1. Context
Esophageal varices (EVs), submucosal venous dilations in the lower esophagus, typically develop as a consequence of portal hypertension, most commonly resulting from liver cirrhosis (LC) (1-3). Among the LC-related complications, gastroesophageal varices (GEV) rupture is the most frequent and life-threatening event. The significant variceal hemorrhage-related morbidity and fatality highlight the critical importance of precise diagnosis and appropriate therapeutic interventions (4, 5). Esophagogastroduodenoscopy (EGD) represents the gold standard for diagnosing and assessing the risk of gastroesophageal variceal bleeding (VB) (6). Nonetheless, a significant proportion of patients with LC who undergo EGD screening are found to have either no EVs or only small ones (7). This suggests that routine endoscopic screening for EVs may be a procedure that could be postponed in certain cases, as it poses potential risks to patients and contributes to increased healthcare costs. Early identification of high-risk patients is crucial to improving outcomes and optimizing medical resources (8).
Recently, artificial intelligence (AI) and machine learning (ML) have made significant progress in medical image analysis, risk prediction, and clinical decision support. Machine learning is a subset of AI. The ML specifically involves systems that can learn from and make decisions based on data. In the context of esophageal varices and LC research, ML techniques like deep learning can be used to analyze medical images or patient data to identify patterns and predict outcomes, which is part of the AI-driven approach to improve diagnosis and treatment. These advancements offer new tools and methods for managing LC and its complications, thereby enhancing diagnostic accuracy and streamlining clinical workflows.
2. Evidence Acquisition
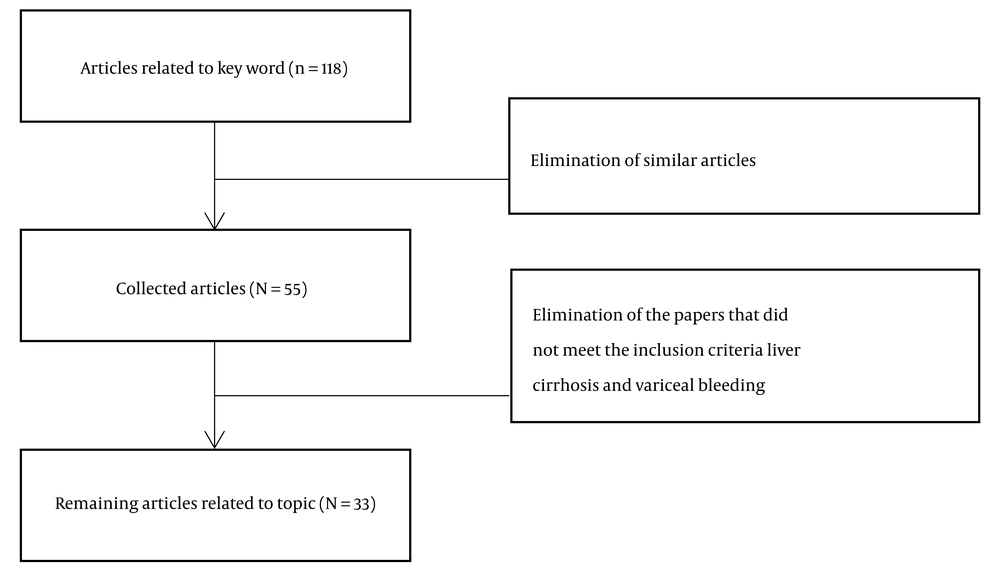
This paper was considered a review of AI in managing LC and its complications, particularly esophageal variceal bleeding (EVB). The review included an electronic search in PubMed and MEDLINE, using the terms "artificial intelligence", "machine learning", "liver cirrhosis", and "esophageal varices or variceal bleeding". Based on the three search queries: (Esophageal varices) AND (machine learning), (esophageal varices) AND (artificial intelligence), and ((liver cirrhosis) AND (varices)) AND (artificial intelligence), a total of 118 articles were identified. This review considered both original and review types. Initially, articles were screened using their titles and abstracts, followed by a comprehensive full-text analysis. The selection process adhered to specific inclusion criteria, which required the articles to be original research, published in English within the last decade (2014 - 2024), and focused on studies involving human subjects. The exclusion criteria removed irrelevant studies, leaving 33 articles focused on esophageal varices (including those related to liver cirrhosis) and AI (including machine learning) (Figure 1).
