1. Context
Diabetes mellitus (DM) as a chronic disorder of glucose metabolism can cause a variety of complications (1). It is estimated that the global diabetes prevalence in 2019 was 9.3% (463 million people), projected to increase to 10.2% (578 million) and 10.9% (700 million) by 2030 and 2045, respectively (2). This complex illness needs continuous medical care beyond glycemic control, which is related to the multifactorial risk-reduction approaches. There are shreds of evidence suggesting that a variety of interventions in the form of a systematic approach is needed to improve diabetes outcomes (3). In this regard, both health care professional and patient education would be essential and considered as key strategies to diabetes management (4, 5).
Not only there is a shortage of competent health care professionals in providing high-quality diabetes care (4, 6, 7), but also the increasing complexity of DM management needs an up-to-date strategy for its prevention and management (8). Therefore, health care professionals are challenged to remain well informed of the latest clinical treatments and health care trends (8) and need constant and accessible evidence-based educational opportunities to provide evidence-based diabetes care (9). However, a variety of means are introduced to train and keep them up to date considered by researchers.
Patient education is an essential component of diabetes management (10). In this regard, evidence suggests that diabetes self-management education (DSME) would be an effective and cost-benefit strategy for improving glycemic and mental health outcomes via informing, training, and motivating people suffering from diabetes to manage their disease on their own (11). Diabetes self-management education varies in delivery method, content, technology use, and specific aims (11). However, the efficacy of DSME in both children and adolescents would be a challenge for the future (5).
Hence, regardless of education benefits for the patient (12-14) and health professional (4), it is imperative to analyze the recent research to identify research gaps and the following research priority in this area in our context. In Iran, there have been efforts to address these evidence gaps. For instance, the Iran Diabetes Research Roadmap (IDRR) study aimed to highlight gaps in diabetes education (15). Besides, other similar scoping reviews on diabetes in Iran have emphasized these evidence gaps (16).
2. Objectives
Our study aimed to have a scoping review of studies about patient and health professional education in the field of diabetes to identify research gaps in this area in Iran.
3. Data Sources
The current scoping review was conducted in the Diabetes Research Canter of Endocrinology and Metabolism Research Institute. This approach was selected to identify key concepts and gaps in the literature (17). The six-stage approach of Arksey and O'Malley (18) was used. It consisted of (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies; (4) charting the data; (5) collating, summarizing, and reporting the results; and (6) expert consultation.
3.1. Stage 1: Identifying the Research Question
The following research question was developed to inform the review: "What are the educational gaps and needs for patients with diabetes and health care providers who are involved in diabetes care teams in Iran?"
3.2. Stage 2: Identifying Relevant Studies
Two databases, including Scopus and PubMed were used to find relevant articles in the current study. The time interval for searching articles was from January 2015 to December 2019. The key terms used in the search strategy were Diabetes and Education. The diabetes group of terms were "diabetes"," diabetic", "T1DM", "T2DM", "T1D", "T2D", "MODY", "NIDDM", and "IDDM". The education terms were "curriculum", "education", and "teaching methods".
3.3. Stage 3: Study Selection
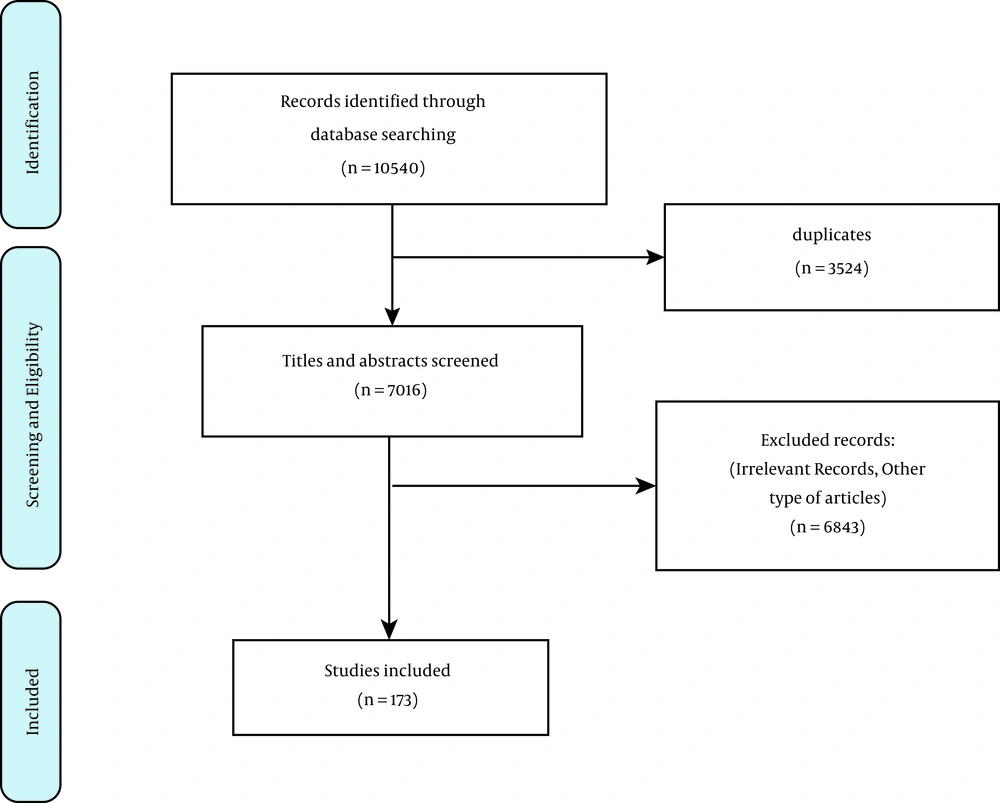
Two researchers (MA and MS) independently screened abstracts of the articles and assessed the eligibility for full-text retrieval. Selected full-text articles with disagreements were discussed between research team members to reach a consensus according to the inclusion criteria. The initial inclusion criteria were as follows: (1) original studies and reviews; (2) research studies conducted on Iranian populations; (3) studies published in 2015 – 2019; and (4) English and Persian languages. Since the current scoping review aimed to examine how education affects diabetes control in peer-reviewed research, we excluded books, book reviews, commentaries, letters to editors, Ph.D. theses, and reports. In this regard, after removal of duplicates, 7016 titles and abstracts were screened. Based on the criteria, 173 articles included in the study.
