1. Background
In 1917, "Bangungut" was identified as a sudden nocturnal death in healthy Filipinos, with no autopsy evidence. It was later linked to ventricular fibrillation by the Brugada brothers in 1992 (1, 2). Brugada syndrome (BrS) is an inherited cardiac arrhythmia disorder associated with a high risk of sudden cardiac death, primarily affecting young and seemingly healthy individuals (3, 4). It is characterized by distinct electrocardiogram (ECG) abnormalities, such as right bundle branch block (RBBB) and coved-type ST-segment elevation in leads V1 to V3 (5, 6). The syndrome can present a range of symptoms, from being asymptomatic to experiencing life-threatening cardiac events like ventricular tachyarrhythmia and sudden cardiac death (5, 6).
The prevalence of BrS is estimated to be 0.36% in Europe and the United States, 1.4% in Japan, and 1.8% in Thailand (7-9). Brugada syndrome is more common in young males than females, with a ratio of 8:1 (10). The mean age of patients with BrS is between 40 and 45 years (7, 10). This condition primarily arises from genetic abnormalities, particularly mutations in the SCN5A gene, which affect cardiac sodium channels by causing a loss of function in the alpha-subunit of these channels, leading to repolarization disturbances. These disturbances result in abnormalities such as RBBB, ST-segment elevation, and inverted T waves in the right precordial leads due to an increased magnitude of the right epicardial action potential notch. This leads to reduced calcium current availability, delaying the second upstroke and onset of phase 3, thereby prolonging the action potential (11-15).
Patients with BrS often exhibit symptoms during periods of high vagotonic activity, such as sleep, rest, after large meals, or during fever. There is potential phenotypic overlap with other conditions like cardiac conduction disease (CCD), sinus node dysfunction, and long QT syndrome (LQTS) due to similar molecular mechanisms (10, 16). Pharmacological provocation tests using sodium channel blockers like flecainide or ajmaline are critical for confirming these latent patterns (7, 17, 18). These pharmacological agents are frequently used to unmask concealed BrS patterns for definitive diagnosis.
Increasingly, attention is focused on QT interval measurements — their prolongation and dispersion — as they are considered predictive of arrhythmic risk in BrS patients (5, 7, 19). The goal is to guide management strategies, such as the use of implantable cardioverter-defibrillators (ICDs) for individuals identified at high risk (5, 10).
2. Objectives
This study aims to elucidate the effects of flecainide testing on both the QT interval and QT dispersion within patients diagnosed with or suspected of having BrS. By correlating these findings with clinical presentations, the research seeks to enhance the understanding of flecainide’s role in the diagnostic and prognostic evaluation of arrhythmogenic conditions.
3. Methods
3.1. Study Design
This retrospective study aimed to evaluate the differences in ECG parameters, including the QT interval, QTc interval, QT dispersion, and RR interval, between patients with and without BrS after the administration of flecainide. The study included 20 patients diagnosed with BrS (10 patients in group 1) and those who did not meet Brugada criteria (10 patients in group 2). Patient data were obtained from hospital records between 2007 and 2011, following approval by the local ethics committee under reference number IUMS.REC.1393.878.
3.2. Patient Selection
Patients were selected based on clinical suspicion of BrS and the administration of a flecainide challenge test during the study period. The inclusion criteria required all patients to have undergone a thorough clinical evaluation, including serum tests, echocardiography, and ECG monitoring. The groups were defined as follows:
Group 1: Brugada syndrome (n = 10) – these patients displayed the type-1 Brugada ECG pattern after flecainide administration, characterized by a coved ST-segment elevation ≥ 2 mm followed by a negative T wave in the right precordial leads.
Group 2: Non-Brugada (n = 10) – These patients did not exhibit the characteristic Brugada ECG pattern.
Key exclusion criteria included significant renal or electrolyte abnormalities and major structural heart disease, as confirmed by echocardiographic assessments.
3.3. Drug Administration and Electrocardiogram Monitoring
All patients received a 300 mg oral dose of flecainide, following standard protocols for the flecainide challenge test. Electrocardiogram monitoring was conducted for a period of 24 hours post-administration, with data recorded at the following intervals: (A) fifteen minutes, 30 minutes, 60 minutes, 90 minutes, and then every hour for the first 6 hours, followed by every 2 hours until the 24-hour mark; (B) ECG measurements were taken at these intervals for all patients, and all recordings were calibrated to 25 mm/s for speed and 10 mm/mV for amplitude.
3.4. Electrocardiogram Lead Placement
Electrocardiogram data were recorded using the following lead configurations:
1. Standard precordial leads (left precordial): A traditional 12-lead ECG was performed, with V1 and V2 placed in the 4th intercostal space (ICS) for standard analysis of the right precordium.
