1. Background
Surgical repair of common congenital heart defects, such as atrial septal defect (ASD), ventricular septal defect (VSD), and partial atrioventricular canal (pAVC) with mitral valve cleft, has significantly improved in terms of safety and quality. These surgical repairs boast nearly 100% survival rates and success, with minimal complications and a reduced need for reoperations due to residual or recurrent defects (1-4). Mortality and morbidity following pediatric cardiac surgery have decreased in recent years. In asymptomatic children or those with minimal symptoms, elective surgical repair of heart defects is recommended. Evidence suggests that minimally invasive methods yield cardiac repair results comparable to traditional invasive approaches, while being less disruptive to lifestyle. These methods are associated with shorter hospital stays, rapid return to function through a muscle-sparing approach, improved aesthetics with a hidden scar, and enhanced quality of life (5-8).
Most open-heart procedures are traditionally performed via a complete median sternotomy. However, efforts have been made to minimize the invasiveness of this technique by reducing the incision size. The most common minimally invasive procedure is the upper partial sternotomy (mini-sternotomy). Despite potentially longer surgical times with the mini-sternotomy approach, improved outcomes have been reported, including reduced ventilation time, less bleeding, and shorter intensive care unit (ICU) and hospital stays (9, 10). Minimally invasive heart surgery for both children and adults has gained attention as a means to decrease ICU costs and hospital stays, while improving cosmetic outcomes. Shorter recovery times, pain reduction, and faster recovery of respiratory function are particularly important in children, although studies in this area are limited (11-13).
The midline incision offers several advantages, such as avoiding pericardial incisions near the phrenic nerve and eliminating the need for myocutaneous flaps that can aid in skin denervation. However, the disadvantages of complete midline sternotomy are primarily cosmetic, due to scar length and potential chest wall deformities, which are significant concerns for growing children. Although minimally invasive cardiac surgery is performed worldwide, it carries its own risks. Restricted access to the heart can result in suboptimal surgical outcomes (14). Consequently, there remains some uncertainty regarding the superiority of these procedures, and whether mini-sternotomy offers additional advantages over full sternotomy is not well established. This uncertainty may stem from the lack of prospective randomized clinical trials comparing minimally invasive procedures to conventional incisional methods (15).
2. Objectives
Therefore, this clinical trial was designed to investigate the outcomes of open-heart surgery in children using full versus mini-sternotomy incisions.
3. Methods
Participants in this single-blind randomized clinical trial (where the patient and parents were unaware of the surgical method) comprised 78 patients aged 1 to 25 years who were candidates for open-heart surgery. These patients were identified after referral to the Heart Clinic or Emergency Department of Modarres Hospital, Tehran, Iran, during the period 2023 - 2024. Patients undergoing valve replacement, septal defect repair, or other types of cardiac surgery were included in the study. Patients without inflammatory, infectious, autoimmune, malignant, renal, hepatic, or thyroid diseases, diabetes, or a history of previous surgery in the chest area were eligible for inclusion. The occurrence of complications such as bleeding resulting from surgery or the need to expand the surgical incision during the operation were exclusion criteria. The patients' demographic and clinical information was recorded at the time of admission. Based on preliminary study data (16), the primary outcome of the study (i.e., pain level in children in the first 24 hours) and the parameters considered, a sample size of 74 patients was initially calculated to achieve a trial power of 80% and an alpha level of 5%. Considering a 5% probability of dropout, the final number of 78 patients was included. Random assignment of patients to two groups — group A (patients undergoing full sternotomy) and group B (patients undergoing mini-sternotomy) — was performed. For this purpose, the website https://www.Randomization.com was used for random assignment, and then all patients underwent surgery. The informed consent form was signed by the patients or their parents. This study was initiated after obtaining ethics code IR.SBMU.MSP.REC.1402.619, trial ID 75977, and IRCT registration code (IRCT20230626058586N4) from the International Center for Clinical Trials Registration of Iran.
3.1. Incision Procedures
For mini-sternotomy, the skin was incised approximately 8 cm from the midpoint between the suprasternal notch and the sternal angle to the level of the fourth intercostal space. The manubrium was divided in the midline from the suprasternal notch downwards and then into the right fourth intercostal space. For full sternotomy, a skin incision was made between the suprasternal notch and the xiphoid process, and the sternum was divided in the midline from the suprasternal notch to the xiphoid process.
