1. Background
Warfarin is a pharmacological agent used for sixty years in the treatment and prevention of venous and arterial thromboembolic events. It was used as the only oral anticoagulant until novel oral anticoagulants (NOAC) were discovered (1). Although it has advantages such as daily single dose use, oral intake easiness, and low price, it also has disadvantages such as narrow therapeutic range, high drug-drug interaction, and high drug-nutrient interaction (2).
Warfarin is used for the treatment of diseases such as pulmonary thromboembolism (PTE), deep vein thromboembolism (DVT), and atrial fibrillation-related (AF) cerebrovascular event prevention, which may cause severe mortality and morbidity (3). To be effective, it should be present at a certain level in the blood. Thromboembolic protection cannot be provided below this level, and it may cause fatal bleeding when it is above this level. Thus, keeping warfarin within the therapeutic range is very important to prevent thromboembolic events, which is the primary objective, and to prevent undesired effects (2).
"International normalized ratio" (INR) is used to measure the therapeutic levels of warfarin. Keeping INR within the therapeutic range detected based on the disease is important for preventing mortality and morbidity. Thus, it is important to calculate the time in the therapeutic range desired during the period of use for patients using warfarin. To achieve this, time in therapeutic range (TTR) must be calculated for every patient. Time in the therapeutic range shows us the percentage of the time during which a patient uses warfarin within the therapeutic range (2, 4, 5).
For effective warfarin treatment, the TTR level should be 60% and above (2). High drug-drug interaction, drug-nutrient interaction of warfarin, and requirement of regular INR control are difficulties requiring the patient to understand the importance of treatment and increasing the need for patient and treatment compliance. The prescribing doctor should make it suitable for the patient due to treatment difficulties such as patient comorbidities and chronic drugs used.
2. Objectives
The objective of this study was to investigate the relationship between TTR levels and sociodemographic characteristics of patients using warfarin and the drugs they used and to investigate factors that can assist in the achievement of optimal TTR levels.
3. Methods
This study was considered ethically appropriate based on Sağlık Bilimleri University (S.B.U.) Okmeydanı Training and Research Hospital Ethics Board decree no 450. Files of patients who were admitted to S.B.U. Okmeydanı Training and Research Hospital Internal Diseases Polyclinics and used warfarin were scanned retrospectively. Patients who were using therapeutic warfarin and had a minimum INR level of 2 under the warfarin effect were included in the study. Patients who were under 18 years of age and those who used warfarin for purposes other than treatment (such as suicide) were not included in the study. Files were scanned both in the physical environment and through the hospital automation system. Among patients admitted for INR control between 06.04.2014 and 06.04.2016 who met the inclusion criteria, 50 male and 50 female patients, starting from those whose admission date for control was on the nearest, were included in the study. Exclusion criteria were determined as patient age under 18 or warfarin use for causes other than treatment (such as suicide). An equal number of female and male patients was included to investigate the effect of gender on TTR.
Information about age, gender, education level, occupation, weight, height, smoking and alcohol use, chronic diseases, drugs used, warfarin starting date, warfarin usage indication, INR, creatinine and alanine aminotransferase (ALT) levels were recorded for all study subjects.
The information was inputted into the Microsoft Excel 2013 software. Body mass index (BMI) was calculated by dividing weight in kilograms by the square of height in meters. Time in therapeutic range was calculated using the Rosendaal method.
3.1. Statistical Method
Mean, standard deviation, median minimum, maximum, frequency, and ratio values were used in definitive data statistics. Kolmogorov Smirnov test was used to measure the distribution of the variables. Mann-Whitney U test and independent sampling t-test were used to analyze the quantitative data. The chi-square test was used for qualitative data analysis, and the Fisher test was used when chi-square test conditions were not met. The Kappa compliance test was used for compliance analysis. SPSS 22.0 program was used for the analyses.
4. Results
Mean age was calculated as 61.7 ± 13.2 (24 - 89) years. Average body weight (kg) was detected as 82.5 ± 16.9 (50 - 130), average height (cm) was 166.4 ± 9.5 (150 - 188), and average BMI was 29.8 ± 5.7 (19 - 45). It was observed that TTR levels were 60% and above for 34 patients and over 60% for 66 patients (Table 1).