3. Results
3.1. Limitations of Current Predictive Models and Scoring Systems of Esophageal Varices and Gastric Varices
Although LC severity is evaluated using current scoring systems, such as the Child-Pugh (CP) score and the model for end-stage liver disease (MELD) (9), they do not specifically focus on assessing the mortality risk in patients with upper gastrointestinal bleeding (UGIB), particularly in emergency settings. This limitation restricts the potential for early intervention, thereby reducing the effectiveness of timely clinical management and the improvement of patient outcomes during acute bleeding episodes. Radiomics has been employed in diagnosing LC and predicting related complications (10). Nevertheless, most recent studies predict EVB risk based on single-level image features, resulting in incomplete data. Additionally, direct measurement of the portal pressure gradient (PPG), a critical factor in determining the risk of EVB and refractory complications, is invasive and not frequently used in clinical settings (11), highlighting the urgency for developing non-invasive techniques to determine PPG accurately.
Risk stratification for predicting the first VB episode in patients with compensated advanced chronic liver disease (cACLD) is currently limited (12). Frequently, patients with chronic liver disease (CLD) develop thrombocytopenia (TCP), with severe cases (platelet count < 50 × 109/L) increasing morbidity and complicating management, further escalating the bleeding risk through invasive procedures. This emphasizes the need for improved risk stratification and non-invasive diagnostic tools to enhance patient outcomes.
3.2. Detection and Risk Assessment of Esophageal Varices and Gastric Varices
3.2.1. Artificial Intelligence and Machine Learning in Endoscopic Image Analysis
Recent studies have demonstrated the high precision of deep learning (DL) and AI systems in detecting and grading GEV and predicting VB risk in patients with LC. A multi-center retrospective study (6) highlights the remarkable capabilities of deep convolutional neural networks (DCNN) in detecting EVs and gastric varices (GVs), as well as revealing endoscopic risk factors for gastroesophageal VB. The ENDOANGEL system, after extensive image training, achieved accuracies of 97.00% and 92.00% in EV and GV detection, respectively. It also performed well in determining size, shape, color, bleeding signs, and treatment suggestions.
Building on these findings, another study developed an AI system named ENDOANGEL-GEV (13) for segmenting, grading (grades 1 - 3), and classifying red color signs (RC0-RC3) of GEV in cirrhotic patients. Trained and validated across three datasets, ENDOANGEL-GEV demonstrated high accuracy and consistency. When combined with the CP score for risk stratification, ENDOANGEL-GEV outperformed endoscopists in detecting EVs and showed comparable performance for GV.
Furthermore, a retrospective cohort study (1) explored the use of DL in the prediction of the 12-month risk of EVB in cirrhotic patients using endoscopic images. Among the six trained and validated DL models, EfficientNet achieved the highest accuracy (0.910 in validation and 0.893 in test datasets), outperforming two endoscopists (accuracies of 0.800 and 0.763). Notably, AI assistance improved endoscopists' accuracy by 17.3% and 19.0%. The study highlights the potential of DL and AI-aided diagnosis as valuable tools in managing LC and predicting EVB risk.
In addition, a study (4) first evaluated automated multimodal ML feasibility for predicting 12-month EVB by integrating endoscopic images and clinical variables. The EfficientNet model demonstrated the highest accuracy in the validation set, and a stacking model showed superior performance in the test dataset.
In patients with hepatocellular carcinoma (HCC), the EVendo score (14) was introduced as a non-invasive tool to predict EV and varices needing treatment (VNT). A retrospective multi-center cohort study included 112 HCC patients with 117 qualifying EGDs, with the EVendo score revealing a sensitivity and a negative predictive value of 97.4% and 96.9%, respectively, for predicting VNT. These findings suggest that the EVendo score could enable the safe deferral of approximately 30% of EGDs for EV screening in this population, thereby reducing healthcare costs and minimizing delays in commencing atezolizumab and bevacizumab treatment.