3.4. Stage 4: Charting the Data
Selected studies were categorized according to the study question, study design, participants, main findings, and outcomes. These criteria were extracted by two reviewers independently (MA and MS).
3.5. Stage 5: Collating, Summarizing, and Reporting Results
Of the 173 peer-reviewed articles, 151 articles were quantitative while 14 and eight articles were qualitative and review studies, respectively. Sixteen out of 70 articles collected data using questionnaires. Additionally, nine main categories were identified among 173 articles focusing on (1) educational program/approach/models; (2) health literacy; (3) mental health; (4) healthcare provider education; (5) self-management/care/efficacy; (6) virtual education; (7) educational establishment; (8) children; and (9) peer education. The following discussions will be made based on the findings of articles in each category.
3.6. Stage 6: Expert Consultation
To be confirmed, we presented our findings to several diabetes educators who were asked whether they recognized the findings, missed anything, and had any other comments on the findings.
4. Results
Based on the results of the search and review of the articles based on the study inclusion criteria, 173 articles (1.6% of all searched results) that considered diabetes education in Iran from 2015 to 2019 were reviewed. In Figure 1, the number of included and excluded articles is shown. Most of the articles (n = 46) were published in 2018, and the least ones (n = 25) in 2015. According to the subject classification, the included articles were categorized into 10 categories: Educational program/approach/models, health literacy, mental health, healthcare provider education, self-management/care/efficacy, virtual education, educational establishment, peer education, child education, and others. Most published studies (n = 151) were quantitative, whereas the least ones (n = 8) were review articles. Moreover, the categories of healthcare provider education (n = 2) and educational establishment (n = 2) had the least studies, and the category of self-management/care/efficacy (n = 64) had the most studies. Additionally, virtual education varied as SMS (11), game (1), websites (10), and mobile application (3). In this regard, the comparison of educational research on diabetes conducted in Iran is suggested in Table 1.
| Variables | N | Educational Program / Approach / Models | Health Literacy | Mental Health | Healthcare Provider Education | Self-management / Care / Efficacy | Virtual Education | Educational Establishment | Peer Education | Child Education | Others |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Publication range | 2016 - 2019 | 2016 - 2019 | 2017 - 2018 | 2015 - 2016 | 2015 - 2019 | 2016 - 2019 | 2018 - 2019 | 2016 - 2019 | 2018 | 2015 - 2019 | |
| Number of articles | 36 | 9 | 5 | 2 | 64 | 25 | 2 | 7 | 4 | 19 | |
| Study type | |||||||||||
| Quantitative | 151 | 34 | 8 | 5 | 2 | 57 | 19 | 0 | 6 | 1 | 19 |
| Qualitative | 14 | 0 | 0 | 0 | 0 | 5 | 4 | 2 | 0 | 3 | 0 |
| Mixed Methods | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Reviews | 8 | 2 | 1 | 0 | 0 | 2 | 2 | 0 | 1 | 0 | 0 |
| Study setting | |||||||||||
| Clinic | 133 | 27 | 4 | 3 | 0 | 49 | 23 | 2 | 6 | 2 | 17 |
| Hospital | 29 | 7 | 1 | 1 | 2 | 12 | 2 | 0 | 1 | 1 | 2 |
| Others | 11 | 2 | 4 | 1 | 0 | 3 | 0 | 0 | 0 | 1 | 0 |
| Study Design | |||||||||||
| Quantitative | |||||||||||
| Experimental | |||||||||||
| Randomized clinical trial | 57 | 13 | 1 | 2 | 0 | 22 | 9 | 0 | 5 | 0 | 4 |
| Quasi-experimental | 41 | 12 | 1 | 2 | 1 | 11 | 9 | 0 | 1 | 0 | 4 |
| Observation | |||||||||||
| Descriptive | 43 | 5 | 6 | 0 | 1 | 19 | 1 | 0 | 0 | 0 | 11 |
| Analytical | 12 | 4 | 0 | 1 | 0 | 5 | 0 | 0 | 0 | 1 | 1 |
| Qualitative | |||||||||||
| Phenomenological | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Content analysis | 7 | 0 | 0 | 0 | 0 | 4 | 2 | 0 | 0 | 1 | 0 |
| Grounded theory | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Action research | 4 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 |
Comparison of Educational Research on Diabetes Conducted in Iran (n = 173)
5. Discussion
Education is an important part of diabetes care that makes personalized care for each patient possible. This education has mainly been studied and known as diabetes self-management education (DSME), which improves treatment adhesion and increases patient's sensitivity to acute and chronic complications of DM and therefore leads to optimized management (19).
