1. Background
Non-alcoholic fatty liver disease (NAFLD) is characterized by the accumulation of fat in the liver, exceeding 5 - 10% of its weight, without significant alcohol intake or other chronic liver conditions, involving the buildup of fat that exceeds 5 - 10% (1, 2). This condition is marked by the presence of steatosis, which can lead to serious complications such as cirrhosis, portal hypertension, and hepatocellular carcinoma (2, 3). The NAFLD is a common and serious condition that ranges from simple fat accumulation to advanced liver damage, including cirrhosis (4). It is closely associated with metabolic syndrome, particularly in individuals who are obese and exhibit high blood pressure, insulin resistance, and dyslipidemia (3). Additional risk factors for developing NAFLD include race, type of obesity, physical inactivity, and consumption of high-fat diets (2, 5). Although NAFLD progresses slowly, it has become the third leading cause of liver transplantation in the United States (6). The rising prevalence of NAFLD, driven by lifestyle changes and unhealthy dietary habits, poses a significant public health threat and challenges healthcare systems worldwide (5, 7).
Gallstones (GS) form when there is a disruption in the processing of cholesterol, bilirubin, calcium salts, specific proteins, and bile acids within the gallbladder and bile ducts. Two main types of GS are classified by their chemical composition: Cholesterol stones and pigment stones. Cholesterol GS are the most common type found in developed countries (8, 9). Gallstone disease (GSD), also known as cholelithiasis, is more prevalent among older adults, females, and individuals who are obese or have metabolic syndrome, hypertriglyceridemia, diabetes, and insulin resistance (10, 11). These risk factors contribute to the formation of GS, making it a significant health concern. Although GSD has a low mortality rate of 0.6%, it is one of the leading causes of hospitalization due to gastrointestinal complications (11). The financial burden associated with GSD has increased by over 20% since the 1980s, highlighting its substantial impact on healthcare systems. Therefore, effective management and prevention strategies for GSD are necessary to mitigate its implications on public health and healthcare resources (10, 12).
Gallbladder stones can lead to symptoms when they migrate to the cystic duct or the common bile duct (CBD), resulting in blockage or inflammation (13). A significant indicator of gallbladder disease is biliary colic, characterized by persistent and often intense pain. When a stone obstructs the cystic duct or CBD, it increases pressure within the gallbladder, leading to swelling that cannot be alleviated by the organ’s repeated contractions (12, 13). This pressure results in visceral pain, typically experienced as a constant sensation of fullness in the upper middle abdomen and upper right quadrant, often radiating to the area between the shoulder blades or the right shoulder. Biliary pain may be triggered by consuming fatty meals, large meals following fasting, or regular food intake (13, 14). It frequently manifests at night, several hours after going to bed. Biliary colic typically presents suddenly, lasts between 30 minutes and 5 hours, and gradually or rapidly subsides (10, 15).
The relationship between GSD and NAFLD is intricate and bidirectional. Research indicates that individuals with NAFLD are at a heightened risk of developing GSD, while those with GSD may also be predisposed to NAFLD. Both conditions share common risk factors, including obesity, age, diabetes, dyslipidemia, and hypertension (9, 11). It remains unclear whether NAFLD precedes GSD or if the presence of GSD signifies long-standing features of metabolic syndrome that accelerate the progression of NAFLD. Although multiple studies have suggested a potential association between NAFLD and GSD, this conclusion remains a subject of ongoing debate (12, 16).
Cholecystitis arises when a stone obstructs the cystic duct. Several factors increase the risk of developing this condition, including age, female gender, obesity or rapid weight loss, certain medications, and pregnancy. Research indicates chronic cholecystitis is more prevalent than acute cholecystitis and exhibits differences between genders (11, 12).
2. Objectives
The incidence of NAFLD and symptomatic GS is increasing, influenced by similar risk factors such as lifestyle choices, dietary habits, genetic predispositions, hormonal factors, and environmental influences (3, 13). Consequently, the present study aimed to evaluate the prevalence of NAFLD in patients with symptomatic GS undergoing cholecystectomy.