3.2. Evaluations of Outcomes
In this study, the recovery rate encompasses postoperative pain, analgesic use, wound infection, antibiotic use, wound dehiscence, ventilation time, and the length of ICU and hospital stay. The primary outcome was pain and analgesic use in patients, assessed using a facial pain assessment tool (17). Secondary outcomes included infection rate, antibiotic therapy, surgical site debridement, complications (such as pneumonia, pleural effusion, atelectasis, atrial fibrillation), inotrope administration (including norepinephrine and milrinone), mortality, bypass time, ventilation time, extubation time, ICU and hospital length of stay, bleeding rate, and transfusion rate. Analgesic consumption, infection, antibiotic therapy, and surgical site dehiscence were evaluated in three sessions: Zero - 6 hours post-surgery, 24 - 48 hours post-surgery, and at discharge (first, second, and third sessions).
3.3. Statistical Analysis
The data were analyzed using SPSS version 22 software. Quantitative parameters were reported as mean and standard deviation (SD), while qualitative parameters were presented as number and percentage. In the analytical section, qualitative data comparisons were performed using Fisher's exact test or chi-square test. Quantitative data were assessed for normal distribution compliance using the Kolmogorov-Smirnov test and then compared using the t-test. All analysis results were considered significant at a level of 0.05, with 95% confidence intervals.
4. Results
4.1. Comparison of Demographic and Clinical Factors Between Two Groups
As shown in Table 1, demographic and clinical factors, including age, gender, BMI, and type of surgery, were compared between the mini-sternotomy and full sternotomy groups. These parameters did not differ significantly between the groups, indicating that the groups were well matched.
| Parameters | Full Sternotomy (n = 39) | Mini Sternotomy (n = 39) | Total Patients (n = 78) | P-Value b |
|---|---|---|---|---|
| Gender (male) | 5 (12.8) | 4 (10.3) | 50 (64.1) | 0.47 |
| Type of surgery | 0.28 | |||
| PS | 5 (12.8) | 4 (10.3) | 9 (11.5) | |
| PVR | 5 (12.8) | 5 (12.8) | 10 (12.8) | |
| TOF | 8 (10.3) | 3 (7.3) | 5 (12.8) | |
| AVR | 5 (12.8) | 4 (10.3) | 9 (11.5) | |
| ASD | 12 (30.8) | 14 (35.9) | 26 (33.3) | |
| VSD | 3 (7.7) | 3 (7.7) | 6 (7.7) | |
| PDA closure | 3 (7.7) | 0 (0) | 3 (3.8) | |
| PA banding | 3 (7.7) | 0 (0) | 3 (3.8) | |
| CoA | 2 (5.1) | 0 (0) | 2 (2.6) | |
| MVR | 2 (5.1) | 0 (0) | 2 (2.6) | |
| Age (y) | 6.89 ± 6.14 | 6.53 ± 7.87 | 6.71 ± 7.02 | 0.82 |
| BMI (Kg/m2) | 23.76 ± 3.47 | 23.71 ± 23.71 | 23.74 ± 3.32 | 0.94 |
Abbreviations: PS, pulmonary stenosis; PVR, pulmonary valve replacement; TOF, tetralogy of Fallot; AVR, aortic valve repair; ASD, atrial septal defect; VSD, ventricular septal defect; PDA, patent ductus arteriosus; PA, pulmonary artery; CoA, coarctation of the aorta; MVR, mitral valve repair; BMI, Body Mass Index.
a Values are expressed as No. (%) or mean ± SD.
b P-value less than 0.05 considered as significant.
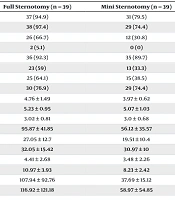
4.2. Comparison of Intraoperative and Postoperative Parameters in Patients of the Two Groups
In this part of the study, clinical and laboratory parameters related to the recovery of patients between the two groups were compared (Table 2). All patients in both groups received antibiotic therapy during the first session. Upon comparing other parameters, it was observed that the amount of analgesic consumption in the second and third rounds, antibiotic therapy in the third round, surgical complications, pain score in the first round, bypass time, ventilation time, length of hospital stay, bleeding rate, and transfusion rate were significantly higher in patients undergoing full sternotomy.
