1. Background
Coronary artery disease (CAD) constitutes the leading cause of death worldwide (1-3). In patients with acute coronary syndrome (ACS), which includes ST elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI), and unstable angina (UA), early risk stratification is the cornerstone of therapeutic strategies (4, 5). The Global Registry of Acute Coronary Events (GRACE) is recommended by American and European current clinical guidelines to stratify the risk of mortality in-hospital and within 6 months (6, 7). It is measured by clinical variables, including age, systolic blood pressure, heart rate, cardiac arrest, and Killip classification; electrocardiographic parameters, including ST-segment deviation; and laboratory values, including creatinine level and elevated cardiac enzymes (8). Although the GRACE score calculates the risk of recurrent events and mortality, it is not intended for prediction of the severity and complexity of CAD.
The Synergy Between Percutaneous Coronary Intervention (SYNTAX) score, a comprehensive grading system based on coronary angiography (CA) findings, aims to classify the extent and complexity of CAD (9).This score guides in making the decision between performing coronary artery bypass grafting (CABG) surgery or percutaneous coronary intervention (PCI) (10). However, if a non-invasive assessment method of coronary anatomy prior to CA could be developed, the therapeutic decision, intensity, and timing of intervention could be modified.
To date, only a number of studies have investigated the usefulness of GRACE scoring in predicting severe CAD. Most of these studies did not enroll patients with STEMI (11-14). However, the GRACE score can also guide cardiologists to assess the need for an early PCI after fibrinolytic therapy in STEMI patients (15).
2. Objectives
In the present study, we aimed to determine the correlation between the GRACE and SYNTAX scores among patients admitted with ACS (UA, NSTEMI, and STEMI). Therefore, we sought to assess the value of the GRACE score for predicting angiographic features.
3. Methods
This cross-sectional study prospectively enrolled a total of 101 consecutive patients diagnosed with ACS who underwent CA, presenting to the Cardiac Emergency Unit of Shahid Modarres Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran, between 2021 and 2023. In our study, we included clinically diagnosed ACS patients who were indicated for CA because they met 1 of the following criteria: (a) patients presenting to the emergency department with chest pain less than 2 months since the onset of symptoms; (b) patients with electrocardiogram (ECG) changes indicative of acute ischemia; and (c) patients with elevated cardiac enzyme levels. There were no exclusion criteria in our study. The study was performed in accordance with the principles of the Declaration of Helsinki (16) and was reviewed and approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (ID: IR.SBMU.MSP.REC.1400.390). Written informed consent was provided by all ACS patients participating in the study.
Baseline clinical features were documented for each study participant at the time of admission. A checklist was used to assess demographics and cardiovascular risk factors (i.e., smoking, alcohol consumption, dyslipidemia, diabetes mellitus (DM), hypertension, family history, history of previous CAD, history of previous myocardial infarction (MI)). In addition, the parameters used in the GRACE scoring system (i.e., age, systolic blood pressure, heart rate, Killip classification, cardiac arrest in-hospital, elevated cardiac enzymes, creatinine level, ST-segment deviation) were recorded and assessed by a cardiologist (8). The GRACE ACS Risk and Mortality Calculator (available online at www.mdcalc.com) was used to calculate the GRACE risk.
Coronary angiography was performed for all participants in the Shahid Modarres Hospital Catheterization Laboratory. An experienced interventional cardiologist assessed all coronary angiograms visually, blinded to patients’ other clinical data. To assess the complexity and extent of coronary artery lesions, the interventionist calculated the SYNTAX score for all participants using the algorithm and calculator as previously described in detail on the website (https://syntaxscore.org).
