1. Background
Heart failure (HF) is a complex clinical syndrome characterized by a set of symptoms, including shortness of breath, ankle swelling, and fatigue, which may be accompanied by signs such as increased jugular vein pressure, pulmonary crackles, and peripheral edema. The diagnosis of HF requires the identification of the underlying etiology of cardiac dysfunction, which is often attributed to myocardial dysfunction, but can also be caused by valvular, pericardial, and endocardial pathologies, as well as heart rhythm and conduction abnormalities (1, 2).
The epidemiology of HF is characterized by a decline in age-stratified incidence in developed countries, potentially reflecting improved management of cardiovascular disease, whereas the overall prevalence is increasing due to global aging (3, 4). The prevalence of HF is estimated to be around 1 - 2% of adults, although the true prevalence may be higher due to the inclusion of only detected/diagnosed cases in most studies (5, 6).
Heart failure is classified into three categories based on ejection fraction (EF): Reduced EF (HFrEF), mid-range reduced EF (HFmrEF), and preserved EF (HFpEF). All three types of HF are associated with high mortality rates due to comorbidities and the inherent nature of the disease itself (7). The two main causes of HF are ischemic heart disease and hypertension, both of which have a relatively high prevalence (2).
The prognosis of patients with HF has improved significantly over the past few decades. However, it remains poor, and the quality of life (QOL) is significantly reduced (8). The 1-year and 5-year mortality rates after diagnosis for all types of HF patients were 20% and 53%, respectively, between 2000 and 2010 (9). Notably, transitions in EF are common over time, and patients who progress from HFmrEF to HFrEF have a worse prognosis than those who remain stable or transition to a higher EF category (10-12).
The European Society of Cardiology (ESC) has recently published new guidelines on the diagnosis and treatment of HF, which incorporate significant changes based on the large body of clinical studies conducted in the field of HF (13). The latest ESC guidelines aim to provide evidence-based guidance for healthcare professionals to manage heart disease effectively (14). The revised guidelines emphasize the importance of reducing the consequences of HF, particularly mortality, and highlight the need for evidence-based treatment approaches. Symptomatic benefits have also been noted with specific treatments (15).
In an effort to reduce the burden of HF in Iran, we designed a study to compare the quality of treatment for patients with HF against the latest ESC guidelines.
2. Objectives
This study aims to inform future policy changes to improve the QOL for Iranian patients with HF.
3. Methods
This descriptive cross-sectional study was conducted at Modarres Hospital in Tehran, where patients diagnosed with HF were selected in a non-random consecutive manner during 2023. The study protocol was carried out in accordance with the principles of the Declaration of Helsinki and the accepted regulations of the Shahid Beheshti University of Medical Sciences ethical committee (IR.SBMU.MSP.REC.1402.161). Written informed consent was obtained from each patient.
Demographic data were collected using a standardized questionnaire. The diagnosis of HF was made by a cardiologist based on the patients' medical records, including echocardiography reports. Patients were classified into three groups: HFrEF, HFmrEF, and HFpEF. The medications used by each patient were recorded in detail, including the type of drug, dosage, and category.
After collecting all the necessary data, we evaluated the patients' medications for compliance with the ESC guidelines in terms of drug category and dosage. The results were analyzed as compliance or non-compliance with the guidelines regarding the type and dosage of the drug received.
3.1. Statistical Analysis
The data were analyzed using SPSS version 22 software. Descriptive statistics were used to summarize the data, with mean and standard deviation reported for quantitative variables and number and percentage reported for qualitative variables. To compare parameters between two groups, the chi-square test was used for qualitative variables and the t-test for quantitative variables. A P-value of 0.05 or greater was considered statistically significant in all tests.
4. Results
4.1. Patient Characteristics
In this study, 97 patients with HF referred to Shahid Modarres Hospital (73 men and 24 women) with an average age of 64.3 ± 15.8 years (minimum 22 and maximum 92 years) were investigated.
