1. Background
Millions of people are affected with hepatitis C virus (HCV) infection worldwide that proceeds to cirrhosis in about one-fifth of them (1, 2). African and Asian countries reported elevated infection rates in comparison to Northern American as well as Northern and Western Europe (3). In Egypt, about 13.8% of population is affected by HCV, achieving the highest prevalence of HCV all over the world (6%-28%) (4-8). Hepatocellular carcinoma (HCC) is one of the most common non-dermatologic cancers in the world (9). It is the fifth most common cancer and the third most frequent cause of cancer-related death (10). The annual risk of developing HCC following cirrhosis is between 1% and 6% (11, 12). The mortality from HCC is substantial with survival rates as low as 1% in two years in untreated patient (13, 14).
Serum α-fetoprotein (AFP) levels are not frequently elevated in a significant proportion in patients with early-stage, potentially curable, HCC. Moreover, AFP levels may increase transiently, intermittently, or permanently in patients with viral hepatitis without HCC (15). Increase in AFP is most often paralleled by an increase in aminotransferase levels; however, the diagnostic dilemma occurs in differentiating HCC from a viral illness when an increase in AFP levels does not correlate with an increase in aminotransferase or occurs in the presence of normal levels (16). Therefore, other markers should be studied in an attempt to identify a more sensitive laboratory test.
Cytokine production is thought to play an important role in the recruitment of tumor-associated inflammatory cells, induction of angiogenesis, and direct modulation of tumor cell proliferation (17, 18). Inflammatory cytokines including tumor necrosis factor-α (TNF-α) are an integral part of inflammation in chronic HCV infection. TNF-α mediates its effects by binding to two distinct cell surface receptors, namely, tumor necrosis factor receptor I (TNFR-l) and TNFR-II. Subsequently, proteolytic cleavage of the extracellular parts of these receptors elicits the soluble TNF receptors, i.e. sTNFR-Iα (-p55) and sTNFR-IIα (-p75). Therefore, sTNFR levels are considered sensitive and reliable indicators of the activation of TNF-α system, preferable to TNF-α itself (19).
2. Objectives
In this study, we investigated the value of serum level of sTNFR-IIα in the diagnosis and early detection of HCC and its role as a potential tumor marker in patients with chronic HCV infection.
3. Patients and Methods
3.1. Patients
This study was performed in Internal Medicine Department, Faculty of Medicine, Cairo University, Cairo, Egypt, between May 2012 and December 2013. It included 110 subjects who were assigned to five groups. Group I consisted of 20 patients with chronic HCV, persistently normal transaminases for more than six months, and without liver cirrhosis. Group II included 20 patients with chronic HCV infection, elevated transaminases, and without liver cirrhosis. Group III included 20 patients with chronic HCV infection and liver cirrhosis. Group IV included 20 patients with chronic HCV infection, liver cirrhosis, and HCC diagnosed by abdominal ultrasonography, triphasic computed tomography of abdomen and serum AFP before receiving any treatment. Group V included 30 healthy individuals as a control group.
3.1.1. Ethical Approval
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The ethical committee of Faculty of Medicine, Cairo University, approved this study. Written informed consents were obtained from all participants.
3.1.2. Exclusion Criteria
All patients with HBV infection or HBV-HCV coinfection, autoimmune or drug-induced hepatitis, other autoimmune diseases, and those with renal, cardiovascular, or respiratory diseases were excluded from the study. In addition, patients with any malignancy other than HCC and pregnant women were excluded.
3.2. Methods
All individuals were subjected to full history taking, clinical examination, and abdominal ultrasonography. In addition, the following laboratory parameters were evaluated: liver function tests including serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), bilirubin, albumin (Alb), prothrombin time (PT), and prothrombin concentration, complete blood count (CBC), HBsAg ,anti-HCV Abs (by third generation ELISA), qualitative assessment of HCV-RNA in serum by nested RT-PCR assay (20), AFP by ELISA (21), and serum sTNFR-IIα.
