1. Background
Chronic hepatitis B virus (HBV) infection and liver cancer caused by HBV is one of the most serious but frequently neglected health disparities among U.S. foreign-born immigrants from China, Korea, Vietnam (1) and other Asian countries where hepatitis B is endemic. These immigrants are more likely to have been exposed to HBV and to live with chronic hepatitis B than the U.S.-born population. Most studies in Asian Americans have presented test results of HBsAg, which indicate whether a person was infected, or hepatitis B surface antibody (anti-HBs), which, if positive, implies that the person has developed immunity from HBV infection (2).
The presence of total hepatitis B core antibody (anti-HBc) indicates previous or ongoing HBV infection when a person has a result of positive anti-HBs (2). Most U.S. screening programs in Asian American or other communities do not routinely test for or report the presence of total hepatitis B core antibody (anti-HBc) (3), which, when positive indicates previous or ongoing HBV infection when combined with a positive anti-HBs result or, when negative indicates that an individual is immune due to hepatitis B vaccination when combined with a positive anti-HBs result (2). In acute hepatitis B infection, anti-HBc appears at the onset of symptoms and persists for life (2).
Most of the literature on anti-HBc is limited to liver donation due to the higher likelihood of hepatitis B reactivation in the allograft from anti-HBc-positive liver donors (4). Yet it is important to assess the prevalence of anti-HBc among high-risk groups such as foreign-born Asian Americans because of their much higher prevalence compared to that of the general population in the U.S.
The overall U.S. rate of anti-HBc presence was 4.6% in 1999 - 2008 and 6% in 2011 - 2012 in a nationally representative sample from the national health and nutrition examination survey (NHANES) data (5, 6). Meanwhile, studies have found that the rate of infection is at least three times higher among Asian Americans, at 19% among foreign-born college students (7); 34% in large Asian American community screening data (8); 43% in a refugee population from Asia (9); and 53% in a community health fair screening (10). Based on these numbers, it appears that foreign-born Asian Americans are commonly exposed to HBV prior to coming to America.
The purpose of this study is to estimate the HBV prevalence and socio-demographic determinants of exposure to HBV in the foreign-born Asian American population, focusing on Chinese, Korean and Vietnamese Americans as the target group. Besides reporting the prevalence of individuals who are infected (HBsAg positive) and susceptible or unprotected (HBsAg, anti-HBc, and anti-HBs all negative), we also present the number of individuals with negative HBsAg and the various combinations of anti-HBc and anti-HBs, which are rarely reported in the literature.
2. Methods
The study was approved by the committee on human research of Johns Hopkins Bloomberg school of public health. All participants signed a written informed consent form. The study period for the Asian American liver cancer prevention program (here after the Program) period was from April 2013 to March 2014.
2.1. Participants
Using a non-probability sampling method in the Baltimore-Washington Metropolitan Area, foreign-born Asian American adults (≥ 18 years of age) who had never been tested for hepatitis B, were recruited from the community. The Baltimore-Washington metropolitan area (i.e., Maryland, Washington DC, northern Virginia) has a combined population of 7,390,422 (11). The proportion of Asian Americans was 4.53% in Baltimore metro area and 9.27% in Washington metro area (12).We gained critical access to the recruitment locations because we had long-term connections to the community from serving on the advisory board of a local community-based organization (CBO) since 2008. Recruitment locations and other recruitment efforts included: (1) advertisements describing the study in local Chinese, Korean, and Vietnamese newspapers, and in local Asian grocery stores; individuals who responded to the advertisement by calling the telephone number listed on them were screened for eligibility during that telephone call and invited to participate in the study; (2) lay health workers (LHWs) who were previously trained by members of the research team and capable of educating community members about HBV announced the screening events and information about the study to the community; and (3) contact with church and temple leaders to arrange recruitment days during which church and temple members were recruited to participate in the study on the spot. Most participants were recruited directly by the LHWs or learned about screening events by word-of-mouth (13).
2.2. Data Collection Procedures
Pre-test/Education program. After providing written informed consent, all of the participants were asked to complete a self-administered questionnaire in English, Chinese, Korean, or Vietnamese with the assistance of a bilingual interviewer when necessary. Then, all of the participants were instructed to read culturally integrated and linguistically appropriate educational materials (e.g., a photonovel) that had been developed and validated for efficacy from prior studies (14-16).