| Min - Max | Median | Mean ± SD or No. (%) | |
|---|---|---|---|
| Age | 24 - 89 | 62 | 61.7 ± 13.2 |
| Gender | |||
| Woman | 50 (50.0) | ||
| Male | 50 (50.0) | ||
| Weight (kg) | 50 - 130 | 80 | 82.5 ± 16.9 |
| Length (cm) | 150 - 188 | 165 | 166.4 ± 9.5 |
| BMI | 19 - 45 | 29 | 29.8 ± 5.7 |
| Cigarette use | 17 (17.0) | ||
| Alcohol use | 5 (5.0) | ||
| Profession | 0.0 | ||
| Unemployed-housewife | 36 (36.0) | ||
| Retired | 39 (39.0) | ||
| Worker | 11 (11.0) | ||
| Officer | 4 (4.0) | ||
| Self-employment | 10 (10.0) | ||
| Education status | 0.0 | ||
| Illiterate | 20 (20.0) | ||
| Literate | 21 (21.0) | ||
| Primary school | 41 (41.0) | ||
| Middle school | 3 (3.0) | ||
| High school | 13 (13.0) | ||
| University | 2 (2.0) | ||
| TTR % Rosendaal | 0 - 100 | 49 | 47.7 ± 28.9 |
| TTR Rosendaal | |||
| < 60 | 66 (66.0) | ||
| > 60 | 34 (34.0) | ||
| TTR % | 0 - 100 | 38 | 40.9 ± 24.4 |
| TTR | |||
| < 60 | 70 (70.0) | ||
| > 60 | 30 (30.0) |
Sociodemographic Characteristics and Time in Therapeutic Range levels
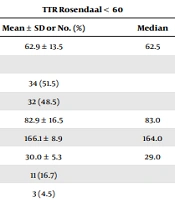
The average age was detected as 62.9 ± 13.5 for the group with TTR below 60% and as 59.4 ± 12.5 for the group with TTR of 60% and above. Thirty-four of those with TTR below 60% were female (51.5%), and 32 were male (48.5%); 16 of those with TTR of 60% and above were female (47.1%), and 18 were male (52.9%). Based on the BMI of the patients, 30 ± 5.3 was the average for the group with TTR < 60%, and 29.4 ± 6.5 was the average for the group with TTR > 60%. Eleven patients were smokers (16.7%), and 3 patients drank alcohol (4.5%) in the group with TTR < 60%; 6 patients were smokers (17.6%), and 2 patients drank alcohol (5.9%) in the group with TTR > 60%. The 2 groups had similar occupations and education levels (Table 2).
| TTR Rosendaal < 60 | TTR Rosendaal > 60 | P | |||
|---|---|---|---|---|---|
| Mean ± SD or No. (%) | Median | Mean ± SD or No. (%) | Median | ||
| Age | 62.9 ± 13.5 | 62.5 | 59.4 ± 12.5 | 61.5 | 0.209 |
| Gender | 0.673 | ||||
| Female | 34 (51.5) | 16 (47.1) | |||
| Male | 32 (48.5) | 18 (52.9) | |||
| Weight (kg) | 82.9 ± 16.5 | 83.0 | 81.6 ± 17.8 | 80.0 | 0.597 |
| Length (cm) | 166.1 ± 8.9 | 164.0 | 167.0 ± 10.7 | 166.5 | 0.875 |
| BMI | 30.0 ± 5.3 | 29.0 | 29.4 ± 6.5 | 28.7 | 0.449 |
| Cigarette use | 11 (16.7) | 6 (17.6) | 0.902 | ||
| Alcohol use | 3 (4.5) | 2 (5.9) | 1.000 | ||
| Profession | 0.916 | ||||
| Unemployed-housewife | 24 (36.4) | 12 (35.3) | |||
| Retired | 25 (37.9) | 14 (41.2) | |||
| Worker | 8 (12.1) | 3 (8.8) | |||
| Officer | 1 (1.5) | 3 (8.8) | |||
| Self-employment | 8 (12.1) | 2 (5.9) | |||
| Education status | 0.629 | ||||
| Illiterate | 15 (22.7) | 5 (14.7) | |||
| Literate | 14 (21.2) | 7 (20.6) | |||
| Primary school | 26 (39.4) | 15 (44.1) | |||
| Middle school | 3 (4.5) | 0 (0.0) | |||
| High school | 8 (12.1) | 6 (17.6) | |||
| University | 1 (1.5) | 1 (2.9) | |||
| TTR % Rosendaal | 31.0 ± 18.8 | 31.9 | 80.1 ± 12.8 | 78.9 | |
| TTR % | 28.9 ± 17.7 | 31.0 | 64.2 ± 18.1 | 60.5 | 0.000 |
| TTR | 0.000 | ||||
| < 60 | 66 (100.0) | 4 (11.8) | |||
| > 60 | 0 (0.0) | 30 (88.2) | |||
| Creatinine | 1.0 ± 0.3 | 0.9 | 1.2 ± 0.8 | 0.95 | 0.820 |
| ALT | 19.7 ± 10.5 | 17 | 18.9 ± 12.2 | 16 | 0.360 |
Relation Between Sociodemographic Characteristics and Time in Therapeutic Range Groups
Comorbid disease, chronic drug use, and drug use interacting with warfarin were similar among the groups (Table 3).