Serum sTNFR-IIα levels were measured by ELISA kit (DR200) using quantitative sandwich enzyme immunoassay technique (22). Kit was supplied from R & D system Europe, Ltd. (19 Barton Lane, Abingdon Science Park, Abingdon, UK). A monoclonal antibody, specific for sTNFR-IIα, was precoated onto a microplate. Standard and study samples were pipetted into the wells and immobilized antibodies bound to any present sTNFR-IIα. After washing any unbound substances away, an enzyme-linked polyclonal antibody, specific for sTNFR- II α, was added to the wells. Following a wash to remove any unbound antibody-enzyme reagent, a substrate solution was added to the wells and color was changed in proportion to the amount of sTNFR-IIα bound in the initial step. The color development was stopped and the intensity of the color was measured. The minimal detectable dose of sTNFR-IIα ranged from 0.2 to 2.3 pg/mL.
3.2.1. Statistical Methodology
The data were coded and entered into SPSS 15 (SPSS Inc., Chicago, Il, USA). The data were summarized using descriptive statistics, mean, and standard deviation. Statistical differences between groups were tested using Chi square test for qualitative variables, independent-samples t test with multiple comparisons post hoc for quantitative, normally distributed variables, and nonparametric Mann–Whitney U test and Kruskal-Wallis test for non-normally distributed quantitative variables. Two-way ANOVA test was used to compare variance of each marker levels among four different groups and the controls. P value < 0.05 was considered as statistically significant (23).
4. Results
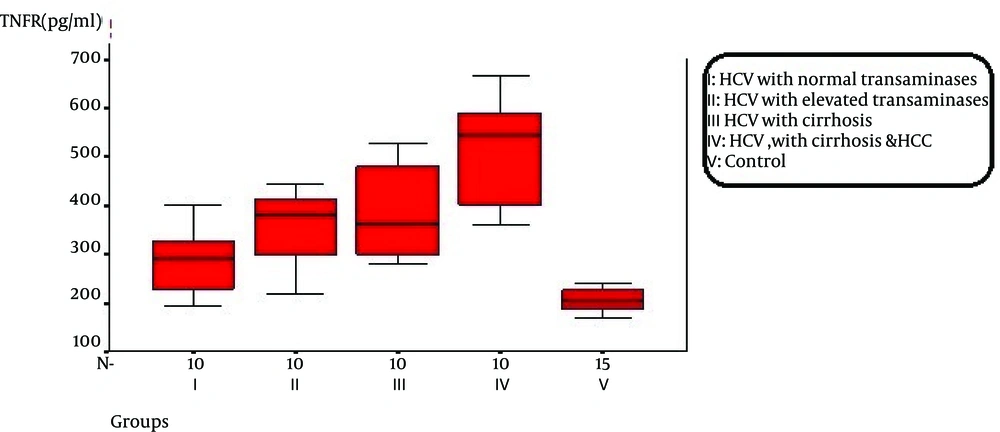
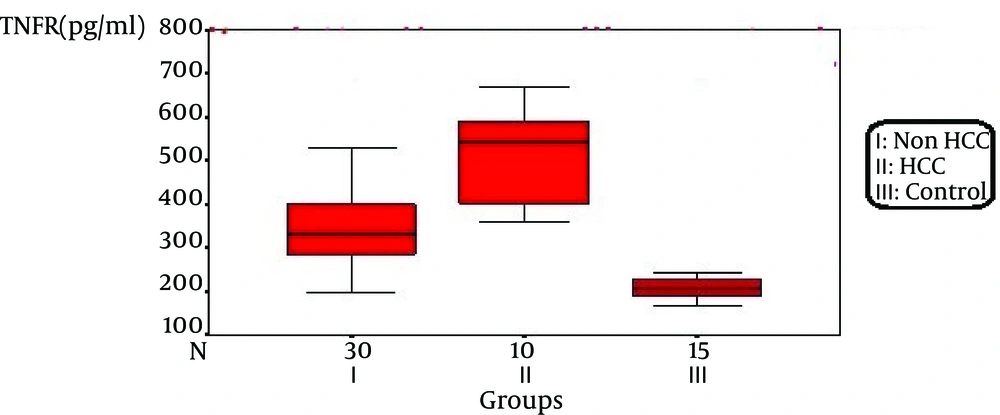
Statistical analysis of age and gender showed no significant difference among the studied groups (Table 1) The hemoglobin (Hb) level, total leucocytic count (TLC), platelet count, prothrombin concentration, and serum Alb were significantly reduced (P < 0.05) in groups III and IV. The serum bilirubin, AST, and ALT were significantly higher in groups II, III, and IV in comparison with groups I and V. The serum AFP level was significantly elevated in groups III and IV in comparison to the other noncirrhotic groups (I and II) and the control, with the highest level in the HCC group. On the other hand, the sTNFR-IIα level was significantly higher in HCC group (511 ± 10.7 pg/mL) in comparison to the other noncirrhotic (group I,357 ± 6.4 pg/mL; and group II 383 ± 7.1 pg/mL) and cirrhotic (group III, 384 ± 1.3 pg/mL)and the control groups (205 ± 22.5 pg/mL). There was a statistically significant difference among the non-HCC groups (I, II, and III) and the control; however, no significant difference could be detected among these groups in relation to each other (Tables 2 and 3 ; Figures 1 and 2).
