1. Background
Myocardial bridging (MB) is the most common type of congenital abnormality that usually exhibits no specific symptoms, but it can lead to dangerous disorders in the human heart. According to the obtained results, diagnosing this disease is very difficult because most of the time it presents no symptoms, or complications are rare (1-4).
In MB, a portion of the coronary arteries delves into the underlying layer of the heart muscle and then emerges again. Typically, in 70 - 90% of cases, the myocardial bridge is located in the second part of the left anterior descending artery (LAD) (3-6).
In advanced stages of this disease, when the cardiac muscle bridge enlarges and exerts pressure on the coronary arteries supplying the heart, individuals may experience symptoms such as angina pectoris, myocardial ischemia, acute coronary syndrome, left ventricular dysfunction, arrhythmias, and even sudden cardiac death (1, 5-8). Myocardial bridging should be considered a possible cause of exertional chest pain, especially in young patients with no significant coronary artery disease. Physiological assessment to confirm the hemodynamic significance of MB involves exercise echocardiography or dobutamine myocardial perfusion imaging (6).
Moreover, coronary angiography is considered the gold standard for diagnosing this disorder. Other modalities, like intravascular sonography and multidetector computed tomography, are also useful for diagnosis (9, 10). During coronary angiography, the detection rate of MB is relatively low, ranging from 0.8% to 4.9% (6). The diagnosis of MB by coronary angiography is challenging as it relies on indirect signs, including “systolic compression and the milking effect,” rather than direct visualization. Thus, studies that used coronary angiography underestimated the prevalence of MB compared to pathological studies. However, it has been noted that more MB were detected in studies where the investigator was exploring previous angiographies to search for MB (11), or when intracoronary acetylcholine was used (9, 11). Although the prevalence of MB varies significantly according to the methods used and the conditions of the patients, studies show that among patients with hypertrophic cardiomyopathy, the phenomenon of MB is significantly more frequent, with an average prevalence of 30% in adults (9, 12).
2. Objectives
Given the significant diversity in the form and clinical manifestations observed in patients with myocardial bridge, a patient registry and survey are necessary to better understand the outcomes and determine the best management methods for these patients. Thus, this study aimed to assess the epidemiological, angiographic, and cardiovascular outcomes of patients diagnosed with myocardial bridge.
3. Methods
This two-centered, cross-sectional prospective study was conducted at a tertiary center in the North of Iran, enrolling 151 consecutive patients who had undergone angiography at Heshmat and Aria hospitals in Rasht from May 2014 to May 2016. Ninety-four patients did not meet the inclusion criteria and were excluded from the study.
(1) Patients undergoing coronary angiography or coronary artery bypass graft (CABG).
(2) Patients who, in addition to myocardial bridge, have another vascular stenosis that may cause cardiac ischemic symptoms (any stenosis of more than 70% in the angiography report).
3.1. Statistical Method
All data were entered into SPSS version 16 software, and quantitative variables were reported as mean and standard deviation, while qualitative variables were reported as frequency percentages. Descriptive statistics, chi-square tests, and independent t-tests were used for analyzing the data, and the significance level for the tests was set at P < 0.05.
4. Results
Table 1 presents the demographic and clinical information of the participants. Among the 57 patients examined in this study, 53 patients (93%) had a single bridge, and 4 patients (7%) had two bridges. All patients with a single bridge in this study had left anterior descending artery (LAD) involvement, while 4 patients had two bridges, 3 patients had another vessel involved in addition to LAD, and one patient had two bridges on LAD. Among the total of 61 bridges observed in 57 patients, LAD was the most commonly involved vessel, with 58 (95.08%) bridges located above LAD. The other 3 bridges were located above the RCA, OM, and Diagonal.
