1. Background
Mitral valve stenosis (MS), as a progressive disease, is one of the most important valvular disorders in developing countries, which can lead to significant morbidity and negative clinical outcomes (1). Rheumatic heart disease, as well as degenerative calcification of the mitral annulus, can be considered as major reasons for occurrence of MS (2). Mitral valve stenosis occurs in both genders of all age categories and races, but most evidence suggests a female predominance in patients who suffer from MS (2). Percutaneous transvenous mitral commissurotomy (PTMC) is a well-accepted treatment option for symptomatic MS that causes hemodynamic changes such as a decrease in left ventricular pressure and an increase in the preload (3).
In response to the overload of pressure and expansion of volume, the heart attempts to secret certain hormones such as Atrial (ANP) and B-type brain natriuretic peptide (BNP) natriuretic peptides (4). Brain natriuretic peptide is used as a prognostic marker for clinical outcomes in patients with heart failure and acute coronary syndrome. Since the level of BNP changes with left ventricular filling pressure and stress on the ventricle wall, monitoring this hormone can guide the response to treatment. Recently, it has been argued that there is an increase in the level of natriuretic hormones in patients with MS (5, 6). Therefore, the changes of these neurohormones may follow PTMC (7, 8).
Several PTMC related complications could be seen as a result of unsuccessful PTMC
such as embolic stroke, regurgitation, and restenosis of mitral valve which warrant replacement of mitral valve or repeated PTMC as soon as possible.
Numerous studies have reported that BNP levels are decreased immediately after PTMC (3-5). Therefore, measuring serum levels of BNP may predict the successfulness of PTMC procedure in patients with symptomatic MS, and may function as a reliable marker.
2. Objectives
This study aimed to determine the relationship between BNP levels and hemodynamic parameters in patients with MS who underwent PTMC.
3. Methods
3.1. Patients Selection
This case-control study was approved by Board Review of Shahid Beheshti University of Medical Sciences (SBUM), Tehran, Iran (code number: 615) after obtaining the informed consent from participants who had undergone PTMC from September 2015 to January 2017 and assessing them for enrollment in the study. Echocardiography left, and right catheterization was performed on all included patients before and after PTMC.
3.1.1. Exclusion Criteria
Patients with incomplete medical records, with moderate and severe left ventricular dysfunction (who had left ventricular ejection fraction less than 45%), with moderate or severe aortic, with mitral or tricuspid valve regurgitation, and with severe aortic stenosis were excluded from our study.
3.2. Study Protocol and Statistical Analysis
In the study group, BNP levels were measured by performing radioimmunoassay on all participants 30 minutes before PTMC and 24 hours after PTMC. Demographic data such as age and gender were collected from both groups. Full echocardiography (especially evaluation of mitral valve area (MVA) and mean gradient) was done on both study and control group. Catheterization data, including pulmonary artery pressure (PAP), left atrial pressure (LAP), right atrial pressure (RAP), left ventricular end-diastolic pressure (LVEDP), and right ventricular end-diastolic pressure (RVEDP) of all patients with MS were evaluated and recorded in the questionnaire during the study period.
The results from the parametric data analysis were expressed based on the mean and standard deviation. Qualitative and classified data were presented based on the number, percentage, and the univariate analysis on quantitative and qualitative data using t-test and chi-square tests. Data were analyzed by SPSS (v.18. IBM Inc. IL). A P-value less than 0.05 was considered significant.
4. Results
Fifty patients with MS who had undergone PTMC from September 2015 until January 2017 were included in this cross-sectional study. The mean age of the cases with MS was 45.14 ± 13.69 years. Furthermore, the youngest case was 24 years old, and the oldest one was 85 years old. Majority of the patients were aged 21 - 42 years. Out of 50 patients, six cases (12%) were males and 44 cases (88%) were females. The clinical characteristics of the patients are presented in Table 1.
| Values | |
|---|---|
| Male gender | 6 (12) |
| Diabetes mellitus | 10 (20) |
| Hypertension | 15 (30) |
| Hyperlipidemia | 10 (20) |
| Echocardiographic parameter | |
| LVEF | 7.4 ± 9.52 |
| LAP | 1.7 ± 6.24 |
| LVEDD | 49.0 ± 56.4 |
| LVESD | 53.0 ± 25.3 |
| RVID | 55.0 ± 05.3 |
Clinical Characteristics and Echocardiographic Parameters Before PTMC a
Only one patient (2%) had NYHA class I, and other 49 cases (98%) had NYHA class II. The type of cardiac rhythm was atrial fibrillation (AF) in 21 cases (42%) and sinus in 29 cases (58%).