2. Right Precordial Leads: Additional leads were positioned at the 3rd ICS for V1 and V2, and V3R and V4R were placed to assess the right-sided heart activity more specifically.
3.5. Electrocardiogram Parameters
The following ECG parameters were calculated and compared between the two groups:
1. QT interval: The interval from the beginning of the QRS complex to the end of the T wave was measured across all leads.
2. QTc interval: The corrected QT interval was calculated using Bazett’s formula.
Where RR is the interval between successive R waves in the ECG in seconds, and QT is in milliseconds. The difference between the longest and shortest QT interval observed across precordial leads. The time between successive R waves, which was assessed to analyze heart rate variability.
3.6. Statistical Analysis
Data was analyzed using SPSS version 22. The analysis aimed to compare the QT interval, QTc interval, QT dispersion, and RR interval between the two groups (Brugada positive vs. non-Brugada) for both left and right precordial leads. Statistical tests performed included: (A) descriptive statistics to summarize patient demographics and baseline ECG characteristics; (B) independent samples t-test for normally distributed variables to compare mean differences between the groups. The Mann-Whitney U test was utilized for non-normally distributed data to compare median values between groups, while paired sample t-tests were employed to compare ECG parameters within each group between left and right precordial leads. A P-value of less than 0.05 was considered statistically significant for all comparisons.
3.7. Key Variables and Comparisons
The study focused on comparing the following variables between group 1 (BrS) and group 2 (Non-Brugada):
1. QT interval: Analyzing the absolute QT interval and its dispersion in both left and right precordial leads.
2. QTc interval: Evaluating the corrected QT interval in both groups to account for heart rate variations.
3. QT dispersion: Identifying differences in the spread of the QT interval across the leads, comparing right vs. left precordial leads.
4. RR interval: Analyzing heart rate differences based on RR interval data and their possible association with arrhythmogenic risk.
3.8. Positive Test Definition
A positive Brugada test was defined by the presence of the type-1 Brugada ECG pattern after flecainide administration in group 1. In group 2, no Brugada-type pattern was observed, and these patients served as the control group for comparison.
3.9. Ethical Considerations
Due to the retrospective nature of the study, no direct interventions were performed on patients. Patient data were coded to ensure confidentiality, and no personal identifiers were used in the analysis.
4. Results
In this study, 20 patients, comprising 19 males and 1 female, were examined. The patients were divided into two equal groups: Those with BrS and those without, with an average age of 36.23 ± 16.02 years, ranging from 16 to 70 years.
4.1. Overview of Electrocardiogram Findings
Initially, we compared the ECG parameters of all patients, both with and without BrS, before and after the flecainide oral administration. As shown in Table 1, the only significant difference observed was in the right QT interval (P = 0.04), indicating a notable change post-administration. Other parameters such as left QT, left RR, left QTD, right RR, and QTc intervals did not show significant differences.
| Parameters | Before Oral Administration | After Oral Administration | P-Value |
|---|---|---|---|
| Left QT | 396.00 ± 39.25 | 410.00 ± 60.34 | 0.14 |
| Left RR | 857.45 ± 125.04 | 880.00 ± 256.04 | 0.77 |
| Left QTD | 28.00 ± 16.41 | 33.10 ± 18.48 | 0.26 |
| Right QT | 386.25 ± 44.25 | 415.00 ± 61.75 | 0.04 a |
| Right RR | 838.75 ± 126.37 | 878.75 ± 220.84 | 0.49 |
| Right QTD | 35.00 ± 8.94 | 35.00 ± 8.94 | - |
| Left QTc | 429.45 ± 34.53 | 437.95 ± 40.48 | 0.45 |
| Right QTc | 423.00 ± 37.53 | 446.31 ± 50.12 | 0.12 |
Comparison of Electrocardiogram Findings in Both Groups Before and After Oral Administration of Flecainide
4.2. Brugada Syndrome Patients
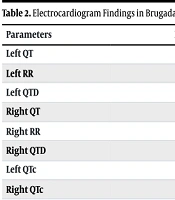
For patients with BrS, the ECG findings before and after the flecainide oral administration were compared. As detailed in Table 2, there was an increase in the left QT, left RR, right QT, right RR, and right QTc intervals post-administration, although these changes were not statistically significant (P > 0.05). The right QTD remained unchanged, while the left QTD and left QTc decreased, but again, these changes were not significant (P > 0.05).
