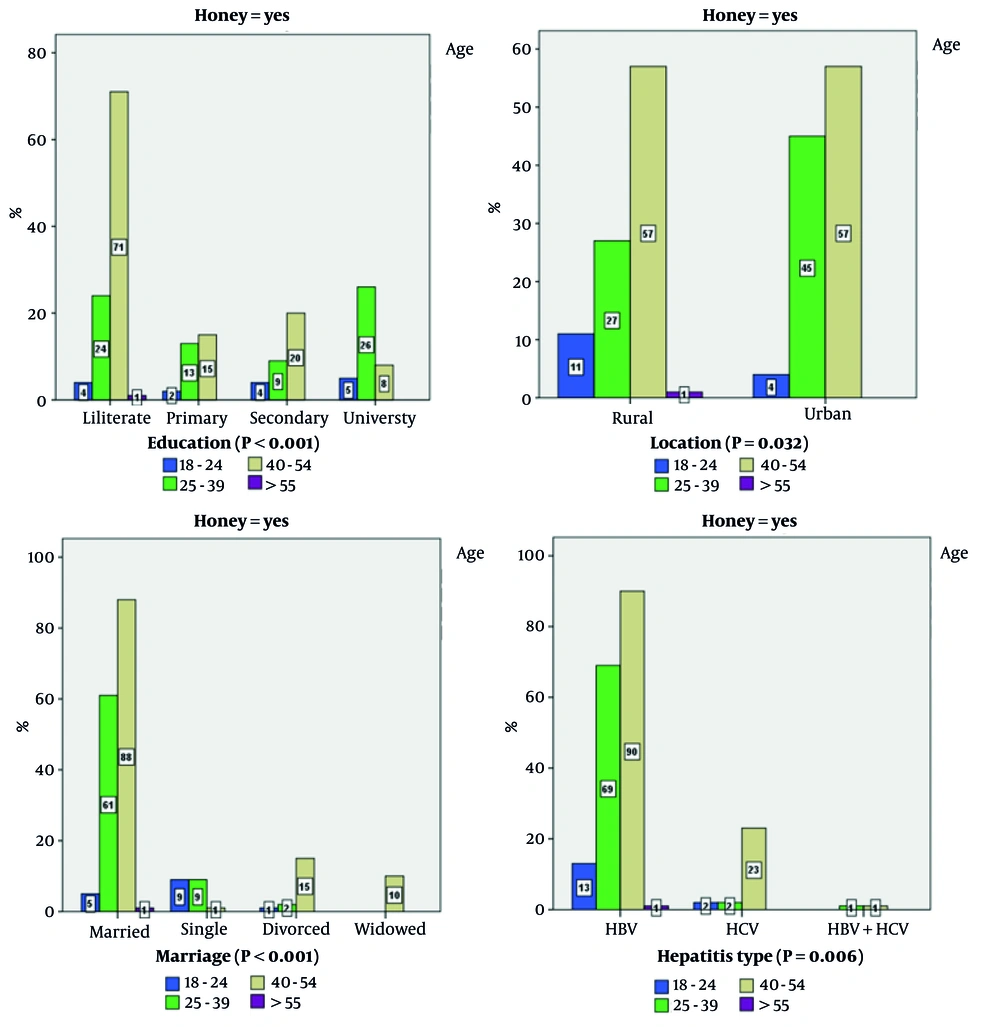
4.4. Honey Usage and Socio-Demography
Cases using honey in CAM treatment were analyzed in terms of sociodemographic structure according to age groups (Figure 2). It was found that the education level of cases between the ages of 40 and 54 who used honey was predominantly illiterate (P < 0.001). When the region of residence of the honey-using cases was evaluated according to age groups, it was found that the 25 to 54 age group mostly lived in urban areas (P = 0.032). Interestingly, it was shown that the cases who preferred honey in the alternative treatment of hepatitis were generally married individuals in the young age group (P < 0.001). Chronic HBV cases in the older age group were found to prefer honey more than HCV cases (P = 0.006).