| Variables | Values a |
|---|---|
| Age (y) | 56.12 ± 9.8 |
| Sex | |
| Male | 33 (57.9) |
| Female | 24 (42.1) |
| Number of bridge | |
| Single bridge | 53 (93) |
| Two bridges | 4 (7) |
| Involvement of a vessel with a bridge | |
| LAD | 53 (93) |
| Involvement of a vessel with two bridges | |
| LAD | 1 (1) |
| LAD and another vessel | 3 (6) |
| HIP | |
| Yes | 36 (63.15) |
| No | 21 (36.85) |
| HTN | |
| Yes | 35 (61.4) |
| No | 22 (38.6) |
| DM | |
| Yes | 19 (33.3) |
| No | 38 (66.7) |
Demographic and Clinical Information of the Participants
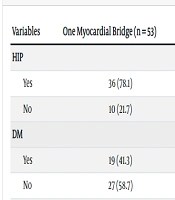
Table 2 demonstrates the frequency of myocardial bridge based on clinical and paraclinical findings. Of patients with a single myocardial bridge, 27.1% had positive ischemic changes in ECG, 69.6% had ischemia in the exercise test, 76.1% had hypertension, 41.3% had diabetes, and 78.1% had hyperlipidemia.
| Variables | One Myocardial Bridge (n = 53) | Two Myocardial Bridges (n = 4) |
|---|---|---|
| HIP | ||
| Yes | 36 (78.1) | 3 (75) |
| No | 10 (21.7) | 1 (25) |
| DM | ||
| Yes | 19 (41.3) | 1 (25) |
| No | 27 (58.7) | 3 (75) |
| HTN | ||
| Yes | 35 (76.1) | 3 (75) |
| No | 11 (23.9) | 1 (25) |
| ECG | ||
| Positive | 13 (27.1) | 1 (25) |
| Negative | 35 (72.9) | 3 (75) |
| ETT | ||
| Positive | 16 (69.6) | - |
| Negative | 7 (30.4) | 4 (100) |
| Heart scan | ||
| Positive | 21 (84) | 1 (25) |
| Negative | 4 (16) | 3 (75) |
Frequency of Myocardial Bridge Based on Clinical and Paraclinical Findings a
According to Table 3, the average bridge length in patients with positive ischemic changes in ECG was 17.3 ± 6.6 mm, with a positive exercise test was 14.89 ± 1.49 mm, and in patients with a positive heart scan was 16.78 ± 7.52 cm. Using independent t-test analysis, there was no significant difference in terms of myocardial bridge length with paraclinical findings (P > 0.05). Additionally, the average distance between the myocardial bridge and the vessel in patients with positive ischemic changes in ECG was 48.08 ± 6.68, with a positive exercise test was 44.919 ± 9.97, and in patients with a positive heart scan was 50.55 ± 11.17. Using statistical tests, there is a significant difference between the two groups with positive and negative exercise test in terms of the distance between the bridge and the opening of the vessel (P = 0.010), while according to the rest of the paraclinical findings, there was no statistically significant difference in the distance from the bridge to the vessel opening (P > 0.05).
| Variables | ECG | P-Value b | ETT | P-Value b | Heart Scan | P-Value b | |||
|---|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | Positive | Negative | ||||
| Myocardial bridge length | 17.3 ± 6.6 | 15.6 ± 0.98 | 0.4 | 14.89 ± 1.49 | 17.4 ± 2.35 | 0.372 | 16.78 ± 7.52 | 15.5 ± 4.5 | 0.74 |
| The distance between the myocardial bridge and the vessel | 48.08 ± 6.68 | 50.56 ± 29 | 0.599 | 44.919 ± 9.97 | 63.214 ± 21.52 | 0.01 | 50.55 ± 11.17 | 47.92 ± 26.39 | 0.736 |
Examination of One Myocardial Bridge Based on Paraclinical Findings a
Characteristics of one myocardial bridge based on gender are demonstrated in Table 4. According to this table, the average length of the vein bridge is 18.05 ± 6.8 in men and 13.44 ± 2.8 in women, and using independent t-test analysis, there is a significant difference between the two genders in terms of the length of the bridge (P-value = 0.004). The average distance between the myocardial bridge and the vessel is 54.24 ± 15.57 and 43.67 ± 7.81 in men and women, respectively. Additionally, using independent t-test analysis, it was realized that there is a significant difference between the two sexes in terms of the length of the pons (P-value = 0.004).