HBV screening test/Informing the results. All participants received hepatitis B testing for HBsAg, HBsAb, and HBcAb (hepatitis B core antibody). Blood samples were drawn by phlebotomists and transported to Quest Diagnostics. The results were sent by quest diagnostics to the program director, who made an aggregate record of the findings and a copy of each individual lab results. One week after the screening, copies were mailed to participants along with a notification letter in English and the participant’s native language. The notification letter classified test results into one of three categories: immune, susceptible, or infected. We recommended that those categorized as susceptible to have a series of 3 vaccinations. For those categorized as infected, a medical doctor called to provide medical counseling and further follow-up treatment in their language preference.
2.3. Interpretation of Hepatitis B Serologic Test Results
The HBsAg and anti-HBc tests indicate the presence or absence of the biomarker; however, a negative test result for HBsAg or anti-HBc does not mean that the person has never been infected because 0.5% of HBsAg carriers spontaneously clear the infection annually (17). The anti-HBs test is quantitative: ≥ 10 µIU/mL as positive antibody titer, per CDC guideline (18). The detection of anti-HBs indicates a prior immunologic exposure to the antigen or vaccine. Hepatitis B testing results fall into 5 categories: (1) currently infected (HBsAg(+), anti-HBc(+), anti-HBs(-)); (2) immune due to previous infection (HBsAg(-), anti-HBc(+), anti-HBs(+)); (3) immune due to vaccination (HBsAg(-), anti-HBc(-), anti-HBs(+)); (4) susceptible to HBV infection (HBsAg(-), anti-HBc(-), anti-HBs(-)); and (5) unclear interpretation with most common possibility of resolved infection (HBsAg(-), anti-HBc(+), anti-HBs(-)).
2.4. Statistical Analysis
We used descriptive data analysis to explore the data using chi-square tests. Logistic regression was used to examine whether previous exposure to HBV infection (0 = anti-HBc (-); 1 = anti-HBc (+)) was associated with gender, ethnicity, age, education, spoken English proficiency, family history of HBV infection, and having health insurance. Crude and adjusted odds ratios (ORs) and 95% confidence interval (CIs) were obtained. Data were analyzed with Stata version 13 (19).
3. Results
A total of 600 foreign born Asian American adults (201 Chinese, 198 Korean, and 201 Vietnamese) participated in the study. Their mean age was 47.3 (SD = 11.8) with a range of 18 to 91 years; 58% were female. About 48% were college graduates or had higher education. About 13% had a family history of HBV infection. About a half had health insurance (see Table 1).
| Characteristics | Valuesa |
|---|---|
| Age | 47.31 ± 11.82 |
| Range | 18 - 91 |
| Race/ethnicity | |
| Chinese | 201 (33.5) |
| Korean | 198 (33.0) |
| Vietnamese | 201 (33.5) |
| Gender | |
| Male | 252 (42.0) |
| Female | 348 (58.0) |
| Education | |
| < High school | 86 (14.5) |
| High school graduate | 152 (25.6) |
| Vocational/some college | 71 (11.9) |
| College graduate+ | 285 (48.0) |
| Employment | |
| No | 202 (33.7) |
| Yes | 398 (66.3) |
| Spoken English Proficiency | |
| Fluent | 29 (4.8) |
| Well | 112 (18.7) |
| So-So | 234 (39.0) |
| Poorly | 166 (27.7) |
| Not at all | 59 (9.8) |
| Family history of HBV infection (= yes) | 78 (13.0) |
| Having Health insurance (= yes) | 307 (51.5) |
aValues are expressed as No. (%) or mean ± SD.