3. Methods
This cross-sectional study included 330 patients who underwent cholecystectomy at the Referral Hospital of Ganjavian in Dezful city, Iran, between 2020 and 2022. Patients were selected using a simple random sampling method. Inclusion criteria entailed patients aged 18 - 85 with symptomatic GS. Exclusion criteria comprised liver diseases such as viral and non-viral hepatitis, autoimmune hepatitis, alcoholic fatty liver based on the patient’s history, liver cancer, and cholecystectomy due to other causes such as gallbladder cancer. The study assessed the medical records of patients diagnosed with symptomatic GS who had undergone cholecystectomy, including both open and laparoscopic surgery. Data on age, gender, NAFLD (assessed using ultrasonography), alanine aminotransferase (ALT), aspartate aminotransferase (AST), serum glutamic oxaloacetic transaminase (SGOT), serum glutamate pyruvate transaminase (SGPT), and comorbidities (diabetes, hypertension, hyperlipidemia), as well as smoking status, were collected. The NAFLD was classified based on the ultrasonography report as non-infected, afflicted mild (grade 1), moderate (grade 2), and severe (grade 3) for cholecystectomy patients. Data analysis was conducted using SPSS version 22. Descriptive statistical analysis was used for quantitative variables, while percentage and frequency distribution tables were used for qualitative variables. Baseline characteristics were compared using chi-square tests for categorical variables and t-tests for continuous variables. The statistical significance level for this study was set at 0.05.
4. Results
Among the 330 symptomatic gallstone patients who underwent cholecystectomy, the mean age was 46.80 ± 14.51 years. Of the total, 77 patients (23.33%) were male with an average age of 48.79 ± 13.86 years, while 253 patients (76.67%) were female with an average age of 44.81 ± 14.54 years. Approximately 31.82% (n = 105) of all patients were diagnosed with NAFLD. The average age of patients with NAFLD was 48.64 ± 13.48 years.
Table 1 shows that 225 patients (68.18%) displayed no indicators of NAFLD, 61 patients (18.48%) were diagnosed with grade 1 NAFLD, and 44 patients (13.33%) were found to have grade 2 NAFLD. None of the patients were found to have grade 3 NAFLD. Among the 105 patients with NAFLD, 58.10% (n = 61) were found to have grade 1, while 41.90% (n = 44) were diagnosed with grade 2 NAFLD.
| Grades | No. (%) | Age (y) | Sex | Severity | |||
|---|---|---|---|---|---|---|---|
| Male | Female | ||||||
| No NAFLD | 225 (68.18) | 44.96 ± 14.84 | 56 (72.73) | 46.04 ± 14.01 | 169 (66.80) | 43.89 ± 13.49 | - |
| Grade 1 | 61 (18.48) | 49.84 ± 12.74 | 5 (6.49) | 51.34 ± 9.12 | 56 (22.13) | 48.35 ± 14.27 | Mild |
| Grade 2 | 44 (13.33) | 48.12 ± 12.59 | 16 (20.78) | 47.43 ± 10.70 | 28 (11.07) | 48.81 ± 12.03 | Moderate |
| Grade 3 | - | - | - | - | - | - | Severe |
Distribution of Patients According to NFALD Grading, Gender, and Mean Age a
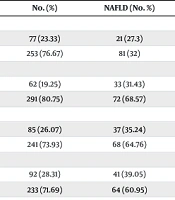
The results presented in Table 2 indicate that there is no significant association between sex and smoking status with NAFLD, as evidenced by odds ratios (OR) of 0.79 (95% CI: 0.42 - 1.44) and 1.42 (95% CI: 0.77 - 2.61), respectively. However, a statistically significant association was observed between NAFLD and diabetes (OR = 2.97, 95% CI: 1.61 - 5.45), dyslipidemia (OR = 1.96, 95% CI: 1.13 - 4.37), and hypertension (OR = 2.12, 95% CI: 1.24 - 3.61). The distribution of age, triglyceride (TG), cholesterol, SGOT, and SGPT variables based on NAFLD and non-NAFLD is illustrated in Table 3.