| Parameters | Full Sternotomy (n = 39) | Mini Sternotomy (n = 39) | Total Patients (n = 78) | P-Value b |
|---|---|---|---|---|
| First dose analgesic (yes) | 37 (94.9) | 31 (79.5) | 68 (87.2) | 0.08 |
| Second dose analgesic (yes) | 38 (97.4) | 29 (74.4) | 67 (85.9) | 0.007 |
| Third dose analgesic (yes) | 26 (66.7) | 12 (30.8) | 38 (48.7) | 0.003 |
| Third dose infection (yes) | 2 (5.1) | 0 (0) | 2 (2.6) | 0.49 |
| Second dose antibiotic therapy (yes) | 36 (92.3) | 35 (89.7) | 71 (91) | 0.99 |
| Third dose antibiotic therapy (yes) | 23 (59) | 13 (33.3) | 36 (46.2) | 0.04 |
| Complication occurrence (yes) | 25 (64.1) | 15 (38.5) | 40 (51.3) | 0.04 |
| Inotrope administration (yes) | 30 (76.9) | 29 (74.4) | 59 (75.6) | 0.99 |
| First dose pain Score | 4.76 ± 1.49 | 3.97 ± 0.62 | 5.15 ± 0.99 | 0.003 |
| Second dose pain score | 5.23 ± 0.95 | 5.07 ± 1.03 | 4.37 ± 2.1 | 0.49 |
| Third dose pain Score | 3.02 ± 0.81 | 3.0 ± 0.68 | 3.01 ± 0.74 | 0.88 |
| Bypass time (minutes) | 95.87 ± 41.85 | 56.12 ± 35.57 | 76 ± 43.46 | 0.0001 |
| Ventilation time (h) | 27.05 ± 12.7 | 19.51 ± 10.4 | 23.28 ± 12.14 | 0.005 |
| Extubation time (h) | 32.05 ± 15.42 | 30.97 ± 10 | 31.51 ± 12.92 | 0.71 |
| ICU stay duration (d) | 4.41 ± 2.68 | 3.48 ± 2.26 | 3.94 ± 2.51 | 1.0 |
| Hospital stay duration (d) | 10.97 ± 3.93 | 8.23 ± 2.42 | 9.6 ± 3.52 | 0.0001 |
| Bleeding volume (mL) | 107.94 ± 92.76 | 37.69 ± 15.12 | 72.82 ± 74.9 | 0.0001 |
| Transfusion volume (mL) | 116.92 ± 121.18 | 58.97 ± 54.85 | 87.94 ± 87.89 | 0.008 |
a Values are expressed as No. (%) or mean ± SD.
b P-value less than 0.05 considered as significant.
5. Discussion
With the decrease in mortality and complications following pediatric congenital heart surgery, variables such as pain and discomfort, postoperative recovery time, cosmetic outcomes, and total length of hospital stay have become primary goals for improving outcomes. This study was designed to investigate and compare the recovery rates of patients undergoing mini-sternotomy and full sternotomy. According to the main results, there was no infection, surgical site dehiscence within the first 48 hours post-surgery, or mortality in patients with either complete or partial incisions. Additionally, all patients in both groups received antibiotic therapy within the first 6 hours. Comparison of other recovery parameters showed that analgesic consumption in the first 6 and 24 hours, antibiotic therapy at discharge, surgical complications, pain score in the first 6 hours, bypass time, ventilation time, length of hospital stay, bleeding rate, and transfusion rate were significantly higher in patients undergoing full sternotomy.
Faster recovery with less respiratory function impairment and reduced pain following less invasive incisions has been reported, although no prospective studies have been conducted to support this claim (18-21). The mini-sternotomy procedure allows for standardized instrumentation and requires the same surgical skills as the conventional open procedure (3, 22-25). The primary concern with any minimally invasive procedure is safety, and mini-sternotomy has the advantage of being easily and quickly convertible to a full sternotomy if needed. It has been performed in a wide range of patients, from 6 months of age to adolescents and adults (22-25).
Consistent with our findings, a study by Luo et al. reported that bypass time, ICU stay, and duration of ventilation were similar in both full sternotomy and mini-sternotomy cases. They found that operative time was shorter in mini-sternotomy cases compared to the full sternotomy group. In the first 24 hours post-surgery, the mini-sternotomy group had a lower drainage volume than the total sternotomy group, but there was no significant difference in blood transfusion between the two groups, and the length of hospital stay was shorter in the mini-sternotomy cases compared to the total sternotomy group (26).
A meta-analysis including 2054 subjects with aortic valve replacement (AVR) surgery via partial upper sternotomy compared with 2532 cases with total sternotomy did not show any difference in early mortality between the two surgical procedures (27). This suggests that AVR can be safely performed via mini-sternotomy in well-equipped centers. Thus, in addition to the advantages of the mini-sternotomy incision, it appears to be sufficiently safe and equivalent to a total sternotomy.
Our results indicated that bypass time was longer in patients undergoing full sternotomy, which contrasts with other studies. One study found that cardiopulmonary bypass times were longer in the mini-sternotomy group (7.9 vs. 11.5 minutes) (28).
According to the results of the study by Konstantinov and Buratto, although mini-sternotomy provided results comparable to full sternotomy, the mean bypass duration was 9 minutes longer due to inferior vena cava (IVC) cannulation and decannulation, and there were no late complications in either group (29). Hancock et al. also demonstrated that mini-sternotomy patients had significantly longer bypass times and worse 4-week lung function. However, lung function at 12 weeks and rates of adverse events did not differ between groups. In this study, full sternotomy was ultimately found to be more cost-effective (14). Thus, it appears that the technique used in mini-sternotomy affects bypass time, which differed in our study.