Overall, these emerging technologies can enhance diagnostic accuracy, reduce healthcare costs, and improve treatment outcomes by safely deferring unnecessary procedures and aiding in early intervention.
3.2.2. Predictive Models Based on Artificial Intelligence and Machine Learning Technologies
Recent studies have highlighted the ability of AI and machine learning models (MLM) to transform EV management in patients with LC. These technologies have demonstrated the ability to enhance diagnostic accuracy, predict bleeding risks, and provide non-invasive alternatives to traditional methods such as EGD. For instance, an Indian study (12) utilized an XGBoost algorithm to predict VB risk in patients with cACLD. This approach significantly enhanced endoscopic stratification performance. Similarly, the EVendo score (7), a readily available clinical data-based scoring system, was developed and validated to predict EV and varices needing treatment (VNT) presence in cirrhotic patients. This score has the potential to help low-risk patients avoid unnecessary EGDs, thereby reducing healthcare costs and patient risks.
Furthermore, an MLM (15) was tested for the prediction of short- and long-term survival in cirrhotic patients. Unlike traditional scoring systems, such as the MELD-serum sodium (MELD-Na) and Child-Turcotte-Pugh (CTP) scores, the MLM demonstrated superior prediction accuracy. It achieved mean area under the curve (AUC) values of 0.87, 0.85, and 0.76 for 1-, 3-, and 12-month survival, respectively, across the entire study population. In patients with VB, the model achieved AUC values of 0.91 for 1-month, 0.88 for 3-month, and 0.91 for 12-month survival. The study concluded that the MLM outperformed traditional scoring systems in predicting survival and identifying high-risk VB.
Another example is the artificial neural network (ANN) model (2) developed to estimate the 1-year risk of esophagogastric variceal bleeding (EGVB) in patients with LC. The model identified 12 independent risk factors: Gender, decompensation, drinking/smoking history, varices location and size, ascites, alanine aminotransferase, γ-glutamyl transferase, hematocrit, neutrophil-to-lymphocyte ratio, and red blood cell count. The ANN model achieved an AUC of 0.959, significantly superior relative to the AUCs for the North Italian Endoscopic Club (NIEC) and revised NIEC indices (0.669 and 0.725, respectively). Decision curve analyses showcased the enhanced ANN model's net benefits, unlike the NIEC and Rev-NIEC indices, suggesting its precise ability to predict the 1-year risk of EGVB and inform risk-based surveillance strategies.
In addition, a review of 12 studies (8) using various MLMs to predict bleeding risks and grading EV in LC patients manifested high predictive accuracy, with some models yielding AUC values above 99%. These findings highlight the transformative capability of AI in treating EVs in LC. A multi-center retrospective study (16) further identified risk factors for early rebleeding following endoscopic variceal ligation (EVL). The study highlighted the predictive potential of CP grade C, Japanese variceal grade F3, and esophageal variceal diameter (EVD). This underscores the importance of integrating clinical data with AI-based predictive models.
Overall, AI-based systems, especially ML and DL, have shown promise in improving risk stratification and diagnosis by analyzing laboratory data, clinical scores, endoscopic images, and imaging modalities. While these technologies have significant potential to enhance diagnosis, risk evaluation, and treatment approaches for EVs, they should be used to complement traditional methods (3). Further studies are required to enhance these technologies and confirm their clinical efficacy through rigorous validation.
3.2.3. Artificial Intelligence and Machine Learning technologies and Electronic Health Records
The significant potential of AI and ML, in conjunction with electronic health records (EHRs), has been underscored to enhance CLD and LC management. These advancements offer new avenues for improving diagnostic accuracy, predicting complications, and optimizing treatment strategies. For instance, a study from Spain (17) employed natural language processing (NLP), ML, and SNOMED-CT terminology to analyze free-text information from EHRs. This innovative approach enabled the extraction of data to assess the connection between invasive procedures, bleeding events, and prophylactic treatments in patients with CLD. By leveraging the rich, unstructured data within EHRs, this study demonstrated the potential of AI to uncover critical insights that may not be apparent through traditional data analysis methods.