Our results revealed no significant correlation between the level of TNFR-IIα and demographic and laboratory parameters within the different groups, except in group II that we found a significant correlation between TNFR-IIα and either AST (r = 0.45; and P < 0.05) or ALT (r = 0.25; and P < 0.05).
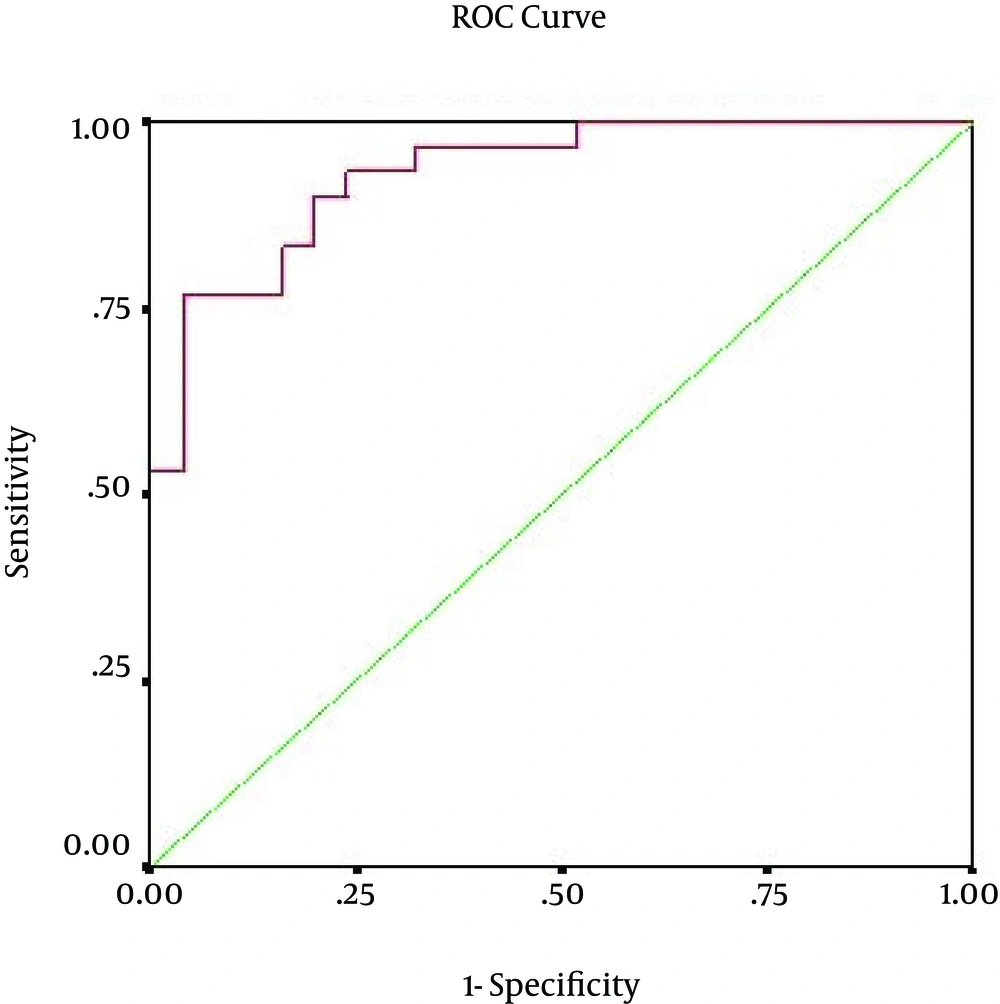
The sTNF-IIα is considered a better positive marker than being a negative one in diagnosing HCC with higher sensitivity (99%) and accuracy (87%) at a cutoff value of ≥ 250 pg/mL (Table 4).
