1. Introduction
Isolated unilateral absence of the pulmonary artery (IUAPA) is a rare congenital anomaly characterized by varied and nonspecific clinical manifestations, such as dyspnea during exercise, recurrent pulmonary infections, hemoptysis, or it may remain asymptomatic (1). Consequently, it is frequently misdiagnosed or undetected. We report the case of a previously "healthy" 38-year-old male who presented with a recent onset of dyspnea. His chest radiograph revealed abnormalities that led to a suspicion of pulmonary embolism. However, subsequent investigations using advanced imaging modalities, including computed tomographic (CT) pulmonary angiography and contrast pulmonary angiography, confirmed a diagnosis of isolated unilateral absence of the right pulmonary artery.
2. Case Presentation
A 38-year-old male, previously healthy, began experiencing progressive dyspnea on exertion four months prior to admission. He denied any past medical history of hemoptysis or recurrent pulmonary infections. Approximately 10 years ago, he sustained blunt torso trauma with multiple right rib fractures during an accident. Upon admission, his blood pressure was 121/72 mm Hg, heart rate was 92 beats per minute, and SpO2 was 97% on room air. Chest auscultation revealed diminished breath sounds over the right lung. The remainder of the physical examination was unremarkable. Routine hematologic and biochemical profiles were within normal ranges, and the D-dimer level was normal.
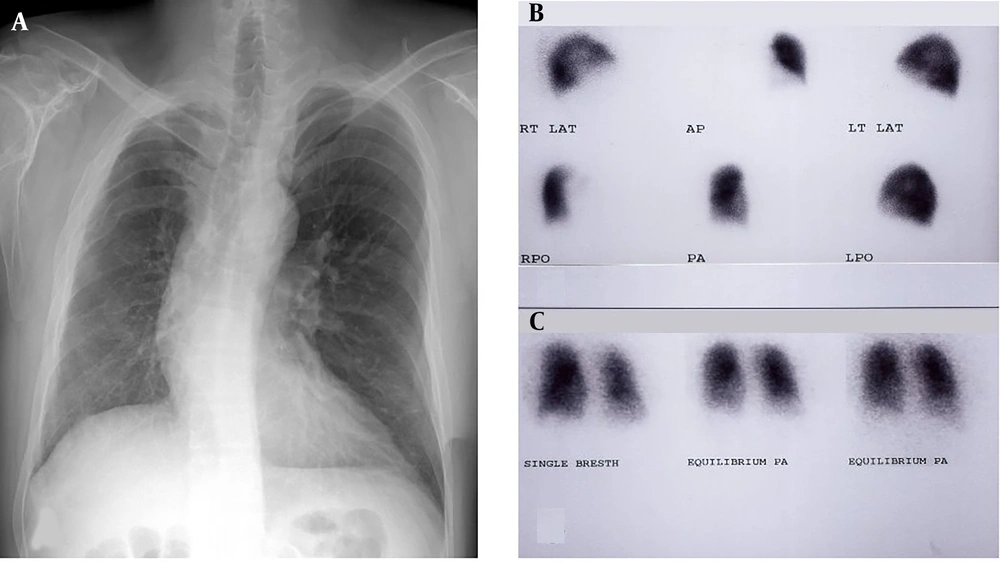
A chest X-ray (Figure 1) showed an absent right hilar shadow, reduced volume of the right lung, decreased pulmonary arterial vascular markings over the right lung, tracheal shift to the right, elevation of the right hemidiaphragm, and multiple right rib fractures. The electrocardiogram was normal. Cardiac echocardiography demonstrated preserved cardiac systolic function and no apparent structural abnormalities of the heart. The clinical presentation of unexplained dyspnea and chest X-ray findings led to a suspicion of pulmonary embolism.