3.1. Statistical Analysis
Data are reported as mean ± standard deviation (SD) for continuous variables and as frequency and percentage for categorical variables. Mann-Whitney U test and Wilcoxon test were used for comparison of GRACE and SYNTAX scores between various subgroups of the study (i.e., diabetic and non-diabetic, with and without heart failure, negative and positive family history of CAD, with or without dyslipidemia, smokers, and non-smokers). The chi-square test was used for the comparison of categorical variables between the groups. The Pearson correlation analysis was performed to determine the association between SYNTAX and GRACE scores. We categorized patients based on their GRACE/SYNTAX scores to assess the difference between mean values of systolic blood pressure, heart rate, and creatinine. The GRACE score < 109 was considered low-risk, 109 ≤ GRACE score < 140 was considered intermediate-risk, and the GRACE score ≥ 140 was considered high-risk. SYNTAX score < 23 was considered low-risk, 23 ≤ SYNTAX score < 32 was considered intermediate-risk, and SYNTAX score ≥ 32 was considered high-risk. Two-tailed statistical tests were applied, and statistical significance was defined as P values < 0.05. Statistical analysis was performed using SPSS v. 22 (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp.).
4. Results
A total of 101 consecutive patients (18 (17.8%) women and 83 (82.2%) men) who were diagnosed with ACS (UA, NSTEMI, and STEMI) and underwent CA were recruited for the study. The mean age of the enrolled patients was 57.2 ± 11.6 years. Moreover, 48.5% of patients had a history of MI. In addition, 31.7% and 44.4% of the participants suffered from DM and dyslipidemia, respectively. Besides, 60.4% of these patients were smokers. Of the total number of patients, 49 (48.5%) were classified as low-risk, 38 (37.6%) as intermediate-risk, and 14 (13.9%) as high-risk, based on the GRACE score that was calculated on admission. The mean GRACE score in the study was 114.5 ± 26.2. According to the determined SYNTAX score, low-complexity CAD (SYNTAX score < 23) was observed in the majority of the participants (85.1%), whilst only 14.9% of participants were classified as intermediate-complexity CAD (23 ≤ SYNTAX score < 32), and none of the study participants obtained a SYNTAX score ≥ 32. The mean SYNTAX score in our study population was 15.1 ± 5.9. Baseline clinical and laboratory parameters are reported in Table 1.
| Parameters | SYNTAX Score < 23 | SYNTAX Score > 23 | P-Value |
|---|---|---|---|
| Systolic blood pressure (mmHg) | 119.01 ± 18.89 | 114.78 ± 6.23 | 0.45 |
| Heart rate (bpm) | 81.53 ± 11.12 | 93.15 ± 3.68 | 0.04 |
| Creatinine (mg/dL) | 1.12 ± 0.2 | 1.04 ± 0.06 | 0.28 |
Clinical Characteristics of Patients Based on the Synergy Between Percutaneous Coronary Intervention (SYNTAX) Score a
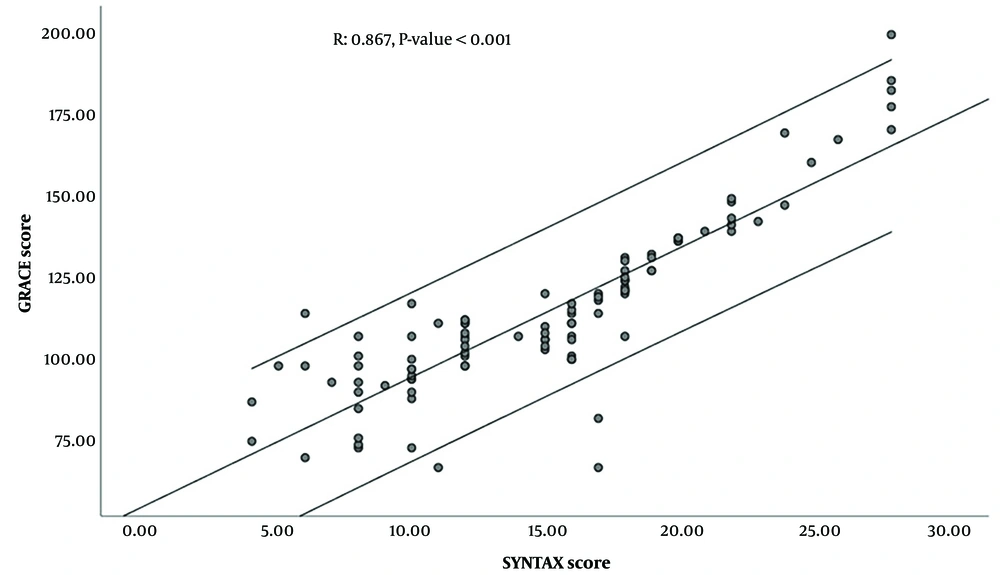
This study demonstrated a significant positive correlation between the GRACE score and SYNTAX score (based on angiography) (r = 0.867, P < 0.001) (Figure 1).