| Variable | Group I (N = 20) | Group II (N = 20) | Group III (N = 20) | Group IV (N = 20) | Controls (N = 30) |
|---|---|---|---|---|---|
| Age a | 53.7 ± 4 | 45 ± 4.6 | 54.5 ± 3 | 46 ± 4.8 | 48 ± 7 |
| Sex | |||||
| Male | 9 (90) | 9 (90) | 8 (80) | 8 (80) | 14 (93.3) |
| Female | 1 (10) | 1 (10) | 2 (20) | 2 (20) | 1 (6.7) |
aValues are expressed as mean ± SE or No. (%).
| Variable | Group I (No. 20) | Group II (No. 20) | Group III (No. 20) | Group IV (No. 20) | Controls (No. 30) |
|---|---|---|---|---|---|
| HB, gm/dL | 12 ± 1.1 | 11.9 ± 1.3 | 9.6 ± 0.9 | 9.3 ± 1 | 13.9 ± 0.8 |
| TLC | 5 ± 0.9 | 4 ± 1.6 | 3.7 ± 2.7 | 3.6 ± 0.6 | 4.7 ± 0.7 |
| Platelets | 365 ± 7.1 | 162 ± 5.8 | 128 ± 3.5 | 119 ± 7.3 | 380 ± 6.2 |
| PC,% | 91 ± 5.6 | 85 ± 7.8 | 39.5 ± 6 | 33.8 ± 4.3 | 99.5 ± 0.8 |
| Albumin, gm/dL | 4 ± 0.6 | 3.6 ± 0.7 | 2.6 ± 0.6 | 2.08 ± 0.6 | 5 ± 0.7 |
| Total bilirubin, mg/dL | 0.69 ± 0.9 | 1.1 ± 0.9 | 3.4 ± 1.3 | 4.1 ± 2.14 | 0.48 ± 0.20 |
| AST, mg/dL | 32 ± 3 | 62 ± 1.6 | 45 ± 1.3 | 50 ± 9.5 | 26.2 ± 6 |
| ALT, mg/dL | 34 ± 4 | 74 ± 1.4 | 41 ± 1.2 | 43 ± 4.7 | 28 ± 6.6 |
| AFP, ng/mL | 5.6 ± 4 | 7.3 ± 4 | 13 ± 4.7 | 1882 ± 330 | 3.8 ± 0.8 |
| sTNFR-IIα, pg/mL | 357 ± 6.4 | 383 ± 7.1 | 384 ± 1.3 | 511 ± 10.7 | 205 ± 22.5 |
aValues are expressed as mean ± SE.
bMeans followed by the same superscript letter within the same row means insignificant variation (P > 0.05).
| Variable | Non-HCC (N = 60) | HCC Group (N = 20) | Controls (N = 30) |
|---|---|---|---|
| Mean ± SD | 342 ± 11.4 | 511 ± 10.7 | 205 ± 22.5 |
aValues are expressed as mean ± SE. Statistically significant level is defined as P<0.05.
bMeans followed by the same superscript letter within the same row means non-significant variation (P > 0.05).
| Variable | No. (%) |
|---|---|
| Best cutoff = 250, pg/Ml | |
| AUC a | 0.93 |
| Sensitivity | 99 |
| Specificity | 72 |
| PPV | 78 |
| NPV | 95 |
| Accuracy | 87 |
aAbbreviations: AUC, area under the curve; PPV, positive predictive value; and NVP, negative predictive value.
5. Discussion
Chronic liver disease (CLD) is characterized by raised cytokines level that might represent a sequel of liver dysfunction as well as an inflammatory process (24). Cytokines-induced discrepancy between T helper 1 (Th1) and T helper 2 (Th2) can extend inflammation, leading to necrosis, fibrosis, and CLD with consequent possible progression and evolution of HCC (24-26).
Such elevated serum cytokines could be used as biomarkers for early diagnosis of HCC in patients with HCV-related CLD. In addition, they were previously investigated for possible use as predictors for treatment response to interferon (IFN) in patients with HCV genotype-4 infection. Numerous cytokines including soluble Fas (sFas), sTNFR-IIα, interleukin-2 receptor (IL-2R), and interleu kin-8 (IL-8) are involved in HCC invasion and metastasis (27, 28).