Regarding ventilation time, ICU and hospital stay, transfusion rate, and drainage volume and bleeding, the results of the studies generally align with the present study. In the study by Brown et al., the mean ventilation time was shorter in the minimally invasive methods (difference of 2.1 hours). The ICU stay duration was also shorter in the mini-sternotomy group (11 hours), as well as the hospital stay (1 day) (16, 28). Regarding the amount of bleeding and the need for transfusion, one study showed that the volume of chest drainage over 24 hours was lower in the mini-sternotomy cases (28). The reduced blood loss may be related to reduced surgical trauma. Another study indicated that mini-sternotomy was not superior to conventional sternotomy in terms of the need for RBC transfusion within 7 days after surgery. Analysis of secondary endpoints revealed a significant difference in the volume of non-red blood cell transfusions. Mini-sternotomy resulted in a relative reduction in the volume of chest drainage (14).
One of the most important outcomes examined in the present study was the assessment of pain and analgesic use in the two groups of patients. Studies in this area have had conflicting results. Some studies have shown that patients experience less pain after mini-sternotomy (30-33). This may be due to the less sternal traction required in partial sternotomy. Furthermore, the presence of sternal fractures may play an important role in initial postoperative pain levels. The results of the study by Laussen et al. indicated that the mini-sternotomy procedure did not change the postoperative pain level. In this study, patients aged between 5 to 16 years. At 6-week follow-up, all patients had essentially returned to full activity and resumed school. However, it is unclear whether an earlier assessment after discharge would have detected differences between the two groups (16). There was no difference in the need for additional postoperative analgesics or the incidence of vomiting between the two groups. The age range studied in this study was different from ours, and the pain assessment tools were different, which may account for the different conclusions between the two studies.
In some studies, the level of discomfort after a standard midline full sternotomy was not severe. This could be attributed to the cartilaginous nature of the sternum, which allows for natural rib movement to expand the sternum. The low level of discomfort observed in full sternotomy cases makes it challenging to demonstrate an advantage for a minimally invasive procedure in this area. Although few studies have reported on pain and pain management strategies have not been standardized, in both full and mini-sternotomy procedures, the sternum should be opened gradually to avoid unnecessary bone fractures. Furthermore, other investigations have concluded that mini-sternotomy does not provide a significant advantage over full sternotomy. In one study, 45 patients (2.6%) who underwent a superior mini-sternotomy required conversion to a full sternotomy due to bleeding, ventricular arrhythmias, ventricular dysfunction, or other conditions. Although the rate of incision type conversion remains low, the need for conversion may be associated with a significantly increased mortality rate (34).
Alternative access methods for congenital heart surgery have been established mainly to improve cosmetic outcomes (35, 36). Although these techniques are particularly recommended for female patients older than 10 years, they have been used for children of all ages. Cosmetic outcomes evaluated in the immediate postoperative period have been acceptable, although some incision-related complications have been reported. There are reports of phrenic nerve injury after ASD closure via right anterior thoracotomy (37, 38). Incorrect development of the pectoralis major muscle and breast has been described after a transverse inframammary incision, accompanied by paraesthesia in the peribreast tissue (39, 40). On the other hand, the advantages of a midline incision include avoiding pericardial incisions near the phrenic nerve. The disadvantages of a complete midline sternotomy are mainly cosmetic, due to scar size and possible chest wall deformities, which are significant concerns for children.
A prospective study found no significant difference in the recovery of patients undergoing a complete sternotomy and a minimally invasive incision for ASD surgery in children. Surgery with a mini-sternotomy approach was not associated with increased operative or postoperative complications. However, since the incidence of complications for this surgical procedure is generally very low, a much larger sample size is necessary to compare specific outcomes. The studies mentioned the need for incision extension as a possible disadvantage of this procedure, but in our study, no patients required incision extension to improve surgical access.
The sample size of this study was relatively small, affecting the generalizability of our findings. It was also a single-center study with a relatively small sample size and short follow-up period, which may have reduced the power to detect small differences in mortality, complications, and fewer safety events. Additionally, many factors can affect postoperative recovery, which may have unintentionally influenced the results of this study. Despite attempts to examine important demographic aspects related to the effect of incision type, some determinants, such as other medications taken by the patient, were not considered. It is recommended that these factors be considered in future studies.
5.1. Conclusions
Mini-sternotomy is as safe and effective as full sternotomy in pediatric cardiac surgery. Additionally, this incision reduces initial pain and bleeding, shortens hospital stay, and provides better cosmetic results. A comprehensive evaluation of patients undergoing open-heart surgery in a large, multicenter cohort, followed prospectively by a focused study of the consequences of full sternotomy, is recommended.