When the cases using honey were analyzed according to occupational groups, it was found that housewives in the older age group (40 to 54 years) used honey more frequently (P = 0.001). When the use of honey was evaluated according to gender, it was found that both females and males with illiterate education levels used honey more frequently (P = 0.004). Similarly, married females and males were found to use honey more frequently (P = 0.030).
4.5. Honey Usage and Associated Factors
Hepatitis patients most commonly use honey as a form of CAM. The rate of those who believe that drinking honey is beneficial for hepatitis treatment is quite high. When regular follow-up visits to the polyclinic with chronic hepatitis treatment were analyzed, it was shown that honey use decreased after the first five years of the disease diagnosis (P < 0.001). The rate of honey use in those who never received antiviral treatment was significantly higher than in those who received treatment (P = 0.039). There was a significant correlation between honey use and regular follow-up visits to the polyclinic (P < 0.001). It was determined that family or friends most frequently recommended honey use in the treatment of chronic hepatitis (P = 0.001). Interestingly, the majority of the users believed that they benefited from honey treatment (P = 0.039). The rate of those who reported harm from honey treatment was very low (P = 0.021) (Table 3).
| Parameters | Honey (N = 300) | P-Value | |
|---|---|---|---|
| Used | Not Used | ||
| Follow-up period (y) | < 0.001 | ||
| New diagnose | 7.3 | 19 | |
| < 5 | 35.3 | 9.6 | |
| 6 - 10 | 11.6 | 2 | |
| > 10 | 13 | 2 | |
| Antiviral therapy | 0.039 | ||
| Never | 56.3 | 30.6 | |
| Yes | 8.3 | 1.3 | |
| Yes, but stop | 2.6 | 0.6 | |
| Policlinic control | < 0.001 | ||
| Regular | 44.6 | 11.3 | |
| No | 22.6 | 21.3 | |
| CAM recommendation | 0.001 | ||
| Family/friends | 40 | 7.3 | |
| TV/radio/internet | 0.3 | 0.6 | |
| HCWs | 18 | 0.3 | |
| Religious official | 7.3 | 1.6 | |
| Others | 1.6 | 0.6 | |
| Benefit of CAM | 0.039 | ||
| Yes | 39.6 | 4 | |
| No | 5.3 | 1.3 | |
| Not sure | 22 | 5.6 | |
| Side effect of CAM | 0.021 | ||
| Yes | 14.3 | 2 | |
| No | 32.3 | 3 | |
| Not sure | 20.3 | 6 | |
Honey Usage and Associated Factors in Cases
4.6. Camel Milk
The relationship between camel's milk, which is the second most frequently used treatment for chronic hepatitis, and sociodemographic data according to age groups was analyzed. Patients aged 40 to 54 years were generally illiterate (P < 0.001). In addition, the same age group was generally married (P < 0.001). When investigated according to gender, it was found that housewives (P < 0.001), married individuals (P = 0.006), and those with one wife (P = 0.034) preferred camel's milk more.
4.7. Burning
Burning, the third most preferred CAM method, was more common in those not receiving antiviral treatment (P = 0.042), in housewives aged 40 to 54 years (P = 0.048), and in both genders who were married (P = 0.001). Interestingly, the proportion of individuals reporting they benefited from burning was also higher (P = 0.045).
5. Discussion
This is the first study to examine CAM methods used by chronic hepatitis cases in Somalia, a sub-Saharan African country. The CAM is commonly used in Africa. In a study conducted in South Africa, this rate was found to be between 6% and 38% (14). The CAM (4.7%) was also cited as a reason why Egyptian chronic hepatitis C patients rejected antiviral therapy (15). A study in Uganda showed that 23% of hepatitis cases used herbal medicine. It was found that HCV patients believed that the simultaneous use of herbal and traditional treatments was more beneficial than for HBV patients. Additionally, CAM usage was higher in those who were followed for more than a year, unlike those who were newly diagnosed. It was shown that local, herbal treatments believed to be healing were generally used (10).
Complementary alternative medicine use is not only common in Africa but also globally. In a study conducted in the United States, this rate was reported to be 42% (16). In India, 68% of patients with cirrhosis were shown to use CAM (17). In studies conducted in Asian countries, the rates were 17.1% in Japan, 18.6% in China, 71% in Singapore, and 72.7% in Korea (18). Recent studies have shown similar rates and various CAM types (16, 19, 20).