Amongst various subgroups of the study (i.e., diabetic and non-diabetic, with and without heart failure, negative and positive family history of CAD, with or without dyslipidemia, smokers, and non-smokers), only heart failure seemed to cause a statistically significant difference in GRACE and SYNTAX scores between patients with heart failure and those without heart failure. The median GRACE and SYNTAX scores were both higher in patients with heart failure than those without heart failure (P = 0.002 and P < 0.001, respectively).
5. Discussion
In the present work, we tried to evaluate the correlation between the GRACE and SYNTAX scores among patients admitted with ACS (UA, NSTEMI, and STEMI) in order to assess the value of the GRACE score for predicting angiographic features. Based on our data, the mean GRACE score was 114.5 ± 26.2. The low-complexity CAD (SYNTAX score < 23) was observed in 85.1% of participants, whilst only 14.9% of participants were classified as intermediate-complexity CAD (23 ≤ SYNTAX score < 32), and none of the study participants obtained a SYNTAX score ≥ 32. Only heart failure seemed to cause a statistically significant difference in GRACE and SYNTAX scores between patients with or without heart failure. Our study demonstrated a significant positive correlation between the GRACE score and the SYNTAX score (based on angiography) in patients with ACS.
A proper treatment strategy can be selected by early identification of CAD complexity since CABG is proven to be beneficial to patients with high and intermediate SYNTAX scores (SYNTAX score ≥ 23) (17). Therefore, the GRACE score may serve as a non-invasive method for predicting CAD severity prior to angiography.
To date, a number of studies have investigated the association of GRACE score with the severity of CAD involvements (12-14, 17-25). Consistent with our findings, Rahmani et al. (13) also reported that there is a weak positive correlation between GRACE and SYNTAX scores in UA and NSTEMI patients (r = 0.34, P < 0.001). A similar patient population was investigated by Avci et al. (12), and a positive significant correlation (r = 0.338, P < 0.001) was demonstrated between the GRACE and SYNTAX scores. In a similar study, Hammami et al. (19) found a correlation between these 2 scores, which was weak but significant (r = 0.23, P < 0.001).
To the best of our knowledge, in this regard, only 2 studies included STEMI patients in addition to NSTEMI and UA patients. In line with our findings, Sofidis et al. (20) found that GRACE and SYNTAX scores in patients with ACS correlated positively. Based on their study, the correlation was weak, although statistically significant (r = 0.32, P < 0.001). In another study with the same population, including STEMI, Bekler et al. (18) demonstrated a positive correlation between these scores as well (r = 0.427, P < 0.001).
Our data provides further evidence of the correlation between GRACE and SYNTAX angiographic score, which is a statistically significant, strong positive correlation (r = 0.867, P < 0.001) and also includes STEMI patients.
Although the GRACE risk score is useful in estimating the risk of mortality in-hospital and within 6 months, our study also indicates that it could represent the severity of coronary artery involvement prior to angiography.
Certain limitations need to be considered in interpreting our findings. Our investigation was conducted at a single center, and a relatively small number of participants were involved. None of our participants obtained a severe SYNTAX score (SYNTAX ≥ 32).
5.1. Conclusions
Our findings point out a significant strong positive correlation exists between GRACE score and SYNTAX score patients with UA/NSTEMI/STEMI who were indicated to undergo CA. Our results need to be accredited prospectively by large-scale, multi-center investigations.