The level of BNP before PTMC was 473.78 ± 66.95 pg/dl in patients with MS. The echocardiographic parameters in pre-PTMC in patient group are shown in Table 1. The systolic, diastolic, and mean pulmonary artery pressures were 51.52 ± 14.44 mm Hg, 25.97 ± 8.86 mmHg, and 35.45 ± 10.92 mmHg, respectively. Notably, the reduction in left atrial pressure as well as mitral valve gradient were observed in patients with MS after PTMC compared with before PTMC (P-value = 0.001) (Table 2). On the other hand, the mitral valve area after PTMC was remarkably increased in contrast with that before PTMC (P-value = 0.001) (Table 2).
| Parameters | P-Value | After PTMC | Before PTMC |
|---|---|---|---|
| LAP | 0.001 | 0.94 ± 15.6 | 7.1 ± 24.6 |
| Mitral valve gradient | 0.001 | 1.1 ± 1.8 | 5.2 ± 10.8 |
| Mitral valve area | 0.001 | 0.13 ± 1.44 | 0.150 ± 0.91 |
| LVEDP | 0.053 | 4. 1 ± 14.3 | 4.3 ± 13.5 |
Comparing Echocardiographic Parameters Before and After PTMC
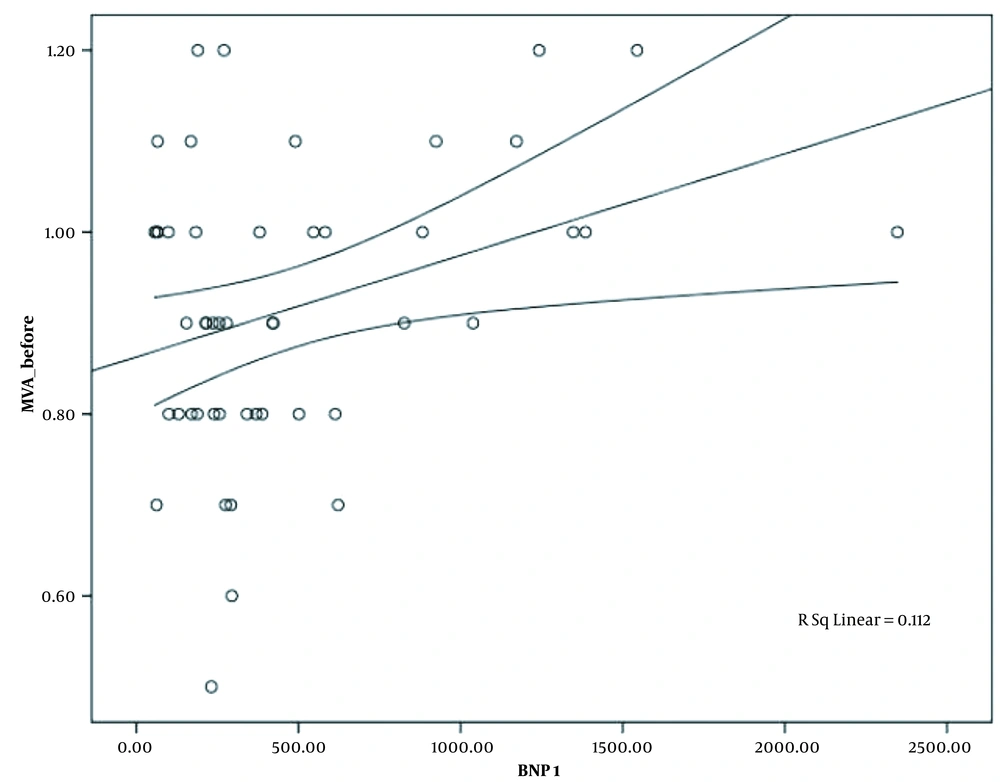
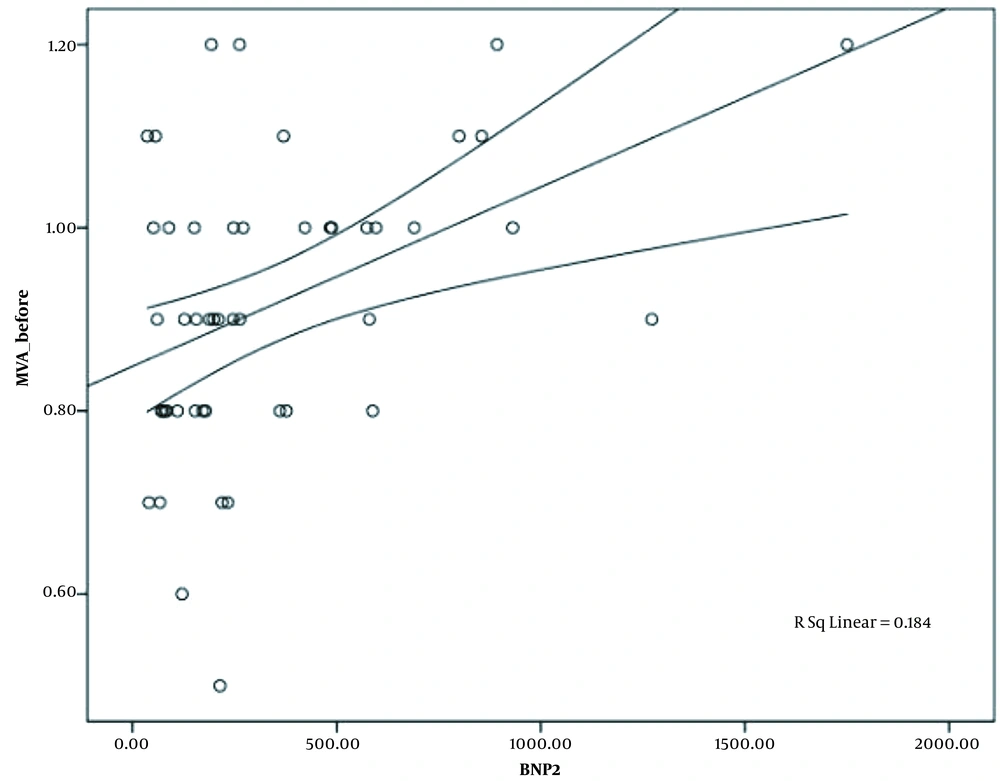
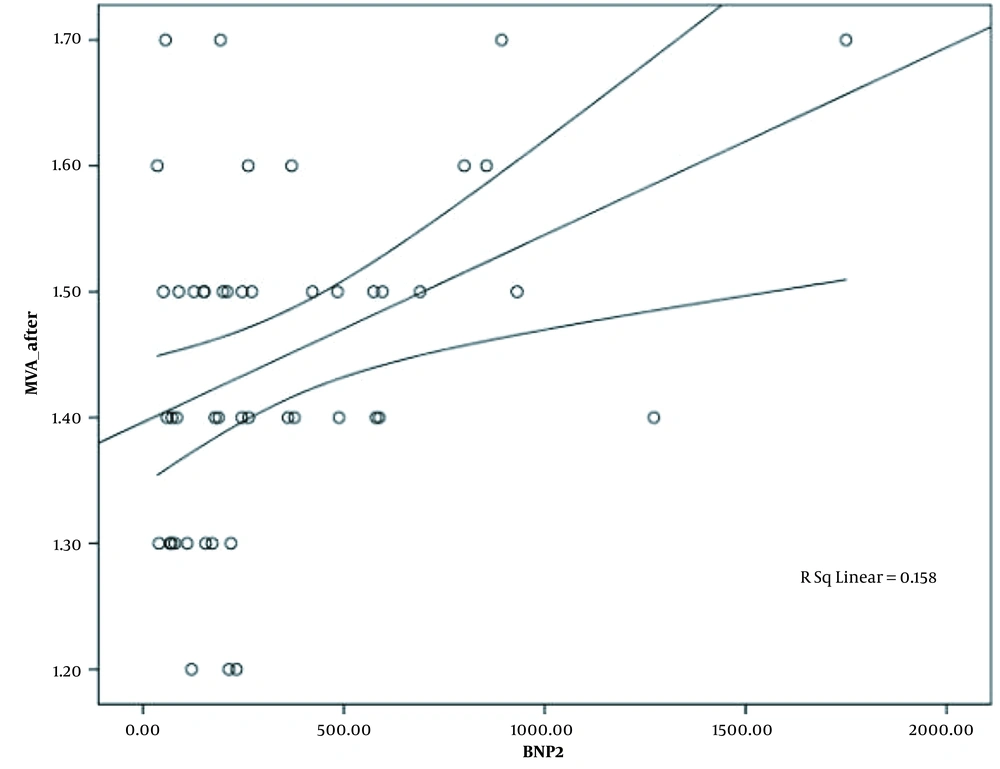
The mean level of BNP prior to PTMC was 473.78 ± 66.95 pg/dL by the lowest and highest level of 56 pg/dL and 2347 pg/dL, respectively. The mean level of post-PTMC BNP was 341.54 ± 48.3 pg/dL, which varied from 36 pg/dL in lowest level to 1750 pg/dL in highest one. Significant reduction was observed in BNP level after PTMC (P-value = 0.006). As it is shown in Table 3, post-PTMC, BNP level in patients with atrial fibrillation was significantly greater than the level of this neurohormone in patients with sinus rhythm (P-value = 0.03). There was a reverse correlation between the pre-PTMC BNP level and left ventricle ejection fraction, but it was not statistically significant (Pearson correlation = -0.259, and P-value > 0.05). According to Appendix 1, there was no significant relationship between the level of BNP before and after PTMC with the left atrial pressure (P-value > 0.05). On the contrary, there was a significant correlation between the level of BNP after PTMC with mitral valve area and left ventricle to end diastolic pressure (Appendix 2 and Figures 1-3). The changes in BNP levels had a significant correlation with pulmonary artery mean pressure variations (P-value = 0.03) (Table 4).