As shown in Table 1, the study population had a high prevalence of comorbidities, with 57.7% of patients having hypertension, 39.2% having diabetes, and 18.6% having a history of substance abuse. Additionally, 76.3% of patients had abnormal ECG results, indicating potential cardiac issues. Furthermore, the study revealed that 71.1% of patients had a history of cardiac catheterization, and the severity of coronary artery disease was distributed as follows: Sixty-nine percent non-obstructive, 12.4% mild obstruction, 14.4% significant vessel disease, 18.6% two-vessel disease, and 21.6% three-vessel disease. These findings underscore the complexity of the patient population, characterized by a high burden of comorbidities and cardiac disease.
| Parameters | Absolute; Frequency (%) |
|---|---|
| Diabetes mellitus (yes) | 38 (39.2) |
| Hypertension (yes) | 56 (57.7) |
| Chronic kidney disease (yes) | 13 (13.4) |
| Family history (yes) | 16 (16.5) |
| Smoking (yes) | 33 (34) |
| Drug abuse (yes) | 18 (18.6) |
| Alcohol (yes) | 1 (1) |
| ECG (N/S) | 74 (76.3) |
| Catheterization history (yes) | 69 (71.1) |
| CAD | |
| Normal | 67 (69) |
| Mild | 12 (12.4) |
| Single vessel disease | 14 (14.4) |
| Two vessel disease | 18 (18.6) |
| Three vessel disease | 21 (21.6) |
Abbreviation: CAD, coronary artery disease.
The echocardiographic examination revealed significant abnormalities in the patient population. The majority of patients (79.4%) had IVC collapse of more than 50%. Furthermore, 5.2% of patients had pulmonary embolism (PE), which is a common complication of cardiac disease. The left ventricular (LV) size was abnormal in 51.8% of patients, with 32% having mild enlargement, 9.3% having moderate enlargement, and 10.3% having severe enlargement. The right ventricular (RV) size was abnormal in 41.6% of patients, with 12.4% having mild enlargement, 5.2% having moderate enlargement, and 2.1% having severe enlargement. Additionally, RV function was abnormal in 51.8% of patients, with 22.7% having moderate dysfunction and 8.2% having severe dysfunction. These findings suggest that the patient population has significant cardiac disease and may require further evaluation and treatment (Table 2).
| Parameters | Absolute; Frequency (%) |
|---|---|
| IVC size (abnormal) | 15 (15.5) |
| IVC collapse (> 50%) | 77 (79.4) |
| Pericardial effusion (yes) | 5 (5.2) |
| Left ventricle size | |
| Normal | 38 (39.2) |
| Mild | 31 (32) |
| Moderate | 9 (9.3) |
| Severe | 10 (10.3) |
| Right ventricle size | |
| Normal | 69 (71.1) |
| Mild | 12 (12.4) |
| Moderate | 5 (5.2) |
| Severe | 2 (2.1) |
| Right ventricle function | |
| Normal | 49 (50.5) |
| Mild | 16 (16.5) |
| Moderate | 22 (22.7) |
| Severe | 1 (1) |
| Diastolic dysfunction | |
| Normal | 2 (2.1) |
| Mild | 26 (26.8) |
| Moderate | 31 (32) |
| Severe | 8 (8.2) |
| Mitral valve stenosis | |
| Normal | 81 (83.5) |
| Severe | 1 (1) |
| Mitral valve regurgitation | |
| Normal | 3 (3.1) |
| Mild | 36 (37.1) |
| Moderate | 35 (36.1) |
| Severe | 8 (8.2) |
| Aortic valve stenosis | |
| Normal | 80 (82.5) |
| Mild | 2 (2.1) |
| Severe | 4 (4.1) |
| Aortic valve insufficiency | |
| Normal | 51 (52.5) |
| Mild | 21 (21.6) |
| Moderate | 12 (12.4) |
| Severe | 2 (2.1) |
Abbreviation: IVC, inferior vena cava.
The New York Heart Association (NYHA) functional classification of patients revealed that most patients (27.6%) were classified as NYHA class II, indicating moderate symptoms of heart disease. A significant proportion of patients (18.9%) were classified as NYHA class III, indicating severe symptoms of heart disease, while 5.2% were classified as NYHA class I, indicating no symptoms of heart disease. Only 1 patient (1%) was classified as NYHA class IV, indicating severe symptoms of heart disease and inability to perform any physical activity.