| Variables and Categories | No. (%) | NAFLD (No. %) | Non-NAFLD (No. %) | P-Value | OR | CI 95% |
|---|---|---|---|---|---|---|
| Sex | 0.43 | 0.79 | 0.42 - 1.44 | |||
| Male | 77 (23.33) | 21 (27.3) | 56 (72.7) | |||
| Female | 253 (76.67) | 81 (32) | 172 (68) | |||
| Diabetes | 0.01 | 2.97 | 1.61 - 5.45 | |||
| Yes | 62 (19.25) | 33 (31.43) | 29 (13.36) | |||
| No | 291 (80.75) | 72 (68.57) | 260 (86.64) | |||
| Dyslipidemia | 0.02 | 1.96 | 1.13 - 3.37 | |||
| Yes | 85 (26.07) | 37 (35.24) | 48 (21.72) | |||
| No | 241 (73.93) | 68 (64.76) | 173 (78.28) | |||
| Hypertension | 0.01 | 2.12 | 1.24 - 3.61 | |||
| Yes | 92 (28.31) | 41 (39.05) | 51 (23.18) | |||
| No | 233 (71.69) | 64 (60.95) | 169 (76.82) | |||
| Smoking status | 0.21 | 1.42 | 0.77 - 2.61 | |||
| Yes | 60 (19.05) | 28 (22.40) | 32 (16.84) | |||
| No | 255 (80.95) | 97 (77.60) | 158 (83.16) |
Characterizing Certain Correlated Factors in Gallstone Patients Undergoing Cholecystectomy
| Factors | NAFLD | Non-NAFLD | t | P-Value |
|---|---|---|---|---|
| Age (y) | 48.64 ± 13.48 | 44.96 ± 14.84 | 1.98 | 0.03 |
| TG (mg/dL) | 178.54 ± 55.34 | 161.58 ± 32.14 | 4.12 | 0.01 |
| Cholesterol (mg/dL) | 198.36 ± 35.41 | 172.61 ± 34.74 | 5.19 | 0.01 |
| SGOT (IU/L) | 28.93 ± 11.41 | 20.56 ± 6.68 | 2.37 | 0.02 |
| SGPT (IU/L) | 29.15 ± 13.23 | 20.75 ± 7.48 | 1.84 | 0.04 |
The Association Between Quantitative Variables of Patients with Non-alcoholic Fatty Liver Disease Status a
The findings shown in Table 3 reveal a significant association between NAFLD and several key factors among cholecystectomy patients. Notably, there was a discernible association between NAFLD and age (P = 0.03), TG levels (P = 0.01), cholesterol levels (P = 0.01), SGOT levels (P = 0.02), and SGPT levels (P = 0.04). These results indicated that, on average, the levels of these factors were higher in patients with NAFLD than in those without NAFLD.
5. Discussion
The present study found that the prevalence of NAFLD among symptomatic gallstone patients undergoing cholecystectomy was 31.82% (n = 105), indicating a significant occurrence of NAFLD in this patient population. The prevalence of NAFLD in patients with GS has been examined in various studies across different countries. For instance, a survey by Ramos-De la Medina et al. in Mexico reported a prevalence of 55% (17). In the United States, a 2013 study by Latenstein et al. found the prevalence to be 20% (18). In China, Qiao et al. reported a prevalence of 58.98% in 2017 (7), while a study by Ahmad et al. in Pakistan the same year indicated a prevalence of 55.62% (19). Additionally, a survey by Hajong et al. in India in 2018 found a prevalence of 31% (20). These findings reveal significant variation in the prevalence of NAFLD among patients with GS across different regions. Despite these differences, the results of these studies align with each other and with the present study’s findings.
Several mechanisms have been proposed to explain the relationship between NAFLD and gallstone formation. Insulin resistance, a key characteristic of NAFLD, is thought to promote gallstone development by increasing hepatic cholesterol synthesis and decreasing gallbladder motility (15). Additionally, the chronic inflammation associated with NAFLD may lead to bile supersaturation with cholesterol, further elevating the risk of gallstone formation (21).
The findings of this study indicate that the high prevalence of NAFLD among symptomatic gallstone patients undergoing cholecystectomy is not influenced by gender or smoking status. The survey conducted by Ramos-De la Medina et al. did not identify a significant correlation between gender and the prevalence of NAFLD (17). Conversely, a study by Qiao et al. suggested a potential association between female gender and symptomatic GS in NAFLD (7). In the United States, a 2020 study by Latenstein et al. similarly found no significant link between NAFLD and gender (18). The absence of an association between NAFLD and these demographic factors is noteworthy (18). Previous research has reported conflicting results regarding the influence of gender and smoking on the risk of NAFLD (17, 18). While some studies have identified male sex and smoking as risk factors for NAFLD, others have not considered these factors to be significant predictors (22, 23). Potential explanations for these associations may involve metabolic, hormonal, or disease-specific mechanisms linking GSD and NAFLD (18, 19, 23). Further investigation is warranted to enhance understanding of the underlying mechanisms and their potential implications for managing these conditions (18, 23).
The findings of the current study indicate a significant association between NAFLD and prevalent metabolic conditions, including diabetes, dyslipidemia, and hypertension. The pathophysiological mechanisms linking NAFLD to these metabolic disorders, such as type 2 diabetes, impaired lipid metabolism, and hypertension, are well-documented. Insulin resistance, a hallmark of NAFLD, can contribute to the development of these metabolic abnormalities. Conversely, these metabolic conditions may exacerbate fat accumulation in the liver and accelerate the progression of NAFLD (21, 24). The co-occurrence of NAFLD and metabolic conditions in patients is clinically significant, highlighting the necessity for a comprehensive approach to managing GSD (19, 22). Clinicians should remain vigilant regarding the potential for multiple metabolic comorbidities in patients with GS and actively screen for and address these conditions to optimize patient outcomes. Early identification and management of NAFLD and associated metabolic disorders can enhance the immediate surgical outcomes of cholecystectomy while also reducing the long-term risk of adverse events, including cardiovascular disease and liver-related complications. This emphasizes the importance of a holistic approach to managing GSD in patients with NAFLD and metabolic conditions (3, 7).