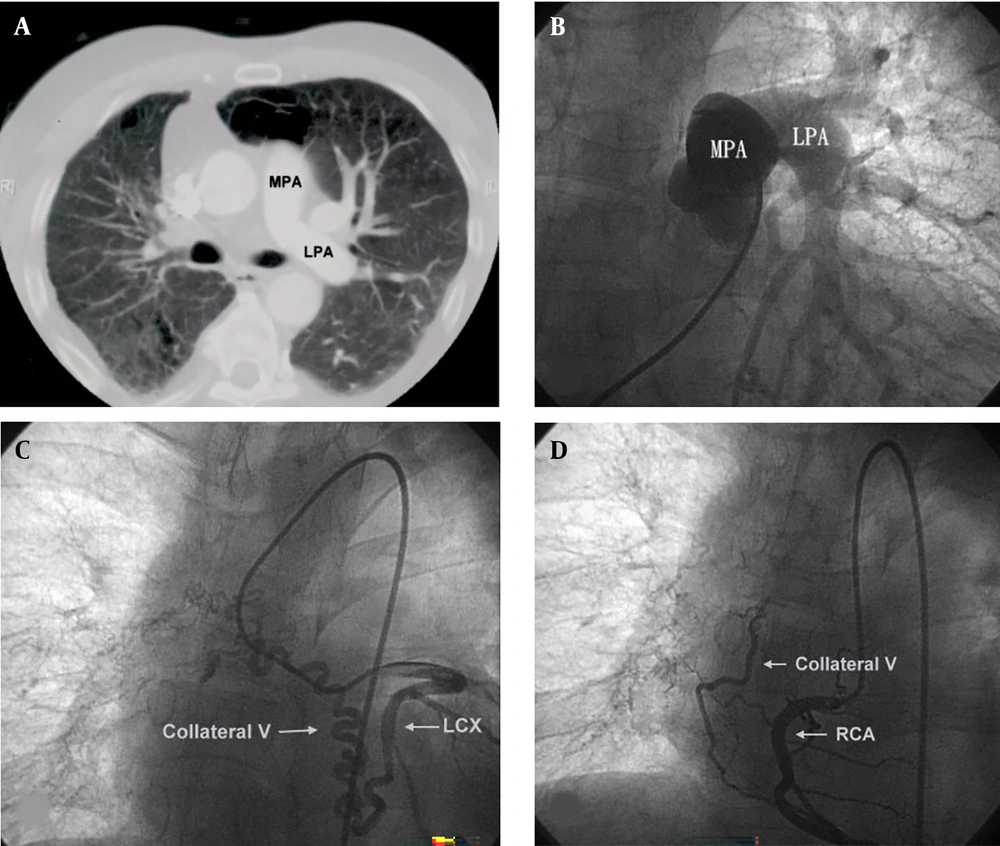
The ventilation/perfusion (V/Q) lung scans were performed. The lung perfusion scan identified absent perfusion of the right lung and normal perfusion of the left lung (Figure 1B). The bilateral pulmonary ventilation scan was normal (Figure 1C). A CT pulmonary angiography scan with contrast enhancement showed a normal left pulmonary artery and an absent right pulmonary artery (Figure 2A). Cardiac catheterization was performed on room air, revealing pulmonary artery pressure of 34/20/26 (systolic/diastolic/mean) mm Hg. Pulmonary angiography confirmed the absence of the right pulmonary artery and a normal left pulmonary artery (Figure 2B). A selective coronary angiographic study demonstrated anomalous vessels arising from the left circumflex artery (Figure 2C) and right coronary artery (Figure 2D) supplying the right lung.
A, Chest PA film showing absent right hilar shadow, reduced volume of right lung, diminished vascular markings over the right lung field, trachea deviate to the right, elevation of right hemidiaphragm and multiple right rib fractures; B, lung perfusion scan demonstrating absent perfusion of the right lung and normal perfusion of the left lung; C, lung ventilation scan demonstrating normal ventilation bilaterally.