As shown in Table 3, the majority of patients (69.1%) were taking statins. Additionally, 38.1% of patients were taking ACE/ARB inhibitors. A significant proportion of patients (52.6%) were taking mineralocorticoid receptor antagonists (MRAs). Other medications used in the patient population included beta-blockers (39.2%), sacubitril/valsartan (14.4%), empagliflozin/dapagliflozin (44.3%), and diuretics (33.6%). Notably, ivabradine and hydralazine-isosorbide were not used in this patient population.
| Parameters | Absolute; Frequency (%) |
|---|---|
| Statin (D) | 67 (69.1) |
| ACE/ARB (D/BD) | 12/37 (12.4/38.1) |
| β-blocker (D/BD/QID) | 38/33/1 (39.2/34/1) |
| MRA (D/BD) | 51/5 (52.6/5.2) |
| Sacubitril/valsartan (D/BD) | 2/14 (2.1/14.4) |
| Empagliflozin/dapagliflozin (D/BD) | 43/1 (44.3/1) |
| Ivabradine | - |
| Hydralazine-isosorbide | - |
| Duretic (D/BD/TDS) | 10/30/1 (1.3/30.9/1) |
| Digoxin (D/BD) | 5/1 (5.2/1) |
Other demographic and clinical characteristics of the study population, including left ventricular ejection fraction (LVEF) and medication dosages, are presented in Table 4.
| Parameters | Min - Max | Mean ± SD |
|---|---|---|
| Weight (kg) | 30 - 98 | 73 ± 12.9 |
| Height (cm) | 146 - 190 | 168.5 ± 7.6 |
| EF (%) | 15 - 55 | 30.1 ± 9.2 |
| SPSP (mmHg) | 20 - 77 | 37.1 ± 12.3 |
| Statin dose (mg) | 10 - 50 | 34.3 ± 10 |
| ACE/ARB dose (mg) | 5 - 160.5 | 46.8 ± 40.1 |
| β-blocker dose (mg) | 1.25 - 100 | 13.7 ± 22 |
| MRA dose (mg) | 2.50 - 25 | 19.8 ± 6.4 |
| Sacubitril/valsartan dose (mg) | 2.50 - 50 | 37 ± 18.3 |
| Empagliflozin/dapagliflozin dose (mg) | 10 - 40 | 10.6 ± 4.5 |
Abbreviations: EF, ejection fraction; MRAs, mineralocorticoid receptor antagonists.
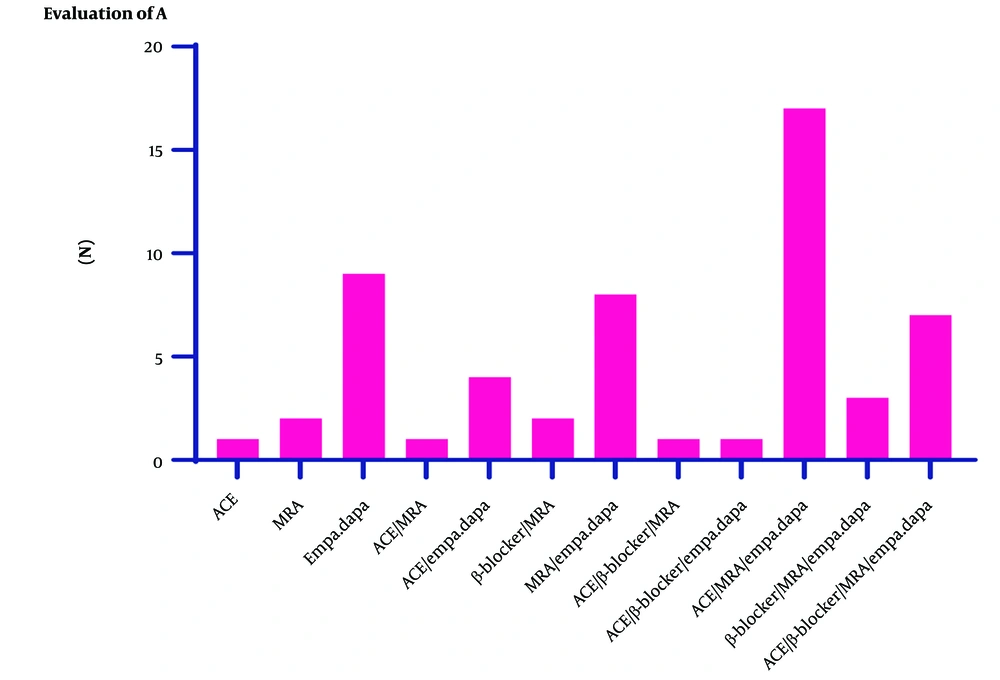
Consistency of the treatment of HF patients with ESC guidelines according to Figure 1, the treatment protocol of 41 patients (42.3%) was consistent with ESC guidelines. A total of 56 patients (57.7%) did not receive treatment according to the ESC guidelines.