The systematic review conducted by Slouha et al. identified a bidirectional relationship between NAFLD and GS. Both conditions share common risk factors, including obesity and dyslipidemia. The review demonstrated a heightened prevalence of GS among patients with NAFLD, and conversely, an increased risk of NAFLD in individuals with asymptomatic GS. This finding underscores the necessity of liver evaluation during cholecystectomy procedures (25). Insulin resistance in NAFLD leads to increased hepatic lipogenesis, impaired lipid metabolism, and TG accumulation. Hepatic fat accumulation can alter bile composition and promote the formation of cholesterol crystals, thereby contributing to the development of GS (21, 23, 25). Chronic inflammation associated with NAFLD exacerbates this process by promoting oxidative stress, hepatocyte injury, and the release of pro-inflammatory cytokines. Gallstones can perpetuate the cycle of inflammation and insulin resistance, as mechanical irritation triggers an inflammatory response. The inflammatory mediators released can impair insulin signaling and contribute to the development of insulin resistance. The bidirectional relationship between NAFLD and GSD, mediated by insulin resistance and chronic inflammation, underscores the necessity for a comprehensive management approach targeting these underlying mechanisms (23, 25).
Our results indicated that age, TG levels, cholesterol levels, and SGOT and SGPT levels were significantly associated with NAFLD in this group of patients. The correlation between advanced age and an increased likelihood of NAFLD is consistent with the typical progression of the condition. As individuals age, their susceptibility to underlying metabolic imbalances, such as insulin resistance and dyslipidemia, increases, thereby contributing to the onset and progression of NAFLD (3, 26). Also, NAFLD was closely connected to disturbances in the lipid profile, as higher levels of TG and cholesterol indicate a strong association between the two conditions. Dyslipidemia, a well-known risk factor for the onset and progression of NAFLD, can trigger liver inflammation and cell damage by causing excessive lipid buildup in the liver (24, 25). Therefore, addressing underlying lipid irregularities in managing NAFLD in gallstone patients is crucial. By concentrating on these irregularities, healthcare providers could reduce the impact of NAFLD and enhance patient outcomes. This emphasizes evaluating lipid profiles in NAFLD management, especially in patients with concurrent GSD (24, 27).
Elevated levels of TG and cholesterol have been closely associated with the development and progression of NAFLD in this patient population. Dyslipidemia, characterized by abnormalities in the lipid profile, may induce liver inflammation and cellular damage by facilitating excessive lipid accumulation in the liver, thereby directly contributing to the onset and progression of NAFLD. Furthermore, increased levels of liver enzymes, such as SGOT and SGPT, were significantly correlated with NAFLD, suggesting that liver injury and inflammation are critical pathways linking these factors. The strong association between metabolic irregularities, including dyslipidemia, and NAFLD underscores the necessity of addressing underlying lipid profile disturbances in managing NAFLD, particularly in patients with concurrent GSD (25-27).
The present study has several limitations that warrant consideration. First, the diagnosis of NAFLD was based solely on ultrasonography, which is less precise than advanced imaging techniques such as magnetic resonance imaging (MRI) or controlled attenuation parameter (CAP) for quantifying liver fat content. This limitation may have resulted in potential underestimation or overestimation of the prevalence of NAFLD in the study population. Second, unmeasured confounding variables may have influenced the observed associations between NAFLD and GSD. Lastly, the cross-sectional design of the study precludes the establishment of definitive cause-and-effect relationships. Consequently, further prospective studies are essential to gain a more comprehensive understanding of the underlying mechanisms and directionality of this association.
5.1. Conclusions
This study found that a significant proportion of symptomatic gallstone patients undergoing cholecystectomy — 31.82% — were diagnosed with NAFLD. Notably, the prevalence of NAFLD was independent of gender or smoking status, indicating that metabolic disorders linked to gallstone formation may play a role. Furthermore, the research identified a strong connection between NAFLD and common metabolic conditions, including diabetes, dyslipidemia, and hypertension, as well as factors such as age, lipid profiles, and liver enzyme levels in these patients. These results highlight the necessity for a comprehensive, multidisciplinary approach to managing GSD, specifically emphasizing early detection and targeted treatment of NAFLD and its related comorbidities. This underscores the importance of thorough screening and monitoring for NAFLD in this patient population, as addressing the underlying metabolic issues could be crucial for improving patient outcomes.