As shown in Table 2, among those 600 screened participants, 33 had chronic HBV infection, yielding a prevalence of 5.5% (CI = 3.7% - 7.3%). The prevalence of HBV infection among Chinese, Korean, and Vietnamese Americans was 6.5%, 5.6%, and 4.5% (P = 0.68). A total of 168 (28.0%) were immune due to previous exposure to HBV, and 166 (27.7%) were immune due to hepatitis B vaccination. A total of 171 (28.5%) were susceptible. Sixty two participants (10.3%) were in the category of unclear interpretation with the most common possibility of resolved infection (HBsAg(-), anti-HBc(+), anti-HBs(-)). The anti-HBc test was positive in 263 (43.8%; CI=39.8% - 47.9%) screened participants, presumably due to the previous exposure to HBV. Statistically significant ethnic differences emerged in the exposure (P < 0.001); Vietnamese (53.2%) had the highest exposure to HBV, then Koreans (43.4%) and Chinese (34.8%).
| Interpretation | Test (Result) | No. (%) |
|---|---|---|
| HBV infection | HBsAg (+) | 33 (5.5) |
| Anti-HBc (+) | ||
| Anti-HBs (-) | ||
| Immune due to natural infection | HBsAg (-) | 168 (28.0) |
| Anti-HBc (+) | ||
| Anti-HBs (+) | ||
| Immune due to HBV vaccination | HBsAg (-) | 166 (27.7) |
| Anti-HBc (-) | ||
| Anti-HBs (+) | ||
| Susceptible | HBsAg (-) | 171 (28.5) |
| Anti-HBc (-) | ||
| Anti-HBs (-) | ||
| Interpretation unclear; four possibilities | ||
| Resolved infection (most common) | HBsAg (-);Anti-HBc (+);Anti-HBs (-) | 62 (10.3) |
| False-positive anti-HBc | ||
| “Low level” chronic infection | ||
| Resolving acute infection | ||
| Total | 600 (100) |
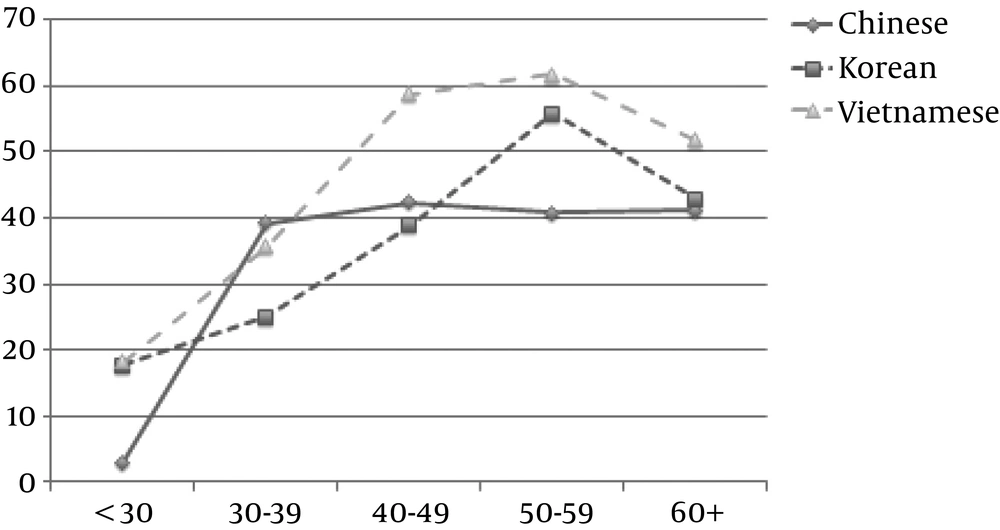
There were some age variations in exposure to HBV by ethnicity. For Vietnamese Americans, prevalence of HBV exposure was highest among those 51 to 60 years of age (61.8%), followed by those 41 and 50 years of age (58.8%). For Korean Americans, prevalence of HBV exposure was also highest among those participants 51 to 60 years of age (55.8%), followed by those older than 60 (42.9%). For Chinese Americans, prevalence of HBV exposure was lowest among those participants younger than 30 years age (3.0%), compared to older participant age groups (see Figure 1).