A, A chest computed tomographic (CT) pulmonary angiography scan with contrast enhancement shows absent right pulmonary artery; B, pulmonary artery angiography shows absent right pulmonary artery; C, selective left coronary angiography demonstrates collateral vessels arising from the left circumflex artery supplying the right lung; D, selective right coronary angiography demonstrates collateral vessels arising from the right coronary artery supplying the right lung. Abbreviations: MPA, main pulmonary artery; LPA, left pulmonary artery; LCX, left circumflex artery; RCA, right coronary artery; collateral v, collateral vessel.
The patient reported improved dyspnea symptoms after bronchodilator therapy and was discharged on hospital day 12. At the latest follow-up, three years after discharge, the patient was well, except for a complaint of mild exercise intolerance.
3. Discussion
Unilateral absence of the pulmonary artery is a rare congenital anomaly first described by Fraentzel in 1864 (2). It is thought to result from altered development of the sixth aortic arch segment, which fails to connect with the pulmonary trunk during embryonic development (3). Systemic-to-pulmonary collateral arteries may develop to sustain the growth and development of the affected lung. These collateral arteries include the bronchial artery and other systemic collaterals such as intercostal, internal mammary, or subdiaphragmatic arteries, and rarely, the coronary artery (1, 4). Collateral vessels connecting the coronary artery and bronchial artery are identified in 4% of cases (4).
3.1. Epidemiology
Unilateral absence of the pulmonary artery is a rare congenital anomaly with an estimated prevalence of 1 in 200,000 individuals. It is often associated with other cardiovascular malformations such as Tetralogy of Fallot, septal defects, patent ductus arteriosus, transposition of the great vessels, and coarctation of the aorta (1). However, it may occasionally be an isolated finding, termed isolated UAPA, which constitutes approximately 40% of overall UAPA cases (1). Non-isolated UAPA may present in infancy with respiratory distress, pulmonary hypertension (PHT), and congestive heart failure (5), typically detected during the diagnostic congenital heart disease (CHD) workup in pediatric patients and can be surgically corrected (1).
3.2. Clinical Presentation
The clinical manifestations of isolated UAPA vary widely. In cases of IUAPA, 15 - 27% of patients remain asymptomatic until adulthood (1, 6). Most patients with IUAPA present with symptoms such as dyspnea on exertion, limited exercise tolerance (40%), recurrent pulmonary infections (37%), hemoptysis (20%), and chest pain (1). Associated PHT is found in 44% of patients (1). These manifestations are nonspecific and may occur in various combinations or singly, making diagnosis challenging for physicians.
3.3. Pathophysiology
Proposed mechanisms of dyspnea in IUAPA patients include reduced total lung capacity, increased resting and/or exercise physiological dead space, and PHT (7, 8). Recurrent pulmonary infections are thought to result from hypoperfusion, leading to reduced mucosal defense and increased risk of respiratory infections (8). Chronic pulmonary infections can lead to secondary bronchiectasis in some patients (9). Hemoptysis is caused by rupture of engorged collateral vessels, which may be self-limiting for many years but can also lead to massive pulmonary hemorrhage and death (8). Pulmonary hypertension is thought to result from increased blood flow to the unaffected pulmonary artery, increasing shear stress on the endothelial lining and causing endothelin (a vasoconstrictor compound) release. This leads to constriction of the pulmonary vasculature, increased pulmonary resistance, and hypertension (10). Severe PHT can cause right heart failure. The implications of associated coronary-to-pulmonary collaterals vary from no effect to myocardial ischemia (11) and infarction (12). In our patient, the effect of associated coronary-to-pulmonary collaterals on myocardial perfusion was not evaluated, as the patient had no chest pain and his ECG showed no signs of myocardial ischemia. However, these collaterals may cause ischemic cardiac symptoms, suggesting that coronary angiography should be an essential diagnostic modality when cardiac catheterization is performed.