| Parameters | Patients with AF | Patients with SR | P-Value |
|---|---|---|---|
| The level of BNP before PTMC | 90.2 ± 547.6 | 93.3 ± 420.4 | 0.3 |
| The level of BNP before PTMC | 91.6 ± 476.5 | 43.7 ± 247.2 | 0.03 |
| P-value | 0.24 | 0.01 |
Comparing Levels of BNP in Patients with Atrial Fibrillation or Sinus Rhythm
| Differences of BNP Levels Parameters | Correlation Coefficient | P-Value |
|---|---|---|
| DPAMP | 0.3 | 0.03 |
| DPADP | 0.003 | 0.986 |
| DPASP | 0.007 | 0.962 |
| DLVEDP | 0.058 | 0.713 |
| DLAP | -0.019 | 0.906 |
| DMTMG | -0.076 | 0.635 |
| DMVA | 0.028 | 0.484 |
Correlation Between Differences of BNP Levels and Changes in Echocardiographic Parameters During the Study
5. Discussion
Percutaneous transvenous mitral commissurotomy can be considered one of the most appropriate therapeutic options for patients with MS, resulting in a reasonable and acceptable rate of success, and preventing or delaying the critical need for mitral valve repair or replacement (8). Plasma level of BNP is utilized for the assessment of mitral stenosis, and there is a significant correlation between levels of this neurohormone with the existence and severity of mitral stenosis (9).
In our study, the relationships between BNP levels and echocardiographic parameters in patients with MS before and after PTMC were compared. According to our results, a noticeable reduction was observed in post-PTMC BNP level of our MS patients. In a study by Zakkar et al., it was determined that NT-proBNP levels had a positive correlation with the severity of mitral stenosis (10). Therefore, the serum levels of this biomarker decreased significantly after the therapeutic procedure (10). Another study by Ahmad et al. showed that PTMC in patients with MS may have significantly decrease the serum level of BNP, reduced the pulmonary artery systolic pressure, and increased mitral valve area (9). Their findings were in line with our study results in this regard.
Furthermore, our results indicated that the serum level of BNP after PTMC in patients with atrial fibrillation may have been statistically and extremely higher than the level of this biomarker in patients with sinus rhythm. Pourafkari et al. reported that the level of natriuretic peptides in patients with AF was two times higher than that in patients with sinus rhythm (SR), but it was not significant (11). They also determined that the existence or non-existence of arrhythmia had no significant effect on the levels of these neurohormones (11). According to our findings discussed earlier, the level of BNP after PTMC had a strong correlation with mitral valve area and left ventricle end diastolic pressure. This result suggested that there was a considerable correlation between the changes in BNP levels and the differences in pulmonary artery mean pressure. Selcuk et al., however, demonstrated that the basic serum levels of NT-Pro BNP were independently correlated with Systolic pulmonary artery pressure alone (7). Pourafkari et al. discovered that the serum levels of BNP before and after PTMC were not closely associated with the changes in MVA. They also detemined that the changes in BNP levels may not have been considered as a predictor of the changes in MVA (11). Arat-Ozkan et al. found a clear correlation between serum NTproBNP level with echocardiographic findings and disease severity in patients with MS (12). In our study, however, no obvious statistical correlation was detected between BNP and LAP or PAP.
5.1. Conclusions
In sum, successful PTMC may have produced beneficial hemodynamic changes like a reduction in LAP and increase in preload capable of changing BNP level. Taking into account this single center and our limited study population, it was also concluded that a considerable decline in the serum level of BNP following effective PTMC may have improved the clinical and hemodynamic status; hence, it was reasonably suggested that the serum level of BNP was effective in evaluating the response to PTMC. However, it was recommended that multi center studies with larger populations should be carried out in order to draw more definitive conclusions.