| Parameters | Before Oral Administration | After Oral Administration | P-Value |
|---|---|---|---|
| Left QT | 420.00 ± 38.87 | 436.00 ± 71.67 | 0.34 |
| Left RR | 880.90 ± 120.95 | 950.00 ± 331.89 | 0.64 |
| Left QTD | 36.00 ± 15.77 | 34.00 ± 21.18 | 0.79 |
| Right QT | 410.00 ± 46.59 | 435.00 ± 81.24 | 0.33 |
| Right RR | 865.00 ± 130.38 | 950.00 ± 277.74 | 0.36 |
| Right QTD | 37.50 ± 7.07 | 37.50 ± 7.07 | - |
| Left QTc | 449.00 ± 28.30 | 445.50 ± 34.15 | 0.79 |
| Right QTc | 441.62 ± 34.47 | 449.25 ± 54.95 | 0.88 |
Electrocardiogram Findings in Brugada Syndrome (Group 1) Patients Before and After Oral Administration of Flecainide
4.3. Non-brugada Patients
In contrast, for patients without BrS, significant changes were observed in several ECG parameters after the flecainide administration, as shown in Table 3. The left QTD, right QT, and right QTc intervals increased significantly, with P-values of 0.02, 0.03, and 0.02, respectively. This suggests that flecainide has a more pronounced effect on these parameters in non-Brugada patients.
| Parameters | Before Oral Administration | After Oral Administration | P-Value |
|---|---|---|---|
| Left QT | 372.00 ± 21.49 | 384.00 ± 32.38 | 0.21 |
| Left RR | 834.00 ± 130.99 | 810.00 ± 131.74 | 0.26 |
| Left QTD | 20.00 ± 13.33 | 32.20 ± 16.450 | 0.02 a |
| Right QT | 362.50 ± 27.12 | 395.00 ± 25.63 | 0.03 a |
| Right RR | 812.50 ± 125.09 | 807.50 ± 125.55 | 0.86 |
| Right QTD | 32.50 ± 10.35 | 32.50 ± 10.35 | - |
| Left QTc | 409.90 ± 29.44 | 430.40 ± 46.54 | 0.19 |
| Right QTc | 404.37 ± 32.21 | 443.37 ± 48.42 | 0.02 a |
Electrocardiogram Findings in Non-Brugada Patients (Group 2) Before and After Oral Administration Flecainide
4.4. Post-flecainide Oral Administration Electrocardiogram Comparison in Two Groups
After the flecainide oral administration, a comparison of ECG findings between the two groups revealed significant differences in the right and left QT intervals and the right and left QTD intervals, as illustrated in Table 4. These differences highlight the inherent variations in ECG parameters between patients with and without BrS after oral administration of flecainide.
| Parameters | Group 1 | Group 2 | P-Value a |
|---|---|---|---|
| Left QT | 420.00 ± 38.87 | 372.00 ± 21.49 | 0.002 |
| Left QTD | 36.00 ± 15.77 | 20.00 ± 13.33 | 0.02 |
| Right QT | 410.00 ± 46.59 | 362.50 ± 27.12 | 0.05 |
| Right QTD | 37.50 ± 7.07 | 32.50 ± 10.35 | 0.007 |
Significant Electrocardiogram Findings After Oral Administration Flecainide
In summary, the study demonstrates that flecainide oral administration significantly affects certain ECG parameters, particularly in non-Brugada patients. The significant increase in the right QT interval across all patients and the notable changes in the left QTD, right QT, and right QTc intervals in non-Brugada patients underscore the differential impact of flecainide based on the presence of BrS. These findings are crucial for understanding the electrophysiological effects of flecainide and tailoring treatment strategies for patients with and without BrS.
5. Discussion
Brugada syndrome is a major cause of sudden cardiac death, especially in young, otherwise healthy individuals, and has spurred significant research for improved diagnostic approaches. It is characterized by RBBB and ST-segment elevation (type 1 Brugada pattern) in the precordial leads V1-V3 (2, 5, 20, 21). These ECG abnormalities may not always be evident at baseline, necessitating drug-provocation tests using sodium channel blockers like flecainide or ajmaline to uncover concealed forms of BrS (2, 5, 7).
The genetic basis of BrS is linked to mutations in the SCN5A gene, encoding the cardiac sodium channel NaV1.5. These mutations disrupt sodium current (INa) conduction, predisposing affected individuals to arrhythmogenesis (10, 11, 16). Brugada syndrome represents a high-stakes condition with potentially fatal consequences; thus, defining and refining diagnostic measures, especially with pharmacological challenges, remains vital.
Flecainide, a potent class IC antiarrhythmic agent, is highly effective in unmasking latent BrS. It works by blocking sodium currents, exacerbating the preexisting conduction delays caused by BrS mutations, thereby highlighting characteristic ECG changes (5, 6, 22, 23).