| Variables | Total | Men | Women | P-Value b |
|---|---|---|---|---|
| Myocardial bridge length | 16.051 ± 5.87 | 18.05 ± 6.8 | 13.44±2.8 | 0.004 |
| The distance between the myocardial bridge and the vessel | 49.655 ± 13.75 | 54.24 ± 15.57 | 43.67±7.81 | 0.004 |
Characteristics of One Myocardial Bridge Based on Gender a
5. Discussion
This study investigated the characteristics of muscle bridges and the severity of myocardial ischemia in patients undergoing angiography. Among the 57 patients examined, most with myocardial bridges were men, with men outnumbering women by about 1.5 times. Previous studies have also shown a higher prevalence of myocardial bridges in men compared to women, although the exact ratio varies widely across studies (9, 13, 14).
Our data revealed that 95.08% of bridges were located above the LAD, while the remaining bridges were situated above the RCA, OM, and Diagonal artery. Researchers suggest that the prevalence of bridges mainly on the LAD is due to its straight longitudinal path, whereas both the RCA and the Circumflex arteries have more curved paths. Consequently, this anomaly is more easily visible and detectable in angiography, whereas bridges located on other arteries may be less conspicuous and more likely to go unnoticed, often only detected during autopsy.
Contrary to previous findings (15), a minority of patients in our study exhibited ischemic changes in the ECG. Additionally, most patients had hyperlipidemia and hypertension, while diabetes was present in less than half of the patients. It's worth noting that among these comorbidities, hypertension is more strongly associated with myocardial bridges, potentially leading to increased myocardial thickness. Consequently, this complication is more commonly observed in patients with hypertrophic cardiomyopathy. Greater myocardial thickness is associated with more effective bridges and increased ischemic events, leading to more positive paraclinical findings, such as ECG abnormalities, positive exercise tests, and abnormal heart scans in these patients.
The observed differences may also be influenced by racial and epidemiological disparities across different societies, as well as variations in healthcare systems among different countries.
In terms of the average length of the myocardial bridge and the average distance from the bridge to the vessel orifice, we observed higher values in males compared to females. A study by Radu et al. on myocardial bridges indicated a difference of 9.9 mm between the maximum length of myocardial bridges in the two genders, with an average length difference of 4.22 mm, both favoring males (16).
The results of our study showed that the average length of the myocardial bridge and the average distance from the bridge to the vessel orifice were greater in men than in women. However, we found no significant relationship between the length of the bridge and the occurrence of ischemic changes in ECG, exercise tests, and myocardial perfusion scans. Controversy exists regarding the correlation between ischemic symptoms and the length of the tunneled segment (17).
Nevertheless, a significant relationship was observed between the distance of the bridge from the opening of the vessel and ischemic changes in the exercise test. The average distance of the bridge from the vessel opening was shorter in patients with a positive exercise test compared to those with a negative test (P-value = 0.010). These new findings suggest that exercise stress tests often reveal nonspecific signs of ischemia, conduction disturbances, or arrhythmias, making it challenging to distinguish between MB and other causes of myocardial ischemia. Angina frequently occurs during exercise, even in the absence of ECG changes (14).
Researchers suggest that including more patients in the study or utilizing another diagnostic modality such as CT angiography could provide further insights into myocardial bridges. They recommend investigating the myocardial depth of the bridges in addition to their length and distance from the vessel opening, along with exploring the relationship between bridge depth and myocardial ischemia. Additionally, they propose modifying the assessment of the bridge length by considering the ratio of the bridge length to the total length of the involved vessel. Regarding the distance of the bridge from the orifice, it is suggested to evaluate not only the longitudinal distance in millimeters but also the position of the bridge within the LAD, determining whether it is located in the proximal, mid, or distal portion of the vessel. Since the severity of myocardial bridge compression may vary over time, leading to variations in ischemia examination results such as exercise tests, heart scans, and ECGs, the researchers recommend prospective examination of the consequences and diagnostic modalities.
5.1. Conclusions
In patients diagnosed with an MB by coronary angiogram (CAG), the highest occurrence of MB was found in the LAD. This finding may contribute to a better understanding of outcomes and guide the selection of optimal management methods for these patients.