Additionally, a recent report showed over-expression of CD5L in HCV-HCC in comparison to HCV-cirrhosis. CD5L is a secreted glycoprotein belonging to the scavenger receptor cysteine-rich superfamily. Although biomarker studies on liver tissues could be a useful strategy for determining new pathogenic biomarkers for diagnostic and/or prognostic processes, serum has much main concern for finding reasonably priced, appropriate, and noninvasive biomarkers (29).
Nonetheless, there are contradictory reports on these markers as predictors for HCC; it was found that IL-2R was not detectable in patients with HCC in comparison to patients with chronic hepatitis and liver cirrhosis (30). Moreover, a previous study revealed that, levels of IL-8 were significantly lower in patients with HCC than in the other groups (31) while contradictory studies found that serum IL-8 levels were markedly elevated in most patients with HCC in comparison to healthy subjects (32) and were overexpressed in the HCC cells in comparison with the non-affected liver cells(33). Consequently, due to the large multitude of reported CLD-associated biomarkers, selecting the most useful biomarkers in clinical practice has been more a challenging. Notably, sTNFR-IIα was closely correlated with disease progression in chronic HCV infection. Moreover, TNFRs up-regulation might alter host response and potentially add to liver damage (34).
Thus, in the current study we determined the value of serum level of sTNFR-IIα in the diagnosis and early detection of HCC in patients with chronic HCV infection. Our results revealed that there was no statistically significant difference regarding age between patients with HCC and other studied groups, which disagreed with Zekri et al. who stated significantly higher mean of patients' age with HCC than that of the other groups (31). This might be related to under diagnosis of early stage cirrhosis, which had started at younger age, possibly due to low rates of biopsy. This was in concert with results of a previous cohort (35) that reported a significant increase in the prevalence of cirrhosis and HCC in patients with HCV infection over the past ten years. The authors added that after adjustment for sex and increasing age of the HCV cohort, the upward slopes in the prevalence of cirrhosis and HCC were lower than the corresponding slopes in the crude rates. They concluded that aging of the patients with HCV infection explains a significant proportion of the rising trend in the prevalence of cirrhosis and HCC (20% and 47%, respectively) with time. Another explanation is that patients with HCV acquired their infection earlier and thus, would have had their infection for a longer time with age progression. If it was true, it would mean that the HCC prevails. Lastly, records from previous studies are liable to be misjudged; the data from recalibrated mathematical models suggest that the age prevalence prevalence of HCV and cirrhosis might be definitely higher than was previously reported (36).
In addition, we found that the serum Hb level was significantly lower in patients with liver cirrhosis (group III) and HCC (group IV) than the other groups. This difference could be explained by acute and chronic gastrointestinal blood loss, folate deficiency, hypersplenism, bone marrow suppression, and the anemia of chronic disease. This is in agreement with Sakisaka et al. who stated that although raised serum erythropoietin (EPO) levels might be present in up to 23% of patients with HCC, elevations in Hb concentration or packed cell volume are uncommon and most patients are anemic at diagnosis because of other side effects of the tumor (37).
In the present study, the total leucocytic and platelet counts were significantly reduced in patients with cirrhosis and those with HCC in comparison with the other groups .This finding was in agreement with the results by Pratt and Kaplan, explaining that observed leucopenia with liver cirrhosis might be due to hypersplenism with splenic margination while thrombocytopenia might be mainly caused by portal hypertension with attendant congestive splenomegaly. An enlarged spleen can result in temporary sequestration of up to 90% of the circulating platelet mass. Decreased thrombopoietin levels might also contribute to thrombocytopenia (38).
Our study revealed that the serum Alb and prothrombin concentration were significantly lower in patients with cirrhosis and those with HCC in comparison with the other groups, which could be explained by decreased synthesis of Alb and coagulation factors by the diseased liver. It was in agreement with the report by Tripod et al. showing poor utilization of vitamin k in advanced parenchymal liver disease (39).
