1. Background
Hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) infections constitute serious healthcare problems and infect millions of people around the world. HBV and HCV infections can result in chronic liver diseases, including cirrhosis and hepatocellular carcinoma, while HIV infection can result in severe opportunistic diseases (1).
Illegal drug use has become an increasingly major problem in Afghanistan due to widespread armed conflict resulting in extensive internal and external displacement and social and economic upheavals since 2001 (2). The population of Kabul, the capital of Afghanistan, has increased to approximately 3 million since 2001 because of returning refugees (3, 4). External displacement is significant, particularly in refugee populations moving to neighboring countries, including Iran and Pakistan. Both countries harbor higher drug user populations and higher prevalence of HBV, HCV, and HIV among people who use drugs (PWUD), especially people who inject drugs (PWID) (5-7). As a result, when the populations return to Afghanistan, they spread illegal drug use to others.
Estimates say that about 1.6 million Afghans are PWUD, fostered by readily available opium and heroin and most of them are men. The Afghan government has space for only about 2,300 of them in its drug treatment facilities around the country and Kabul harbors a large number of PWUD. At these treatment facilities, in addition to stopping drug abuse, the goal of the treatment is to return people to productive lives in their family, workplace, and community. During their 3 - 6-month treatment, the patients receive medication therapy, counselling, and psychotherapy (8).
Most of the PWUD in Kabul live collectively in open areas without any shelters. This lifestyle increases their risky behaviors such as poor hygiene, close contact, shared needles, skin popping, and unsafe extra-marital sexual contact, and not only exposes them to transmissible infections such as HBV, HCV, and HIV, but also makes them the main source of transmission of such viral infections to other people. These observations raised concerns that PWUD and accompanying high-risk behaviors are increasing in Afghanistan and the risk of HBV, HCV, and HIV epidemic would have the potential to be high in the future (9, 10). Additionally, a study carried out on chronic intranasal users of the drug in the USA showed that it has implications for potential transmission of HCV via contact with contaminated nasal secretions (11), which is also common among PWUD in Kabul. The PWUD are a potential source of infection and may represent a serious threat to the community. Therefore, it is extremely important to identify and track infected persons in order to prevent further transmission of these infections by preventive measures and appropriate controls. There are no major differences between in-treatment and out of treatment PWUD in terms of risky behaviors and sociodemographic characteristics in Kabul. However, out of treatment PWUD may differ in terms of continuous contact with infected persons and the prevalence of viral infections (10).
A recent survey conducted by Afghanistan National AIDS Control Program (NACP) in 2012 revealed 12,541 PWUD were living in Kabul. Unsafe injection drug use, including shared needles and other injecting equipment, is considered the key route of HIV, HBV and HCV transmission in Afghanistan. Based on available data, the HIV epidemic in Afghanistan seems to be low and HIV affects mainly PWUD, and are among a key population at higher risk of contracting HIV (12). In a study from 2005 to 2010 covering 1,696 PWUD from some provinces of Afghanistan such as Kabul showed a range of 36.0% - 36.6% seroprevalence of HCV and 5.8% - 6.5% hepatitis B surface antigen (HBsAg) positive (13, 14).
2. Objectives
Little data are available on hepatitis B, hepatitis C, and HIV prevalence, and associated risk behaviors among PWUD who use different methods or a combination of drug use methods in Afghanistan, especially in Kabul. The primary objective of this study was to determine the prevalence of HIV, HBV, and HCV infections among PWUD treated at health facilities of Kabul and to identify the associated risk factors and behaviors that make them exposed to these infections. The impact of this study will be to inform policymakers and program managers at the Ministry of Public Health of Afghanistan and related stakeholders about HBV, HCV, and HIV infection rates among PWUD and the associated risky behaviors in Kabul. In addition, this study might prove useful for developing proper treatment and prevention guidelines and future educational programs.
3. Methods
3.1. Subjects
The current cross-sectional study was conducted in 7 main public and private healthcare facilities treating PWUD from May 2016 to October 2016 in Kabul, Afghanistan. These centers provide social support and medical care for PWUD. Four hundred and ten male users of drug treated at these healthcare facilities were included in this study. Users of drugs are almost male in Kabul and Afghanistan and no female users were referred to these health facilities during the time of the study. The eligible participants were all the PWUDs admitted to these health facilities, with no previous vaccination against HBV (while there is no effective vaccine against HCV and HIV) and were able to provide informed consent. Before data collection, this study was approved by the Research Committee of Kabul University and the Academic Council of the Ministry of Higher Education of Afghanistan, as well as the Ministry of Public Health of Afghanistan. The participants were interviewed, using a questionnaire that included sociodemographic, travel or displacement histories, the past and current drug use, method of drug use, history of blood transfusion, and unsafe extra-marital sexual behaviors.
3.2. Serological Analysis
Five mL of the blood sample was collected from each participant and was centrifuged at 5000 RPM for five minutes at the microbiology laboratory of the Faculty of Pharmacy of Kabul University in order to isolate plasma for serological tests.
First rapid immunochromatographic tests (ICT) for HBsAg (Standard Diagnostics Inc. Korea), anti-HCV (SD, Korea), and anti-HIV-1/HIV-2 (SD, Korea) were performed with 100% sensitivity and 99.5% specificity as mentioned by the manufacturer. For diagnostic accuracy, all samples identified positive by ICT were confirmed by ELISA Kits (General Biologicals Corporation, Kaohsiung, Taiwan). The patients who were diagnosed seropositive for HBV, HCV, or HIV were referred for further investigation and treatment.
3.3. Statistical Analysis
The overall prevalence of viral infections among PWUD was calculated with a 95% confidence interval (CI) with descriptive analysis, reported in numbers and percentages. The chi-square test was used to evaluate the prevalence of viral infections (HIV, HBV, and HCV) among those of various ages, marital status, and economic status, and duration, method of drug use, previous prison residence, and unsafe extra-marital sexual contact. The crude odds ratios (OR) were estimated by univariate analysis to observe the association of each variable with viral infection. The adjusted OR was generated to determine the independent contribution of risk factors to viral infection, using multivariate logistic regression models. All statistical tests were two-tailed and a level of P < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 19 (SPSS Inc, Chicago, IL, USA) software.
4. Results
All 410 PWUD were male aged between 18 - 65 years (mean 31.5, median 30.0); 212 (51.7%) aged between 18 - 30, 144 (35.1%) aged between 31 - 40, and 54 (13.2%) aged between 41 - 65 years old. Among them, 55 (13.4%) were PWID and 355 (86.6%) were non-injection users of drugs (smoking, eating, sniffing, and chewing). Their past history of addiction ranged from 73 days to 30 years (mean 7.2 years, median 6 years), and 277 of them (67.6%) were in a lower economic status (income less than 200 USD per month to feed themselves and their family). Among them, 156 (38%) were single, 252 (61.5%) married, and 2 (0.5%) were divorced. Also, 219 (53.4%) of them were illiterate, 154 (37.6%) had primary level education, and 25 (6.1%) had secondary education, and 12 (2.9%) had higher education. Among them, 303 (73.9%) were jobless before consuming drugs and after drug addiction, all of them had lost their job. Moreover, 352 of the participants (85.9%) were using heroin, 31 (7.6%) were using methamphetamine crystals, 26 (6.3%) were using opium, and 1 (0.2%) was using marihuana. In addition, 236 (57.6%) of them have started drug use in Afghanistan, 159 (38.8%) of them have started drug use in Iran, and 15 (3.7%) of them have started drug use in other countries such as; Pakistan, countries to the North of Afghanistan and even Europe. Further sociodemographic details and other information about study participants are described in Table 1.
| Variable | Values, No. (%) |
|---|---|
| Age | |
| 18 - 30 | 212 (51.7) |
| 31 - 40 | 144 (35.1) |
| 40 - 65 | 54 (13.2) |
| Marital status | |
| Single | 156 (38.0) |
| Married | 252 (61.5) |
| Divorced | 2 (0.5) |
| Education | |
| Illiterate | 219 (53.4) |
| Primary | 154 (37.6) |
| High school | 25 (6.1) |
| Higher education | 12 (2.9) |
| Duration of drug use, year | |
| < 1 | 43 (10.5) |
| 1 - 5 | 141 (34.4) |
| > 5 | 226 (55.1) |
| Drug | |
| Heroin | 352 (85.9) |
| Crystal methamphetamine | 31 (7.6) |
| Opium | 26 (6.3) |
| Method of use | |
| Injection | 25 (6.1) |
| Smoke | 350 (85.4) |
| Other methods | 5 (1.2) |
| Injection + other methods | 30 (7.3) |
| Transfusion | |
| Yes | 12 (2.9) |
| No | 398 (97.1) |
| Reason of using drug | |
| Friendship | 369 (90) |
| Social problems | 4 (1) |
| Medical problems | 37 (9) |
| Country of starting drug use | |
| Afghanistan | 236 (57.6) |
| Iran | 159 (38.8) |
| Other countries | 15 (3.7) |
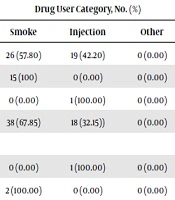
Fifteen PWUD (3.7%, 95% CI 1.8 - 5.5) were HBsAg positive, forty-five (11.0%, 95% CI 7.9 - 14.0) were anti-HCV positive and one anti-HIV positive (0.2%, 95% CI -0.2 - 0.7); one person was co-infected with HIV and HCV (0.2%, 95% CI -0.2 - 0.7) and two persons were co-infected with HCV and HBV (0.5%, 95% CI -0.2 - 1.2). Further details are summarized in Table 2.
| Virus | Situation | Drug User Category, No. (%) | Total, No. (%) | ||
|---|---|---|---|---|---|
| Smoke | Injection | Other | |||
| HCV | Positive | 26 (57.80) | 19 (42.20) | 0 (0.00) | 45 (100.00) |
| HBV | Positive | 15 (100) | 0 (0.00) | 0 (0.00) | 15 (100.00) |
| HIV | Positive | 0 (0.00) | 1 (100.00) | 0 (0.00) | 1 (100.00) |
| Viral infection (Either HIV, HBV or HCV) | positive | 38 (67.85) | 18 (32.15)) | 0 (0.00) | 56 (100.00) |
| Co-infection | |||||
| HIV + HCV | Positive | 0 (0.00) | 1 (100.00) | 0 (0.00) | 1 (100.00) |
| HCV + HBV | Positive | 2 (100.00) | 0 (0.00) | 0 (0.00) | 2 (100.00) |
In univariate and multivariate analysis of HIV and HBV, we did not find any significant association between different variables and HIV, HBV infection among infected and uninfected persons. Owing to that the number of HCV infected persons was higher, we performed a multivariate analysis and adjusted for other variables. We found that shared needles and the use of drugs by injection independently associated with HCV infection (OR = 5.40, CI: 2.60 - 11.23). Due to the small number of HIV and HBV infections, we could not separately calculate risk factors for these infections.
Finally, we analyzed the associated risk factors for viral infection (HIV, HBV, and HCV infection). By univariate analysis, the use of drugs by injection, history of unsafe extra-marital sexual contact, the history of prison was significantly associated with viral infection, but in multivariate analysis, the use of drugs by injection remained significantly associated with viral infection, which is mostly related to HCV infection (OR= 3.57, CI: 1.76 - 7.24). Further details are summarized in Table 3.
| Variable | Univariate OR, CI (95%) | P Value | Multivariate OR, CI (95%) | P Value |
|---|---|---|---|---|
| Age | ||||
| 18 - 30 | 1.0 | |||
| 31 - 40 | 1.64 (0.89 - 3.01) | 0.10 | ||
| > 40 | 1.16 (0.47 - 2.87) | 0.73 | ||
| Marital status | ||||
| Single | 1.0 | |||
| Married | 0.84 (0.47 - 1.50) | 0.56 | ||
| Divorced | 5.78 (0.35 - 95.75) | 0.22 | ||
| Economic status | ||||
| Lowera | 1.0 | 0.11 | ||
| Middleb | 0.59 (0.30 - 1.13) | |||
| Duration of use | 1.022 (0.97 - 1.07) | 0.38 | ||
| Method of use | ||||
| Smoke | 1.0 | |||
| Injection | 3.99 (2.07 - 7.69) | < 0.01 | 3.57 (1.76 - 7.24) | < 0.01 |
| Other methods | 0.00 | 0.99 | ||
| Previous prison | ||||
| No | 1.0 | |||
| Yes | 1.84 (1.00 - 3.39) | 0.05 | ||
| Unsafe extra-marital sexual contact | ||||
| No | 1.0 | |||
| Yes | 2.03 (1.15 - 3.60) | < 0.01 | 1.78 | 0.06 |
aIncome between 200 - 500 USD per month.
bIncome less than 200 USD per month.