Another retrospective observational cohort study (18) utilized EHRs from the TriNetX Network to ascertain liver-correlated outcomes in patients with LC and diagnosed/suspected portal hypertension. The study identified three distinct patient groups based on disease severity and meticulously analyzed outcomes such as variceal hemorrhage, hepatic encephalopathy, ascites complications, and mortality over a 24-month period. Notably, the most severe group exhibited the highest incidence of variceal hemorrhage and composite outcomes, with a cumulative incidence of 59% at 6 months. These findings highlight the importance of stratifying patients based on disease severity to better predict and manage complications.
In a related vein, another study (9) analyzed EHRs spanning from 2001 to 2019, encompassing 16,025 patients with LC and 32,826 emergency department (ED) visits for UGIB. Three ML models were rigorously evaluated, with the XGBoost (XGB) model emerging as the most effective in the prediction of in-hospital and ED mortalities. Key predictors identified by the model included international normalized ratio, red blood cell distribution width, white blood cell count, renal function, and age. These results suggest that ML models, particularly the XGB model, can effectively predict mortality in this high-risk patient group, potentially aiding early intervention and improving outcomes.
Collectively, these findings underscore the transformative capability of AI and ML in improving early intervention and outcomes in high-risk patient groups with CLD and LC. By harnessing the vast and complex data within EHRs, these technologies offer new opportunities to strengthen clinical decision-making, optimize resource allocation, and eventually improve patient care.
3.3. Diagnosis and Staging of Liver Fibrosis and Liver Cirrhosis
3.3.1. Diagnostic Models Based on Imaging
Recent studies have underscored the potential of imaging-based diagnostic models to significantly enhance the management of liver diseases, offering improved diagnostic accuracy and clinical decision-making. In Singapore, an innovative computer-aided diagnosis tool was developed for detecting and classifying liver fibrosis (LF) stages using conventional B-mode ultrasound images (19). By combining kernel discriminant analysis (KDA) and ANOVA, this tool achieved impressive accuracy (91.46%), sensitivity (92.16%), and specificity (88.92%) in classifying the five stages of LF. This approach demonstrates how widely available imaging modalities can be leveraged to provide precise, non-invasive assessments. The evaluation was done on a database of 762 ultrasound images, though the small sample size can limit the robustness and generalizability of the models.
Another study introduced the liver-spleen (LS) MLM, which uses contrast-enhanced CT to anticipate intervention or death risk in cirrhotic patients with acute variceal bleeding (AVB) (20). The LS model achieved AUC values of 0.782 and 0.789 in internal and external tests, respectively, outperforming traditional clinical scores. This highlights the model's ability to improve clinical decision-making in managing AVB.
Similarly, a study developed MLMs that integrate CT morphology features, serum biomarkers, and physical conditions to predict EVB in cirrhotic patients (21). Among these models, random forest and adaptive boosting showed the highest accuracy, with AUC values reaching 0.854 and 0.818 in training and testing. These results emphasize the value of combining multimodal data to enhance predictive capabilities.
Overall, these advancements illustrate how imaging-based models can transform liver disease management. By integrating advanced imaging techniques with ML, these studies pave the way for more precise and personalized approaches to patient care.
3.3.2. Integrating Radiomics and Clinical Features
Recent studies have shown the potential of combining radiomics and clinical features to improve EVB prediction in patients with LC. A study (10) developed a radiomics-clinical model (RC model) to predict the risk of first-instance secondary EVB in cirrhotic patients using clinical data and multi-organ radiomic features from the liver, spleen, and lower esophagus-gastric fundus region. The RC model achieved high predictive accuracy with AUC values of 0.951 in the training cohort and 0.930 in the validation cohort, outperforming individual radiomic and clinical models.
An imaging-based MLM (20) was developed and validated based on contrast-enhanced CT to predict the composite clinical endpoint risk (hospital-based intervention or death) in LC patients with AVB. The LS model displayed superior diagnostic performance compared to traditional clinical scores.
A study (22) developed a non-invasive EVB prediction model using radiomics based on CT in 317 cirrhotic patients. The integrated model combining radiomics, CT, and clinical attributes yielded AUCs of 0.89 and 0.78 in the training and validation sets, implying the potential for early variceal bleeding risk prediction.
A study (23) developed a radiomic model (RM) using ML to diagnose high bleeding risk esophageal varices (HREV) in cirrhotic patients via CT images. The model showed high accuracy with area under the receiver operating characteristic (AUROC) values up to 0.983 in training and 0.736 in external validation, outperforming Baveno VI criteria.
These models highlight the potential of integrating radiomics and clinical attributes to promote diagnostic accuracy and clinical decision-making in the management of LC-related complications.
3.4. Prediction of Prognosis and Complications in Patients with Liver Cirrhosis
3.4.1. Prognostic Model Establishment and Validation
Recent studies have explored the establishment and validation of prognostic models using AI and ML to predict clinical outcomes in patients with LC and related complications. A dual-center retrospective study (24) used AI to verify and compare the prognostic performance of the albumin-bilirubin, platelet-albumin-bilirubin, and CP grades alongside the MELD score in predicting the 1-year variceal rebleeding possibility in patients with LC and VB undergoing early transjugular intrahepatic portosystemic shunt (TIPS) procedures, finding none of the variables optimal. The LC severity might not be fully represented by these variables, limiting their predictive power for this specific outcome.
A retrospective study (25) established prognostic models to predict 3-month overt hepatic encephalopathy occurrence, 1-year mortality, and liver malfunction for LC patients with AVB treated with early TIPS creation, showing the potential of ANN and nomogram models for accurate prediction. However, single-center retrospective training cohorts may have limitations such as selection bias, limited data diversity, and lack of external validation, which can affect the generalizability and robustness of the model's predictions.
A MLM (15) was used to ascertain model feasibility to predict short- and long-term survival of patients at distinct LC stages, showing high AUC values in predicting survival at 1, 3, and 12 months in patients with VB. Another study (26) investigated the correlation between EVD and PPG, suggesting EVD as a possible non-invasive PPG indicator. Moreover, the receiver operating characteristic (ROC) curve demonstrated EVD's high accuracy in diagnosing PPG function.
A study (27) evaluated the effectiveness of various AI techniques in predicting readmission and death in LC patients using data gathered at admission, during hospitalization, and at discharge. The NACSELD cohort included 2,170 patients with a mean age of 57 years, MELD score of 18, and a 90-day mortality rate of 13%. The AI models, including logistic regression, kernel support vector machine (SVM), and random forest classifiers, achieved AUC values of 0.57 - 0.72. Despite using multiple AI techniques, it is difficult to predict 30- and 90-day readmissions and death in cirrhosis. This difficulty underscores the complexity of cirrhosis and its outcomes, which may be influenced by a multitude of factors that are hard to capture comprehensively in AI models.
A study (28) developed and validated the "ABCAP" score, incorporating easily obtained clinical variables, to predict 30-day in-hospital mortality in older patients with UGIB, demonstrating superior or comparable performance to the AIMS65 score and showing promise for effective risk stratification.
3.4.2. Prediction of Specific Complications
Recent advancements in the prediction of specific complications in liver disease have leveraged non-invasive DL models and MLMs to enhance diagnostic accuracy and risk stratification. A non-invasive DL model (11) retrospectively analyzed data to develop an ANN model for predicting PPG, with a three-parameter (3P) model achieving high accuracy and effectively distinguishing high-risk portal hypertension.
Moreover, DL (29) was developed to create an index that integrates liver and spleen volumes with clinical factors for identifying high-risk varices in patients with B-viral compensated LC. The study found that the spleen volume-to-platelet ratio was particularly useful in detecting high-risk varices and evaluating bleeding risk. In LC patients (2), an ANN model that precisely predicted the 1-year risk for EGVB was established, potentially representing a cornerstone for risk-based surveillance approaches.
The PSC risk estimate tool (30) (PREsTo) used gradient boosting to predict hepatic decompensation in primary sclerosing cholangitis (PSC). Derived from 509 patients and validated in 278, PREsTo includes nine variables and achieved a C-statistic of 0.90, outperforming the MELD, Mayo PSC risk score, and SAP < 1.5 × ULN. It remained accurate in patients with bilirubin < 2.0 mg/dL and at later disease stages. PREsTo offers a superior non-invasive prognostic tool for PSC management.
A study (31) used Danish health registry data (1996 - 2014) to identify early-stage alcoholic-related liver disease (ALD) through ML techniques. ALD progresses from fatty liver to steatohepatitis, fibrosis (ALF), and cirrhosis (ALC), with most patients diagnosed at the decompensated LC stage. The study found that ALC was the most frequent form of ALD, with strong associations with liver dysfunction. The MLMs (support vector machine [SVM], random forest [RF], LightGBM, Naive Bayes) achieved high classification performance for ALC (AUC = 0.89) but lower performance for ALF (AUC = 0.67 for Naive Bayes). Identified comorbidities accurately detected ALC and showed promise in predicting ALF.
A study (32) developed a non-invasive machine-learning approach using spleen stiffness, liver stiffness, and heart rate changes to predict response to non-selective beta-blockers in cirrhotic patients with high-risk varices, achieving high accuracy and specificity.
3.5. Comprehensive Application and Future Prospects of Artificial Intelligence in Managing Liver Cirrhosis
3.5.1. Integration of Multimodal Data
A comprehensive methodological analysis (8) reviewed the applicability of diverse MLMs in predicting bleeding risks and grading EV in patients with LC, highlighting their high predictive accuracy. A study using AI (33) compared the accuracy of virtual reality (VR) and endoscopic variceal measurement in measuring the EVD, suggesting VR as a valuable tool for endoscopic detection and treatment of EVs in patients with LC.
3.5.2. Future Directions and Challenges
The review on AI in diagnostics and prognosis provides a broad overview of AI's transformative impact. However, it is essential to address potential biases in AI models, especially those arising from dataset limitations, as they can affect reliability and fairness, leading to skewed results and inequitable healthcare outcomes. These biases often stem from non-representative datasets that do not fully capture patient diversity or clinical scenarios. Furthermore, the lack of interpretability in many AI models, especially deep learning ones, can exacerbate the challenges posed by biased datasets. Their "black-box" nature makes it difficult for healthcare providers to understand decision-making, risking improper treatment decisions.
The role of AI (3) in enhancing EV management should focus on its applications in diagnosis, risk stratification, and treatment optimization. Despite advancements, clinical scores based on laboratory data still show low specificity, often requiring confirmatory endoscopic or imaging studies. Other studies (1, 34) mentioned the potential value of AI-aided diagnosis in LC management, noting challenges such as model validation and optimization.
4. Conclusions
In conclusion, AI and ML offer significant potential in managing LC and its complications, from endoscopic image analysis to prognostic prediction and from single-modality imaging to multimodal data integration. Studies have shown that DCNN perform with high precision in endoscopic image analysis, effectively detecting EVs and GVs and revealing risk factors for bleeding. Furthermore, predictive models based on ML, such as XGBoost and ANN, have shown significant advantages in predicting VB risk, mortality in patients with LC, and the occurrence of complications. The NLP techniques combined with EHRs provide a new perspective for evaluating patient treatments and bleeding events.
Despite significant progress, current clinical scoring systems still have deficiencies in specificity, requiring further research and validation. These technologies are gradually changing traditional diagnostic and treatment patterns, providing more precise and personalized decision support for clinical practice. However, further large-scale validation and optimization are needed to ensure the reliability and generalizability of these models. Further research should focus on validating and refining these models, as well as developing non-invasive methods for evaluating PPG and other critical parameters. While current scoring systems and diagnostic procedures have limitations, the development of ML models and non-invasive techniques offers promising opportunities to enhance patient outcomes and optimize the utilization of medical resources.