The present study revealed that the serum transaminases were significantly elevated in patients with HCC in comparison to those with persistently normal ALT levels and the controls but with insignificant difference with the cirrhotic group. In agreement with our results, Zekri et al. and Sugiyama et al. stated that liver function tests values were significantly elevated in patients with HCC when compared to those with CLD (31, 40). Moreover, Young et al. reported that patients with HCC had the highest values for various concurrently measured liver function tests, AST/ALT, ALT, and AST than patients with cirrhosis did (41).
Although authors (31) confirmed that serum TNFR-II and AFP might be used as combined markers in patients with HCV infection who are at high risk of developing HCC, additional studies are mandatory to reevaluate these findings before their application at the population level. Our study revealed extraordinary high amounts of AFP values (P < 0.05) in patients with HCC in comparison to other groups. Moreover, sTNFR-IIα values were significantly increased in the same group of patients (HCC) in comparison to other groups. High serum levels of AFP in the current study could be explained by the presence of other factors that might affect AFP and sTNFR-IIα levels in serum as high levels of serum AFP have been accompanied with larger tumor size, bilobar association, immense or diffuse-type tumors, and portal vein thrombosis(42). These factors need further elucidation in more detailed studies. On the other side, low sTNFR-IIα level in comparison to AFP in the current study might be related to the histologic pattern of the disease. Such hypothesis could be ascertained by the previous published results stating that enhanced TNFRs in chronic HCV infection might reflect the histologic activity of the disease (34).
Our results showed no statistically significant correlation between sTNFR-IIα and different laboratory variables among different groups, except in group II where there was a statistically significant positive correlation between the levels of sTNFR-IIα and AST and ALT (P < 0.05). In agreement with our results, Itoh et al. reported positive correlations between sTNFR-IIα and several liver disease markers (ALT, AST, and gammaglutamyl transferase) as well as with Knodell’s histologic activity index score in subjects with chronic HCV infection (43).
We reported that levels of sTNFR-IIα were significantly elevated in patients with chronic HCV infection in comparison to the control subjects (P < 0.05). Similar results were reported by Zekri et al., who stated that levels of sTNFR-IIα were elevated in patients with PNALT, CLD, and HCC (31). Moreover, Kato et al. mentioned that sTNFR-IIα was closely correlated with disease progression in chronic HCV infection (12). On the same line, Kallinowski et al. (34), Aderka et al. (44), and Robert et al. (45) stated that HCC cases experience an elevated type 1 immune response before the development of HCC and that levels of sTNFR-IIα and soluble intracellular adhesion molecule 1 (sICAM-1) were positively correlated with each other. On the other hand, Kakumu et al. reported that the serum level of sTNFR- IIα was highest in both HCC and CLD groups (46).
The rate of progression to end-stage liver disease might be related to an up-regulation of the TNFα/Fas pathways and an age-dependent host response (47). Activities of TNFα are mediated through sTNFR-I and II. Released proinflammatory TNFα by host and tumor cells is an important factor in initiation, proliferation, angiogenesis, and metastasis of various cancer types (48, 49).
Regarding the mean levels of serum sTNFR-IIα in the present study, a significant difference was shown between the HCC and the non-HCC groups. The best cutoff value for diagnosing HCC was ≥ 250 pg/mL with sensitivity of 99%, specificity of 72%, positive predictive value of 78%, and negative predictive value of 95% with 87% accuracy. However, a higher cutoff value was reported by Zekri et al. who stated that levels of sTNFR-IIα were significantly elevated in patients with HCC in comparison to those with PNALT and CLD. Analysis of sTNFR-IIα by receptive operative curves revealed satisfactory values regarding sensitivity (70.6%) and specificity (90%) at a cutoff value of ≥ 398 pg/mL (31).
In conclusion, although serum AFP level is still considered as the key serum marker for HCC diagnosis, it could be elevated in some noncancerous liver insults and could be at a low level in some patients with HCC (50, 51). Consequently, the present study elucidates the prospective role of sTNFR-IIα as a potential marker of HCC. We revealed that the serum level of sTNFR-IIα was significantly higher in patients with HCC in comparison to the other groups. The sTNFR-IIα at a cut off value ≥ 250 pg/mL is highly suggestive of HCC in patients with chronic HCV infection and liver cirrhosis. However, auxiliary studies, involving larger scales of patients at various stages of CLD and HCC, in addition to complementary assessment of the effect of HCC treatment on the serum level of sTNFR-IIα are mandatory.
References: