1. Background
Myocardial ischemia/reperfusion (I/R) injury is a major complication of the primary percutaneous coronary intervention (PPCI) procedure. Several pathophysiological mechanisms, including the generation of oxygen products and platelet aggregation, are responsible for this irreversible event (1, 2). Finding novel adjunctive therapeutic strategies to limit myocardial I/R injury could mitigate the problem. Among these methods, melatonin, a hormone secreted from the pineal gland, has been shown to be effective against I/R injury in various organs (3). With oral administration, plasma peak level occurs during 40 - 60 minutes (4, 5). Prescribing a high dose (i.e., 1 - 5 mg) leads to 10 - 100 times melatonin concentrations higher than the physiological peak within the hour after ingestion (6).
A number of the biological effects of melatonin are associated with its ability to clear free radicals and emphasize the action of antioxidant enzymes. Additionally, its metabolism products manifest high radical clearing action (7). Experimental studies have revealed that melatonin raises the discharge of anti-inflammation chemicals (e.g., interleukin 10), obstructs the discharge of inflammation chemicals (i.e., tumor necrosis factor-alpha, interleukin 1 beta, and interleukin 6), and leads to an anti-inflammatory effect (8). It has been demonstrated that melatonin controls lipids in the blood and lessens the oxidized low-density lipoprotein cholesterol (9).
The cardioprotective effect of melatonin has been considered to bind to the melatonin receptors 1 (MT1) and 2 (MT2) (10). These receptors are linked to several intracellular survival signaling pathways, including the activation of the survivor activating factor enhancement (SAFE), the reperfusion injury salvage kinase (RISK), the Sirtuin signaling pathways (SIRT1 and SIRT3), and the mitochondria in cell death process (i.e., necrosis, apoptosis, autophagy, and mitophagy) (3, 11, 12). As stated by novel clinical trials, treatment with melatonin is safe, even if it might cause mild complications, such as a brief hypnotic effect, insignificant headache, and aggravating dyspnea. Therefore, when considering the use of melatonin with other drugs in combination therapy protocols, the potential for side effects caused by interactions should be taken into account (10).
2. Methods
2.1. Study Participants
In brief, the study population included 128 patients admitted with acute ST-elevation myocardial infarction (STEMI) to the Emergency Department of Modarres Hospital, Shahid Beheshti University of Medical Science, Tehran, Iran, who underwent PPCI with a balloon or stent. All the participants gave written informed consent before enrolling in the study. Moreover, the study protocol was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1398.371).
The patients were randomly assigned to two groups, including those receiving 3 mg of melatonin in the emergency department before adding PPCI to standard therapy (test group) and those receiving standard treatment alone (control group). A number was appointed for every patient, and odd and even numbers were determined as the test and control groups, respectively. Angiography was conducted immediately after the diagnosis of acute STEMI in both groups. All angiography and angioplasty procedures were performed with Siemens Axiom Artis (Erlangen, Germany). Successful angioplasty was considered residual stenosis not higher than 20%.
The myocardial blush grade (MBG) and thrombolysis in myocardial infarction (TIMI) frame count (TFC) were assessed visually on the angiogram by an interventional cardiologist blinded to both the test and control groups to evaluate microvascular integrity. The MBG has been defined as 0 (no contrast density or blush in myocardium), 1 (brief contrast density or blush in myocardial), 2 (modest contrast density or blush in myocardial, but smaller than a normal coronary artery), and 3 (normal contrast density or blush in myocardial, similar to a normal coronary artery) (13). When myocardial blush stained, it was considered the leakage of contrast medium into the extravascular space and was graded 0 (14). No digital techniques were used in this study. In order to evaluate blush grading, the final angiographic cine was extended to see the venous phase of the coronary vasculature.
The TFC was calculated as the number of cine frames required to fill the culprit vessels to standardized distal landmarks with contrast in the final angioplasty film. A standard frame count was defined as 20 ± 3.0 frames for the right coronary artery, 22 ± 4 frames for the left circumflex (LCX) artery, and 36 ± 2 and 21 ± 1 frames uncorrected and corrected, respectively, for the left anterior descending (LAD) artery (15).
2.2. Statistical Analysis
SPSS statistical software (version 16) was used to analyze the data with a significance level set at P < 0.05 (two-tailed). Categorical variables were described based on frequency rates and percentages. However, continuous variables were explained using the mean value. The data for continuous variables were compared using a one-sample t-test and the chi-square test. Missing values were excluded pending statistical analysis.
3. Results
The patients were randomly assigned to two groups of 64 cases, including those receiving a single dose of 3 mg of melatonin before PPCI (test group) and those not receiving this dose (control group). The age ranges of the studied participants were 35 - 91 and 36 - 83 years in the control and test groups, respectively. Table 1 shows the basic clinical characteristic profiles of participants. As shown in Table 1, the differences between the test and control groups were not statistically significant.
| Melatonin | Control | P-Value | |
|---|---|---|---|
| Age, y | 58 ± 8 | 56 ± 11 | 0.23 |
| Gender (male) | 82 | 79 | 0.27 |
| Diabetes mellitus | 9.4 | 17.2 | 0.193 |
| Hypertension | 12.5 | 22.6 | 0.045 |
| Hyperlipidemia | 14.1 | 14.1 | 1 |
| Smoking | 44.4 | 48.4 | 0.10 |
| Ischemic heart disease | 1.6 | 4.4 | 0.05 |
| Family history | 23.3 | 28.1 | 0.30 |
aValues are expressed as mean ± standard deviation or percentage.
After PPCI, the TIMI flow grade average was 2.6 ± 0.5 and 2.6 ± 0.6 in the test and control groups, respectively, which showed no significant difference (P = 0.76). The corrected TFC was also similar in both groups (20.1 ± 8.5 and 21.4 ± 10 in the test and control groups, respectively; P = 0.43).
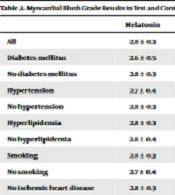
In the study as a whole and subgroup analysis, the MBG demonstrated a significant difference with melatonin prescription (2.8 ± 0.3 and 2.3 ± 0.7 in the test and control groups, respectively; P < 0.001).
| Melatonin | Control | P-Value | |
|---|---|---|---|
| All | 2.8 ± 0.3 | 2.3 ± 0.7 | < 0.001 |
| Diabetes mellitus | 2.6 ± 0.5 | 2.7 ± 0.6 | 0.8 |
| No diabetes mellitus | 2.8 ± 0.3 | 2.2 ± 0.7 | < 0.001 |
| Hypertension | 2.7 ± 0.4 | 2.4 ± 0.7 | 0.3 |
| No hypertension | 2.8 ± 0.3 | 2.3 ± 0.7 | < 0.001 |
| Hyperlipidemia | 2.8 ± 0.3 | 2.7 ± 0.4 | 0.6 |
| No hyperlipidemia | 2.8 ± 0.4 | 2.3 ± 0.7 | < 0.001 |
| Smoking | 2.8 ± 0.3 | 2.4 ± 0.6 | < 0.005 |
| No smoking | 2.7 ± 0.4 | 2.3 ± 0.9 | < 0.005 |
| No ischemic heart disease | 2.8 ± 0.3 | 2.3 ± 0.7 | < 001 |
a Values are expressed as mean ± standard deviation.
In patients with coronary risk factors, no significant difference was observed between the two groups. However, melatonin significantly improved the MBG in patients without such risk factors (Table 2). Regarding ejection fraction, comparison between the test and control groups showed no significant difference (41.7 ± 9.1 and 42.4 ± 8.4 in the test and control groups, respectively; P = 0.62), and similar results were obtained in subgroup analysis.
4. Discussion
Epidemiological studies demonstrated that the production and secretion of melatonin decrease in patients with coronary artery disease (16), and there is an independent relationship between oxidized low-density lipoprotein and low melatonin levels in patients with acute STEMI (17). A cohort study measured melatonin and oxidative stress chemicals in 25 patients as the test group with STEMI and 25 controls with no coronary artery disease. An association was observed between acute STEMI and a nocturnal serum melatonin deficit (16). The data from animal studies showed the protective effects of melatonin on I/R injury in the myocardial Tan et al., Kaneko et al., and Lagneux et al. demonstrated the beneficial effects of melatonin on I/R-induced arrhythmias in isolated rat hearts (17-20).
On the other hand, other studies have failed to show a beneficial protective effect of melatonin. Previous studies showed that melatonin did not have a protective effect on the heart in an animal model of acute STEMI (21, 22) and a rabbit model of myocardial I/R injury (23). While evaluating a study carried out by Dave et al., Duncker and Verdouw mentioned that the rabbit’s heart lacks xanthine oxidase, which might explain why melatonin failed to reduce cardiac dysfunction during I/R in this species (24). Although numerous studies performed on cells and animals have proven that melatonin has cardioprotective effects on I/R injury, fewer studies have reported its effect in patients with STEMI (16, 25). Lee et al. have shown that intravenous melatonin can significantly depress ventricular tachycardia and fibrillation and decrease the total number of premature ventricular contractions (26).
The present study proposed that melatonin could restrict myocardial destruction induced by I/R with its antioxidant effects. The current study observed that patients receiving melatonin had a better MBG while evaluating microvascular integrity during the assessment of the success of PPCI. Similar results were observed in the subgroups. The MBG was significantly improved in patients without any coronary risk factors or history of ischemic heart disease (IHD); nevertheless, it showed no improvement in patients with such problems. This could be due to an insufficient dose of melatonin (3 mg), which might advocate the administration of higher doses of melatonin in patients with risk factors, such as diabetes, hypertension, hyperlipidemia, or a history of IHD. It is noteworthy to mention that there was a discrepancy in the data regarding the administration of the same dose to patients who were smokers. One plausible explanation for this inconsistency could be that some patients were not inclined to admit they smoked.
Recently, the results of a placebo-controlled study demonstrated that intravenous- and intracoronary-administered melatonin failed to decrease myocardial infarct size in a significant manner. In addition, it might reduce the recovery of ejection fraction and enhance myocardial remodeling. The authors concluded that the symptom-to-balloon time was very long, which might have had an impact on the ability of melatonin to reduce I/R injury (27). In subgroup analysis, the infarct size was significantly smaller in patients in the short symptom-to-balloon time group (136 ± 23 minutes). However, a reverse effect was demonstrated in the long-time group (249 ± 41 minutes) (28). The difference between the aforementioned study and the present study is that in the current study, the patients were treated with 3 mg of melatonin before PPCI orally in the emergency department. In addition, giving melatonin before the PPCI procedure could have had a more noticeable effect.
Controversial comments have recently been made concerning the protective potential of melatonin in cardiac diseases with the MARIA trial on 146 STEMI patients who underwent PPCI. The aforementioned study failed to demonstrate the beneficial effects of melatonin on the reduction in infarct size and even showed unfavorable effects on the ventricular volumes and left ventricular ejection fraction (LVEF) (29). The results indicated that the effects of melatonin were related to the timing of reperfusion (27, 30).
Although the present study demonstrated an improved MBG, which is consistent with the findings of other studies that have reported the beneficial effects of melatonin on I/R injury, the current study’s results failed to show a positive effect on the TFC. This could be due to the fact that the MBG is a better means to assess the microvasculature than the TIMI frame count. Further incompatibilities have been demonstrated in some recent studies (22, 27, 31). Such inconsistencies might be due to the methods of administration (32), ischemic duration, or aspects of the study design. Furthermore, they might be explained by the use of healthy animals without cardiovascular risk factors and comorbidities, which are the characteristics of patients with STEMI or undergoing cardiovascular surgery (33). Therefore, in a well-planned study, the findings would support I/R injury protection (29). Considering such discrepancies, further studies are required.
4.1. Study Limitations
There are some limitations in the present study. The number of participants was small, which made proper subgroup analysis impossible. In addition, this study only evaluated a dose of 3 mg of orally administrated melatonin. Nevertheless, it would have been better if different doses were compared using various modes of administration.
4.2. Conclusions
The current study demonstrated the melatonin effects on I/R injury in STEMI patients treated with PPCI. The obtained data showed that melatonin acts as a potent antioxidant, reducing myocardial damage induced by I/R. The patients who received oral melatonin had better microvascular integrity than those who did not receive melatonin. It is a relatively safe drug, easily administered, with few short-term side effects. Furthermore, when administered orally, it is rapidly absorbed. However, further studies with more participants are needed to evaluate the beneficial impact of melatonin on STEMI patients.