| No. (%) | P | ||
|---|---|---|---|
| TTR Rosendaal < 60 | TTR Rosendaal > 60 | ||
| Comorbid disease | |||
| DM | 15 (22.7) | 7 (20.6) | 0.807 |
| IHD | 46 (69.7) | 25 (73.5) | 0.689 |
| HF | 45 (68.2) | 21 (61.8) | 0.521 |
| HT | 31 (47.0) | 17 (50.0) | 0.774 |
| HL | 11 (16.7) | 7 (20.6) | 0.629 |
| CKD | 6 (9.1) | 2 (5.9) | 0.575 |
| COPD | 9 (13.6) | 2 (5.9) | 0.240 |
| Thyroid disease | 6 (9.1) | 6 (17.6) | 0.212 |
| BPH | 4 (6.1) | 5 (14.7) | 0.152 |
| Medication use | |||
| OAD | 10 (15.2) | 7 (20.6) | 0.493 |
| Insulin | 6 (9.1) | 1 (2.9) | 0.254 |
| Anti HT | 36 (54.5) | 19 (55.9) | 0.899 |
| Anti lipid | 11 (16.7) | 7 (20.6) | 0.629 |
| Anti arrhythmic | 57 (86.4) | 29 (85.3) | 0.884 |
| Antiplatelet | 15 (22.7) | 7 (20.6) | 0.807 |
| PPI | 30 (45.5) | 13 (38.2) | 0.490 |
| SSRI | 11 (16.7) | 4 (11.8) | 0.515 |
| Thyroid medication | 6 (9.1) | 6 (17.6) | 0.212 |
| Diuretics | 40 (60.6) | 22 (64.7) | 0.689 |
| Indication for the use of warfarin | |||
| AF | 43 (65.2) | 27 (79.4) | |
| Metallic valve replacement | 20 (30.3) | 5 (14.7) | |
| DVT | 3 (4.5) | 1 (2.9) | |
| Pulmonary embolism | 0 (0.0) | 1 (2.9) | |
| Medicines to reduce the effect of warfarin | 29 (43.9) | 14 (41.2) | 0.791 |
Relation Between Comorbid Diseases, Drugs Used, and Warfarin Use Indications and Time in Therapeutic Range Groups
5. Discussion
Time in the therapeutic range was found in over 60% of 34% of the patients. It was observed that gender, occupation and education level, body mass index, smoking status, comorbid diseases, drugs used, serum creatinine, and ALT levels were similar among TTR groups. The use of drugs decreasing the warfarin effect was found to be similar among TTR groups.
Although the number of patients using DOACs has surpassed warfarin in recent years, many patients are still on warfarin (6). As diseases such as AF, DVT, and PTE requiring anticoagulant use increase with increasing life expectancy, oral anticoagulant usage has also increased. Atrial fibrillation-related is the most common chronic cardiac rhythm disorder (7). While the prevalence of AF is 1/100 in the general population, this rate increases to 1/10 in the elderly (8). Ischemic stroke is the major complication caused by AF (9). Warfarin is used for protection against thromboembolic events such as ischemic stroke caused by AF. DVT and PTE are cardiovascular events that have the third highest prevalence after acute coronary syndrome and stroke, and they have the third highest prevalence among hospital-caused deaths (10, 11). Although warfarin is used for the treatment of diseases with high mortality and morbidity, its dosing adjustment is challenging due to its narrow therapeutic range, high drug-drug and drug-nutrient interactions, and the requirement of regular INR control. Wrong use of warfarin treatment can lead to complications with high mortality and morbidity, such as hemorrhagic stroke and gastrointestinal bleeding (12, 13). Therefore, maintaining warfarin dose within the required therapeutic range has vital importance.
In this study, the TTR level of only 34% of the patients was found to be equal to or higher than 60%, which is the warfarin treatment benefit threshold. In post-hoc analyses made by Connolly et al. with ACTIVE W study data, important differences were found in TTR levels among the countries and centers (14). In the study conducted by Pokorney et al. using data from the ORBIT-AF study, it was similarly demonstrated that TTR levels were different among the centers, and centers with anticoagulation clinics had higher TTR levels (15). It can be claimed that the low number of patients within the therapeutic range in this study could be due to the lack of a separate anticoagulation clinic in the hospital where the study was conducted and the irregular follow-ups as the polyclinic appointments were given from the central hospital appointment system.