3.4. Diagnosis
Various imaging modalities are useful in diagnosing IUAPA. A chest radiograph is usually the first examination test. Characteristic chest radiographic findings of IUAPA include asymmetrical lung fields, reduced volume of the hemithorax with reduced pulmonary vascularities, absent hilar shadow reflecting the absent hilar vasculature on the affected side, trachea and mediastinum shift toward the affected side, and elevation of the ipsilateral hemidiaphragm. Compensatory hyperinflation or a plethora of lung fields due to increased blood flow may be seen on the contralateral side (13). The electrocardiogram is usually normal in uncomplicated cases (without PHT), whereas it shows right ventricular hypertrophy in cases associated with PHT (7). Echocardiography aids in estimating pulmonary arterial systolic pressure by Doppler interrogation of the tricuspid valve regurgitation jet and can detect associated cardiovascular anomalies (7). The V/Q lung scans are useful for diagnosing IUAPA, typically demonstrating nonperfusion in one lung, normal perfusion in the unaffected lung, but normal ventilation in both lungs (14). However, these findings on V/Q lung scans may also be noted in acquired unilateral pulmonary thromboembolic occlusion (15, 16), thus it should be considered in the differential diagnosis. The CT pulmonary angiogram and MRI can depict the detailed anatomic condition of the pulmonary artery, enabling differentiation between these two conditions (7, 8). According to the aforementioned discussion, the clinical manifestation of unexplained dyspnea, chest X-ray findings, and V/Q lung scan findings in this patient closely resemble pulmonary embolism (1, 13, 15, 16). Noninvasive CT pulmonary angiography and MR imaging can diagnose IUAPA with certainty (7, 8). Additionally, chest CT can assess the presence of bronchiectasis (7). Right heart catheterization can provide hemodynamic data such as pulmonary arterial pressure and reversibility of PHT following oxygen or nitric oxide inhalation (17). Although pulmonary angiogram remains the gold standard for diagnosis, it is rarely performed due to the reliability of noninvasive imaging (such as CT pulmonary angiogram and MR imaging) and is reserved for patients who need selective embolization or revascularization procedures (7).
3.5. Treatment
The therapeutic strategy for patients with IUAPA is based on the patient’s symptoms. No treatment is needed in patients without evidence of cardiopulmonary dysfunction (8). Selective embolization of the systemic collateral circulation responsible for bleeding may be used to treat massive hemoptysis (8). In patients with massive or recurrent hemoptysis despite embolization of bleeding collaterals, pneumonectomy can be considered (8). In patients with recurrent intractable pulmonary infections, lobectomy or pneumonectomy can be considered (8). Early re-establishment of pulmonary blood flow may allow the affected lung to develop more normally and improve PHT (6, 18). Surgical revascularization through an aortopulmonary shunt or connection of the affected pulmonary artery to the main pulmonary artery is most successful in the pediatric population and not encouraged in older patients because the intrapulmonary arteries have been found to be severely narrowed or even completely obstructed by fibrosis (8, 18). In patients with severe PHT in whom revascularization cannot be performed, treatment with anti- PHT medications, including calcium channel blockers, prostacyclin analogues, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors, is recommended (1, 8).
3.6. Prognosis
The overall mortality rate of IUAPA is approximately 7% (1). Common causes of death include massive pulmonary hemorrhage, PHT, cardiac and respiratory failure, as well as high-altitude pulmonary edema (7). Since the risk of pulmonary hemorrhage and PHT significantly increases with age in patients with IUAPA (6), patients with absent or minor symptoms should be followed regularly, including serial echocardiography to monitor their pulmonary hemodynamics.
In conclusion, we have reported a case of isolated unilateral absence of the right pulmonary artery, which mimics pulmonary embolism in terms of clinical symptoms, chest roentgenograph, and V/Q lung scan perspectives. Clinicians must be familiar with the characteristic chest X-ray findings that may suggest IUAPA. Awareness of this rare entity and a high index of suspicion are critical for early diagnosis and management.