The most non-compliance was observed in the use of ACE/ARB, MRA, and Empa/Dapa drug combinations.
ICD implantation was observed in 14 patients, while none of the patients received CRT or CRT-D devices.
The study population consisted of 97 individuals, with 56 patients (57%) being treated at Shahid Modarres Hospital and 41 patients (43%) visiting for the first time. Of the patients treated at Shahid Modarres Hospital, 60% received treatment in compliance with ESC guidelines. Among those who referred to our hospital for the first time, 30% received treatment in accordance with ESC guidelines, while 24% did not receive consistent treatment.
5. Discussion
Increasing the prevalence of HF patients remains one of the significant causes of mortality and hospitalization, and therefore a major burden for global healthcare systems, accounting for about 2.1% of the total healthcare budget (16). The ESC guidelines aim to assist health professionals in managing people with HF based on the best available evidence. Fortunately, we now have a large number of clinical trials that help better manage outcomes for people with HF. These guidelines provide practical, evidence-based recommendations focused on the diagnosis and treatment of HF (17). Due to the lack of studies on the compliance of treatment with the ESC guidelines for HF patients in Iranian hospitals, this study was conducted with the aim of evaluating the compliance of the treatment of HF patients in Shahid Modarres Hospital with the ESC guidelines.
The results of this study showed that the treatment protocol of 42.3% of patients was in compliance with the ESC guidelines. Among the patients who did not receive treatment according to the guidelines, 54.6% had a discrepancy in the type of drug, 2.1% had a discrepancy in the drug dosage, and 1% had discrepancies in both the type and dose of the drug. The most significant inconsistency was observed in the use of ACE/ARB, MRA, and Empa/Dapa drug combinations.
Of all patients, 14.4% had an ICD, and none had CRT or CRT-D devices. It was also found that 41 patients, equivalent to 43%, were visiting for the first time. Of the patients treated in Shahid Modarres Hospital, 60% were in compliance with the ESC guidelines. In contrast, only 30% of patients who referred to our hospital for the first time had treatment compliance with the ESC guidelines, with about 24% of these patients not receiving regular treatment.
Adherence to ESC guidelines is associated with better prognosis, improved clinical outcomes, fewer cardiovascular hospitalizations, and delayed rehospitalization (18-20). On the other hand, the complexity of the guidelines is an important obstacle to their implementation. The availability of HF treatment guidelines in a compact and accessible format is considered an essential factor in improving the implementation of the guidelines. However, many factors such as age, the cause of HF, and comorbidities affect the effectiveness of HF treatment (21).
The ESC guidelines recommend the use of three neurohormonal antagonists, including ACE-I/ARBs, beta-blockers, and MRAs, for the treatment of chronic HF with reduced EF (22). These drug treatments have an anti-remodeling effect and can improve survival (61-63, 70, 74-79) (20, 23, 24). In one study, overexpression of the angiotensin receptor was associated with an increase in the sympathetic nervous system, cardiac dysfunction, and premature death from heart problems. β1-adrenergic receptor hyperactivity induces cardiac remodeling that results in ventricular hypertrophy and apoptosis (25).
Several studies reported lower medication compliance than our study. Komajda et al. estimated that overall, less than one-third of patients received the recommended HF medications at target doses (26). Chang et al. showed that less than 25% of HF patients are treated with target doses of ACEI/ARBs and beta-blockers (27).
In a study including 2,834 HF patients from 27 Spanish hospitals, Crespo-Leiro et al. showed that overall, 92.6% of outpatients were taking ACE/ARBs, 93.3% were receiving beta-blockers, and 74.5% were receiving MRAs. The rate of non-compliance for the above drugs was 3.4%, 1.8%, and 19.0%, respectively (23). In our study, the most non-compliance was related to a combination of drugs, which indicates a general non-compliance in a patient, while a higher compliance was observed in patients on a single drug.