The average age of the patients participating in the study was 61.7 ± 13.2 years. As life expectancy increases and the elderly population expands, diseases that need anticoagulants increase and turn into an important health problem. No statistically significant difference was found when we compared the ages of patients with and without TTR levels of 60% and above. In studies made by Pokorney et al. and Ciurus et al., patients were grouped based on a certain TTR level, and, similar to this study, the relationship with age was investigated, and it was observed that age had no effect in this regard (15, 16). In studies conducted by Wieloch et al. and Dlott et al., a positive correlation was found between age and TTR levels. Still, this difference may be due to the fact that the patients were compared on a numeric basis, and they were not separated into 2 groups based on TTR levels (17, 18). In light of this data, it is observed that age affects TTR levels, but the effect of age was not observed when patients below and above a certain TTR level were compared. When we compared the effect of education and occupation of patients with and without TTR levels below 60%, no statistically significant differences were observed with regard to these conditions. In the study by Pokorney et al., it was observed that college graduates had higher TTR percentages. This inconsistency with the current study may be due to the lack of a statistical difference, as only 2% of the patients were university graduates (15).
In the study, Apostolakis et al. developed SAMe-TT2R2 scoring with the outcomes; it was demonstrated that the female gender had a negative effect on TTR level (19). The negative effect of the female gender on anticoagulation control was confirmed in the studies by Lobos-Bejarano et al. and Rose et al. (20, 21). Similar to the findings of Pokorney et al. and Celik et al., it was demonstrated that gender did not have any influence on TTR levels in this study (15, 22). Therefore, it seems that further studies with larger samples are necessary to determine the gender effect. Smoking increases warfarin clearance by inducing cytochrome enzymes (23), and the INR level of smokers should be checked more often. The strong negative connection between smoking and TTR level was demonstrated in the Apostolakis et al. (19) study, and smoking had a score of 2 in SAMe-TT2R2 scoring. Similar to this study, in studies by Chan et al. (24) and McGriff-Lee et al. (25), a statistically significant connection was not observed between smoking and TTR levels (24, 25). Although many studies have confirmed that SAMe-TT2R2 scoring can predict non-conforming TTR levels with a high probability, the effect of only smoking is unclear when these results are considered.
Patients using warfarin are generally elderly patients with many comorbidities and regular drug use. Thus, the relationship between TTR level and comorbidity and drug use is very important and was one of the main objectives of this study. No statistically significant relationship was observed between comorbid diseases and drug use and TTR levels. No relationship was shown between comorbidities and TTR level in the Wypasek et al. study (26). A negative correlation with arterial hypertension in the study by Ciurus et al. was demonstrated, but no relationship was observed with other comorbidities (16). A negative correlation was also shown with anemia, chronic obstructive pulmonary disease (COPD), diabetes mellitus (DM), chronic kidney disease (CKD), and CHF in the study by Pokorney et al. (15). Similar to this study, in the study by Apostolakis et al., it was demonstrated that individual comorbidities did not affect TTR levels. However, when 2 or more comorbidities coexist, they have a negative correlation with TTR levels (19). However, similar to our study, all other important studies compared the patients by separating them into 2 - 4 groups based on their TTR levels. The TTR values of the patients with a therapeutic level below the demanded value (ex: TTR > 60%) do not have numeric importance because these patients do not benefit from the warfarin treatment regardless of their TTR levels. Warfarin may even have a negative effect as it increases the risk of bleeding (27, 28). When this situation is considered, data acquired from this study can be of more clinical importance.
Drug-drug interactions are another warfarin treatment challenge that should be considered and may be difficult to manage for both patients and physicians. In addition to documented drug interactions (Table 2), many interactions are published in the literature as case reports. Although many studies have investigated the effects of drugs on warfarin dose and INR level, there are very few studies investigating this relationship with TTR. When TTR levels of patients using drugs that lower warfarin’s effect was checked, no statistically significant difference was seen between the 2 groups. Similar to this study, in the study by McGriff-Lee et al., it was demonstrated that there was no statistically significant relationship between TTR levels and the use of drugs influencing warfarin levels (25). These results can be interpreted as a statistically significant issue due to the low number of studies and the inadequate number of patients and also due to the fact that follow-ups were managed based on using interacting drugs use by both the patient and the doctor provided INR stability and were not effective on TTR. Current guidelines on anticoagulation recommend that patients using interacting drugs or those with a new drug added to their treatment should be followed up more stringently (2, 3).
The study's limitations include being single-centered, having a small number of patients, and being retrospective.
5.1. Conclusions
In conclusion, this study demonstrated that no single factor is effective on the TTR level, and many factors affect the TTR level cumulatively. Although scoring systems are available, there is no adequate data to predict TTR lability. Following patients regularly in the light based on updated guidelines and urgently adjusting treatment in patients with labile INR appears rational to keep TTR within the desired range.