In Mogadishu, it was observed that patients frequently used honey, camel milk, and burning. Although only one case was reported in our study, drinking camel urine is one of the other methods used. An interesting aspect of CAM therapy is that 103 (34%) patients do not believe in or are not sure of its benefits despite using CAM therapy. However, those who used burning or honey reported a high rate of benefit from the treatment. No scientific studies show that these treatments are actually beneficial in cases of hepatitis. However, they may have had a placebo-like effect on patients.
Another interesting finding in the study is that patients who attend regular outpatient clinic controls prefer CAM treatment more. However, the rate is not high in patients who do not need antiviral treatment. The rate of CAM usage was found to be high, especially in the first five years of diagnosis. Cultural and social pressures and financial limitations may force patients to use such treatments rather than modern medicine. Additionally, the lack of information and guidance provided by healthcare professionals about such treatments may also contribute to this situation.
Herbal products are generally preferred in the treatment of hepatitis. Some studies prove the usefulness of botanical medicines with molecular methods. However, it is very important to prepare the product to be used for treatment with scientific methods and under appropriate conditions. Some studies have identified different toxic mixtures in herbal products. These include arsenic (40%), lead (60%), mercury (60%), and a range of other plant-derived hepatotoxic compounds, toxic industrial solvents, and alcohol. These substances can significantly increase patient mortality and morbidity. Recently, the US FDA and the Australian Department of Health have issued multiple warnings on contaminated and adulterated Ayurvedic products containing ingredients such as Azadirachta indica (Neem), Acorus calamus (Vacha or sweet flag), and various heavy metals that pose a threat to health and life (21-27).
Hepatitis patients who use herbal treatments in Mogadishu often prepare and use these treatments in non-laboratory settings and with unscientific techniques. As found in our study, some side effects are unavoidable. Physical examination of the patients who underwent burning treatment as CAM revealed burn scars on different parts of their bodies. A significant rate of side effects was also reported in patients using honey.
Sociodemographic characteristics are another important factor affecting CAM preference (28, 29). A study conducted in Norway with 42,277 participants found that females were more likely to seek CAM treatment. In both genders, it was observed that the middle age group used CAM more frequently. Smoking was reported to be a factor reducing CAM usage (30). In another study conducted in Turkey, it was observed that females with higher education levels resorted to herbal treatment more frequently (31). Similarly, in our study, sociodemographic structure was found to have a significant effect on CAM use. It was noted that being uneducated, married, female, a housewife, and the region where the patients lived significantly increased the use of CAM. Especially in HBV cases, honey usage was higher. In addition, the older age of the patients was one of the most important factors increasing the rate of CAM usage.
Of course, the study has some limitations. First, since the study was planned as an epidemiologic baseline study, it is not possible to compare antiviral treatment with CAM. Secondly, since a face-to-face survey method was used, it cannot be known whether the participants were completely objective in answering the questions. Third, patients' laboratory values (such as HBV DNA PCR) were not included in the study because they were incomplete. Fourth, the type of treatment, dose, frequency, method of usage, and type of side effects were recorded based on patient declaration. Field practices were not conducted. Finally, no internationally validated scale was used.
5.1. Conclusions
Patients with chronic hepatitis in Mogadishu frequently resort to various CAM methods. Honey, camel milk, and burning are the most commonly used methods. Factors such as marital status, education level, number of wives, early years of the disease, regular polyclinic control, lack of antiviral treatment, belief in CAM, and recommendations from friends and family affect CAM preference. Although the rate of those reporting side effects related to CAM is not low, the rate of those who think they benefit from the treatment is quite high. Comparative studies with laboratory and molecular values are needed to distinguish whether this benefit is antiviral-like or placebo-like. In this study, the aim was to examine the epidemiologic status of CAM in chronic hepatitis cases in Somalia. Field practices should be planned to determine the exact benefits and side effects of CAM in the people of the region. Studies should be conducted in rural areas, and practices should be monitored in the field. If possible, close laboratory control should be performed.