We examined the social determinants associated with previous infection of HBV (anti-HBc positive) (see Table 3). In bivariate analysis, gender, age, race/ethnicity, educational level, and spoken English proficiency correlated to previous HBV infection (P < 0.05). In multivariate analysis, females were less likely to have prior infection than males (OR = 0.55, 95% CI, 0.38 - 0.79). Those in the 51 - 60 age group were more likely to have been exposed to HBV than those under 30 (OR = 10.85, 95% CI, 4.29 - 27.4). Compared to those who had less than high school education, those with a high school diploma (OR = 0.37, 95% CI, 0.21 - 0.67) and those with more than college education (OR = 0.28, 95% CI, 0.15 - 0.53) were less likely to have prior exposure. Those who had a family history of HBV infection were more likely to have prior exposure than those without a family history (OR = 1.76, 95% CI, 1.01 - 3.04).
| Characteristics | Prevalence of Anti-HBc, No. (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| All Participants | 263 (43.8) | ||
| Gender | |||
| Male | 123 (48.8) | 1.00 | 1.00 |
| Female | 140 (40.2) | 0.71 (0.51, 0.98)a | 0.55 (0.38, 0.79)a |
| Race/ethnicity | |||
| Chinese | 70 (34.8) | 1.00 | 1.00 |
| Korean | 86 (43.4) | 1.44 (0.96, 2.15) | 1.18 (0.72, 1.92) |
| Vietnamese | 107 (53.2) | 2.13 (1.43, 3.18)a | 1.38 (0.84, 2.26) |
| Age group, y | |||
| ≤ 30 | 6 (9.0) | 1.00 | 1.00 |
| 31 - 40 | 32 (38.6) | 6.38 (2.47, 16.5)a | 6.41 (2.38, 17.3)a |
| 41 - 50 | 97 (49.5) | 9.96 (4.11, 24.1)a | 9.31 (3.67, 23.6)a |
| 51 - 60 | 101 (52.6) | 11.28 (4.66, 27.3)a | 10.85 (4.29, 27.4)a |
| > 60 | 27 (43.5) | 7.84 (2.95, 20.8)a | 6.29 (2.22, 17.78)a |
| Education | |||
| < High school | 59 (68.6) | 1.00 | 1.00 |
| High school graduate + | 102 (45.5) | 0.38 (0.23, 0.65)a | 0.37 (0.21, 0.67)a |
| College graduate+ | 100 (35.1) | 0.25 (0.15, 0.41)a | 0.28 (0.15, 0.53)a |
| Spoken English proficiency | |||
| Not at all/poorly | 120 (53.3) | 1.00 | 1.00 |
| So so | 94 (40.2) | 0.59 (0.41, 0.85)a | 0.87 (0.56, 1.34) |
| Well/fluent | 49 (34.8) | 0.47 (0.30, 0.72)a | 0.96 (0.54, 1.71) |
| Family history of HBV infection | |||
| No | 149 (41.9) | 1.00 | 1.00 |
| Yes | 39 (50.0) | 1.39 (0.85, 2.27) | 1.76 (1.01, 3.04)a |
| Not sure | 74 (45.1) | 1.14 (0.79, 1.66) | 1.08 (0.71, 1.63) |
| Having health insurance | |||
| No | 137 (47.4) | 1.33 (0.96, 1.84) | 1.07 (0.72, 1.60) |
| Yes | 124 (40.4) | 1.00 | 1.00 |
aP < 0.05.
4. Discussion
The 5.5% HBV infection rate among our convenience samples of foreign-born Asian American recruited in the Baltimore-Washington Metropolitan Area was much lower than that in some studies published in the past five years: 13% for Asian immigrants in New York city (19) and 13.6% for Asian Americans at a community health fair in Houston (10); but it was similar to that in other studies: 5.2% for Asian Americans recruited at community screenings in Los Angeles County (8). The large variation in infection rates could be due to different backgrounds among the sample populations, such as ethnicity, and other socio-demographic variables, and to different recruitment methods.
Our study is one of the first studies to examine the effectiveness of a hepatitis B test that accounts for anti-HBc in addition to HBsAg and anti-HBs. Anti-HBc was the marker routinely examined in past population-based studies among Asian Americans. Having information on anti-HBc allows us to identify past infection or vaccination history, so that we can assess the population’s current status or need and so that we can help public health professionals plan for educational programs or behavioral interventions. Furthermore, our study reports results from a larger and more diverse sample size than most studies done on Asian Americans with serological tests (7, 9, 10).
Based on seroprevalence of positive anti-HBc, our study shows that almost half of the population had been exposed to HBV. This rate of presence of anti-HBc was much higher than the national average (5, 6), but comparable to the results found from other studies of Asian immigrants (9, 10) and studies of individuals from HBV-endemic Asian countries (20, 21). Our finding indicates that Asian Americans are substantially more likely to have been exposed to HBV than the general U.S. population.