As injection drug use is already a known risk factor for HIV, HBV, and HCV infections, we analyzed some factors that may predict injection drug use as well. In the univariate analysis, joblessness, location of starting drug use in Iran and other countries, previous prison and starting drug use with a duration of two years or more were significantly associated with injection drug use. After multivariate analysis, joblessness, location of starting drug use in other countries, and previous prison remained significantly associated with injection drug use. Further details are summarized in Table 4.
| Variable | Univariate OR, CI (95%) | P Value | Multivariate OR, CI (95%) | P Value |
|---|---|---|---|---|
| Occupation | ||||
| Employed | 1.0 | |||
| Jobless | 2.27 (1.04 - 4.98) | 0.04 | 2.92 (1.20 - 7.11) | 0.02 |
| Place of starting drug use | ||||
| Afghanistan | 1.0 | |||
| Iran | 2.21 (1.19 - 4.10) | 0.01 | 1.27 (0.63 - 2.56) | 0.50 |
| Othera | 12.34 (4.06 - 37.57) | < 0.01 | 7.46 (1.99 - 28.03) | < 0.01 |
| Previous prison | ||||
| No | 1.0 | |||
| Yes | 4.79 (2.65 - 8.67) | < 0.01 | 3.57 (1.85 - 6.86) | < 0.01 |
| Duration of drug use, y | ||||
| < 2 | 1.0 | |||
| 2 - 10 | 4.53 (1.36 - 15.11) | 0.01 | ||
| > 10 | 4.67 (1.29 - 16.92) | 0.02 |
aPakistan, countries to the north of Afghanistan, and even Europe.
5. Discussion
In this study, among PWUD in Kabul, 189 (42.4%) of them have started drug use outside Afghanistan, especially Iran (38.8%). This highlights the role of external displacement and as a result bringing this habit back to Afghanistan. The remaining 236 (57.6%) have started drug use in Afghanistan, which shows a great danger of becoming a drug addict in the country nowadays. All subjects of the study population were male because almost drug addicts are male in Afghanistan and it was not possible to compare females with males in this regard.
There was just one case of HIV infection by detection of anti-HIV antibody, but this finding is not representative of PWUD living in Kabul without shelter. Other vulnerable population groups and those having risky healthy behaviors were also not included in this study and may harbor higher prevalence of HIV than the study group; however, this is consistent with the World Health Organization’s latest report on HIV (15). It can be concluded that Afghanistan is in the early stage of an HIV epidemic and the main route of transmission remains shared needle among PWID. On the other hand, this study was conducted on drug user populations referred to hospitals by their families or by themselves. While the prevalence of risk factors, especially shared needles among PWID living on the streets or under bridges crossing Kabul River, in very bad hygienic conditions, is higher and the prevalence of viral infections among them could be higher too, which is not reflected in this study.
In the current study, 3.7% were HBsAg and all of them were using drugs by smoking. This finding may indicate the role of other risk factors other than PWID; however, owing to a small number of positive HBV cases in our study, we could not conclude smoking as a specific risk factor. Moreover, 11% were anti-HCV positive and this was seen both among PWID and non-injecting drug users, this finding potentially anticipates that HCV transmission and incidence among PWUD may increase in the near future and also could be the main source of HCV transmission to other people. In a review article concerning the prevalence of HBV and HCV among all available Afghanistan populations (2), the prevalence of HBV was 1.9% and HCV was 1.1%. Our findings suggest that the prevalence of HBV and especially HCV is ten times higher among PWUDs than the general population.
Among risk factors, injection drug use was related to viral infection and mostly for HCV infection, which is a known risk factor for HCV transmission (16). This finding is similar to a study conducted in Kashan, Iran (17). The results of this study showed no association of HBV and HCV infection with age, economical condition, unsafe extra-marital sexual contact, previous prison, and the duration of drug use; however, shared needles were significantly associated with HCV infection.
In our study, the associated factors for injection drug use that promoted viral transmission and infection included; joblessness, previous prison, and the location of starting drug use in other countries, remained significant. This study is worthwhile for the Ministry of Public Health of Afghanistan and related stakeholders. This study has some strengths and limitations. This was the first study among PWUD admitted in different Kabul health facilities, with the purpose to interview and collect blood samples from a considerable number of the PWUD that can represent all PWUD under treatment and social support. One of the limitations of this study was the lack of information about the history of injection use or shared syringe among PWUDs; also we could not interview and collect blood samples from drug user living without shelters on streets and under bridges in very bad hygienic conditions.
5.1. Conclusions
Our study showed that the prevalence of HCV and HBV are higher among PWUD in Kabul than the normal population and the rate of HIV infection is lower among them. The use of drugs by injection was significantly associated with HCV infection among PWUD. While further studies, especially among PWUD living without shelter in Kabul and other major cities of Afghanistan, are recommended to better analyze the dangers among drug addicts. Based on our results and given the fact that adequate programs against drug use are scarce in Afghanistan, active preventive drug abuse programs focusing on educational campaigns and targeted at young people should be undertaken. It is a fact that intravenous injection of drugs, especially among drug addicts who are jobless and imprisoned, as well as sharing of injection equipment are associated with dangerous viral infections and should be highlighted in future public educational and informational campaigns.