In our study, the administration of flecainide significantly prolonged the right QT interval from 386.25 ± 44.25 ms to 415.00 ± 61.75 ms (P = 0.04). This is consistent with the findings of Pitzalis et al. (5), who demonstrated that flecainide induced significant increases in the QT interval in leads V1 and V2, closely associated with BrS diagnosis. Specifically, their study showed a QTc increase in V1 by 78.2 ± 35.5 ms and in V2 by 107.1 ± 43.8 ms, both with P < 0.01 (5).
The capacity of flecainide to elicit BrS diagnostic patterns underscores its diagnostic utility, particularly in cases where baseline ECG findings are nonspecific. It is particularly important in differentiating true BrS from phenocopies induced by other causes, such as electrolyte disturbances or structural heart disease (5). One of the hallmark findings in BrS is QT interval prolongation post-sodium channel blocker administration. Flecainide-induced changes primarily manifest in the right precordial leads, where delayed myocardial depolarization is most prominently seen (24).
The study by Pitzalis et al. (5) observed prolonged QTc intervals in patients with confirmed BrS following flecainide administration, with an ROC curve area of 0.99, indicating high predictive accuracy for BrS (5). Your findings align closely with these observations, highlighting that right QT prolongation post-flecainide (P = 0.04) is a robust indicator of underlying Brugada electrophysiological abnormalities. Similarly, another study demonstrated that approximately 75% of patients undergoing a sodium channel blocker challenge exhibited the diagnostic coved-type ST-segment elevation (P < 0.01). This early study established the groundwork for subsequent uses of drug provocation as a diagnostic test (2).
Ajmaline, another sodium channel blocker, is frequently used as an alternative to flecainide (18, 25). However, its utility may vary based on the reliability of the ECG changes elicited. Thapanasuta et al. (7) investigated the efficacy of ajmaline in unmasking arrhythmogenic changes by examining the T-peak to T-end (TpTe) interval. Their findings revealed no significant correlation between ajmaline-induced TpTe changes and Brugada pattern emergence (P > 0.05). In contrast, flecainide administration resulted in more reproducible and robust changes in our study, especially concerning QT interval prolongation. These observations highlight a potential edge for flecainide over ajmaline in specific cases where diagnostic sensitivity is paramount. However, both drugs remain essential tools in clinical practice given interindividual variability in response (7).
Additionally, the variability in results might be influenced by underlying genetic factors. Patients with specific Brugada-associated mutations, such as SCN5A variants, may exhibit heightened sensitivity to either drug. This underscores the importance of tailoring pharmacological challenges based on a combined clinical-genetic assessment (10). The genetic underpinnings of BrS significantly influence the outcomes of sodium channel blocker testing. A landmark study by Zumhagen et al. emphasized that 75% of Brugada-positive patients with SCN5A mutations demonstrated significant ECG changes during sodium channel blocker administration (P < 0.01) (10). Flecainide’s diagnostic efficacy particularly stands out in such cases because of its specific ability to amplify existing conduction abnormalities caused by these mutations.
Our study demonstrated that flecainide administration led to significant QT prolongation, suggesting a possible underlying genetic predisposition among the tested population. This aligns with findings by Zumhagen et al., advocating for genetic screening alongside drug provocation tests to better stratify patients at risk of life-threatening arrhythmias (10). The diagnostic role of sodium channel blockers extends beyond confirmation of BrS to broader clinical applications. For instance, Pitzalis et al. highlight the use of QT interval measurements not only for diagnostic purposes but also for predicting outcomes in high-risk populations (5).
Flecainide, with its consistent ability to provoke QT prolongation and coved-type ST-segment elevations, remains one of the most reliable pharmacological provocators. It has a distinct edge in diagnosing concealed Brugada patterns, as seen in our findings and corroborated by multiple studies. However, ajmaline continues to play a complementary role, particularly in patients where flecainide may lead to false-negative results or adverse reactions (7).
The integration of genetic screening further enhances the diagnostic accuracy and risk stratification in BrS. As emphasized by Zumhagen et al., tailoring diagnostic pathways based on SCN5A mutations or other genetic variants moves clinical practice closer to precision medicine (10).
5.1. Conclusions
The study underscores the importance of using flecainide to induce specific ECG changes that aid in the diagnosis of BrS. The integration of genetic testing alongside pharmacological assessment highlights a comprehensive approach to managing this complex condition. By refining diagnostic criteria and leveraging genetic insights, healthcare providers can enhance patient management, ultimately improving prognosis for those at risk.