Interestingly, about 10% of our study participants were HBc positive in the absence of both HBsAg and anti-HBs. This result raises four possibilities for interpretation: 1) resolved infection; 2) false-positive anti-HBc; 3) “low-level” chronic infection; or 4) resolving acute infection. If full recovery from acute HBV does not occur, the virus may lie dormant (i.e., at a low level of chronic infection), with the possibility of reactivation (22). Thus, individuals with this result may be at risk of virological and clinical reactivation of occult HBV infection under certain clinical conditions, such as HIV infection and organ transplantation (23).
Our study confirmed the results of some studies that the presence of anti-HBc among non-infected individuals generally increased with age (18, 20, 24, 25). However in our study, the presence of anti-HBc peaked among those in the 51 - 60 age group while in a previous study of a large foreign-born Chinese and Korean American sample, it peaked among those older than 60 years (8). We also found that individuals younger than 30 years of age had the lowest presence of anti-HBc. This may be a due to the fact that the HBV vaccine was introduced in the immigrants’ home countries in more recent decades. In particular, it was introduced in China in the 1980s and in Korea and Vietnam in the 1990s (26).
We found a significant association between a positive anti-HBc test result and male sex, less education, and a family history of HBV infection. The prominence of male sex was expected because it was similar to the results of other studies of HBV-endemic Asian countries (22, 23, 25) and Asian refugees in Minnesota (9). Few other Asian American studies have examined level of education as a factor associated with the prevalence of anti-HBc. Consistent with previous studies (14, 27), our study significantly correlated level of education with chronic HBV infection among Asian Americans. The inadequate apparatus of disease control and screening and vaccination policy in the origin countries resulted in hepatitis B infection-related health disparity among individuals with different educational levels. We also expected to see the correlation with a family history of HBV infection from our knowledge of HBV transmission route among Asian immigrants, when many individuals were infected perinatally because their mothers had chronic infection and they did not receive appropriate post exposure prophylaxis (2).
There are some limitations to our study. First, to collect a sample of the hard-to-reach population of foreign-born Asian Americans, we mainly used non-probability sampling methods to recruit individuals through CBOs. The results of this non-probability sampling may not be representative of the entire population of foreign-born Asian Americans. Thus, the finding in these concentrated populations in the Baltimore-Washington Metropolitan Area may not be generalizable to Asians who are living in other communities or geographical settings. In addition, we know that the national population-based study (i.e., NHANES) is limited because it cannot recruit non-English-speaking Asians and does not have an adequate sample size of Asian Americans for sub-group analysis. On the other hand, by using a non-probability sampling method, we were able to recruit a large sample population. We hope the advantage gained by a large sample size outweighs the limited representativeness of our sample. Second, our recruitment strategies might underestimate chronic HBV prevalence among foreign-born Asian Americans. One of the inclusion criteria is not having previous hepatitis B testing. Those who already knew that they were infected might not have participated in our study; hence, the prevalence of HBV infection might have been underestimated. Lastly, we did not test for AST or ALT levels and IgM anti-HBV; therefore, we could not distinguish chronic HBV infection from acute HBV infection. We also cannot differentiate whether those with unclear interpretation (HBsAg(-), anti-HBc(+), anti-HBs(-)) had occult HBV infection, considering that we did not conduct HBV DNA detection in blood or in the liver with sensitive diagnostic tests.
In summary, based on our findings, we should consider the appropriateness and cost of performing all three serological tests when conducting community screening among foreign born Asian Americans. A high prevalence (10%) of Asian Americans in our study lacked detectable HBsAg and yet still had been exposed to HBV infection, as indicated by positive anti-HBc. Studies are urgently needed to clarify the prevalence of viraemia (e.g., HBV DNA) among HBsAg negative, anti-HBc positive cases and to evaluate the infectivity of blood components. The study findings suggest a more aggressive HBV screening test is needed for all age groups. As the number of immigrants from Asia grows, it is important to recognize the HBV prevalence and HBV exposure among foreign-born Asian Americans, and to deploy early detection and follow-up efforts to treat chronic HBV infection in order to reduce liver cancer disparities caused by HBV infection.