In another study by Chang et al., from a total of 1,509 patients hospitalized for acute HFrEF in 21 hospitals in Taiwan, the adherence to guidelines was lower than in our study (27), which is probably related to the smaller sample size in their study. With a larger sample size, we would likely have a more accurate estimate of the degree of treatment compliance in patients.
In the study by Sitepu and Hamdani, diuretics had the highest prescription rate at 89.7% (28), which was consistent with the MAHLER survey (29). Other studies also reported the use of diuretics as the most commonly prescribed drugs (30, 31). In our study, the high rate of prescription of diuretics may be due to the fact that most patients experienced shortness of breath, a common sign of congestion.
In the study by Rivera-Toquica et al., out of 2,528 patients, 1,384 (54.7%) with HFrEF were taking 88.9% beta-blockers, 72.3% ACEI/ARB, 67.9% MRA, and 13.1% ARNI. Furthermore, less than a third of all patients reached the target doses recommended by the European HF guidelines (32). However, in our study, the compliance rate was higher for beta-blockers and MRA. Observations of suboptimal dosing are also common in HF registries, indicating a clear gap between recommended doses and actual prescription practices. The reasons behind these suboptimal prescriptions are multifactorial, including the side effects of drugs and the lack of experience of the attending physician, which leads to clinical inertia (33, 34).
In our study, the lowest rate of treatment compliance was related to the combination of drugs in which SGLT2 inhibitors (SGLT2i) were included. Similar to ARNIs, SGLT2i represented a revolutionary advance in the field of HF, significantly reducing the risk of HF hospitalization and cardiovascular death in patients with HFrEF receiving optimal recommended therapy compared to those who received a placebo (35, 36). Although approximately 4 out of 5 patients with HFrEF are likely candidates for initiation of treatment with this class of drugs, studies suggest that there is underuse of these drugs (37). In this context, more real-world data on the use of SGLT2i in patients with HF, with and without T2DM, are needed to demonstrate the significant potential to reduce healthcare costs, morbidity, and mortality in these populations by promoting the prescription of these drugs in patients.
In several studies, the level of compliance and adherence to ESC guidelines was reported to be higher than in our study. In Komajda et al.'s study, the overall adherence of doctors to ESC treatment guidelines was 63% (29). A high rate of prescription of diuretics and ACE inhibitors was observed, similar to what has been reported in recent European studies. However, the administration of beta-blockers was observed in only half of the patients who should receive them according to ESC guidelines (38).
On the other hand, it has been shown that the expertise of the prescriber affects the rate of prescribing ACE inhibitors. Indeed, the high adherence to ACE inhibitor prescription observed here is likely due to the fact that the prescriptions were made by cardiologists. In the case of beta-blockers, reviews indicate that both prescriptions and daily doses are underused. Again, prescribing rates are significantly higher among cardiologists compared to non-cardiologists (29).
In our study, the reasons for non-adherence of doctors/patients to ESC guidelines were not evaluated. However, the results of other studies provide a comprehensive assessment of the barriers that physicians face in implementing guidelines for the treatment of HF. Patient factors can affect adherence through contraindications and poor tolerability of recommended medications. Indeed, guideline-recommended treatments have been observed to be under-prescribed in HF patients with lower body weight, who are generally weaker due to loss of adipose tissue, bone tissue, and impaired muscle mass. For patients living in nursing homes, the issue may be related to the increased risk of adverse drug reactions due to polypharmacy and comorbidities. However, results regarding the association between comorbidities and medication adherence are conflicting across studies. Some data suggest that having more comorbidities is associated with lower levels of adherence. Chronic kidney disease (CKD) is separately associated with non-adherence to ESC guidelines. Although these guidelines recommend beta-blockers (BB) as first-line therapy for all HFrEF patients, cardiologists seem reluctant to prescribe them in patients with underlying lung disease such as asthma or COPD (39).
As a cross-sectional analysis, it was impossible to assess changes in treatment over time. An important limitation of this study was the lack of evaluation of the potential causes of non-prescription of the evaluated drugs, which could include data related to side effects caused by the drug and other contraindications.
5.1. Conclusions
According to the results of this study, although the treatment compliance rate at Modarres Hospital is high, it still needs to be improved. Therefore, it is essential to consider the reasons for not prescribing HF drugs and address them if possible. Simply using the percentage of patients under treatment is a weak indicator of the quality of healthcare in HF. Thus, necessary measures to achieve the optimal dose for each patient should also be prioritized.