However, the field of education has become a wide topic for researchers, and other aspects of education need to be studied and established in Iran, as well. Educational programs, for instance, were the most studied topic in Iran, second to DSME. To achieve an efficient DSME, first, there should be educational programs for patients to ensure that they will be provided with necessary information on DM management, and yet this information will be practical. There have been national efforts in other countries to address specific needs for DM education programs, but there is no sufficient evidence in Iran yet (20). It has been highlighted that DSME is dependent not only on scientific educations on DM management but also on psychological and cultural components that play a role in patients' attitudes and behaviors toward DSME (21). Therefore, further studies should focus on these needs in educational programs for Iranian patients.
Virtual education also comprised a considerable number of included articles when compared to other topics, which is a strong point of Iranian researchers' efforts in the field of DM education since this topic is new and provides great opportunities for the improvement of technology and electronic health keeps going (22). Some DM apps have been used in some investigations, but the longitudinal and widespread use of these apps and virtual delivery of DM education in practice needs more engagement, and therefore, research in this field should not be neglected.
One important aspect of DM education is healthcare providers’ education, with limited studies focusing on this topic. Without a doubt, uneducated healthcare providers are not capable of personalizing DM patients' management with DSME (23). The Iran Diabetes Academy (IDA) has been responsible in this regard since 2017, and there are still many efforts that need to get done. According to healthcare delivery in Iran that is mostly dependent on primary practice in local areas, the IDA project has aimed to provide specific educational materials for these healthcare providers, and further research is mandatory to evaluate the benefits of this project and shed light on gaps and shortcomings for further improvement (24).
Child education is another important part of DM education. Successful primary prevention programs consider education in schools and among children and adolescents as a great opportunity for intervention to minimize the burden of DM by decreasing high-risk behaviors such as consuming unhealthy food and avoiding physical activity (25). The number of studies that have focused on this topic was also limited, which shows the importance of this issue, especially in Iran that has an increasing trend of DM.
Most of the included studies were quantitative studies, and both interventional and observational studies were included in similar numbers. Since randomized controlled trials are considered high-quality interventional studies, the acceptable number of RCTs among included studies indicates the good potentials of Iranian researchers in this field, and therefore, more investment of policymakers on DM education seems to be beneficial for both the prevention of DM and its optimized management.
The previous IDRR study on diabetes education concluded that the number of articles in this field is increasing and suggested that more interventional studies need to be performed (15); and in the current study, the majority of the included articles were interventional studies. The other suggestion in the previous review was to emphasize other topics rather than self-care education (15). The present study showed more variety in diabetes education topics, but the number of new topics is still not comparable with a topic like self-management. Therefore, more studies on these new topics should be done in the future.
Comparing to systematic reviews published recently, one interesting topic that should be investigated in future research is the reasons why diabetic patients do not attend educational programs (26). The role of family support in diabetes education is another new topic for Iranian researchers to address the needs in this regard in current educational interventions for DM (27). There is an evidence gap in the health economy features of DM education. Since systematic reviews suggest that despite the small number of studies, education is cost-effective (28), Iranian researchers can participate and even specify national needs; for instance, how should be the relationship between insurance policies and DM education costs in Iran.
It should be noted that education for diabetes management by a multidisciplinary team would be an important gap, which the included articles did not consider it. However, the effectiveness of multidisciplinary team-based education in children suffering from diabetes (29), newly diagnosed type 1 diabetes mellitus (30), and type 2 diabetes (31) are suggested. It seems that considering education with a multidisciplinary team-based approach based on the context and facilities of Iran is an undeniable necessity.
Only articles in English were included in this study, and therefore, those articles in Persian are missed. However, the search strategy was considered to gather as many articles as possible in English databases. Also, the systematic method of including articles in this scoping review is the other strength that could help with the exclusion of other articles that were not written in English.
5.1. Conclusions
This scoping review demonstrated that Iranian researchers have been active in the field of DM education during past years. However, some evidence gaps should be considered in future research. Utilizing electronic health for DM education, education of primary healthcare providers, and cost-effectiveness of educational interventions are among these gaps. Also, there should be more high-quality epidemiologic studies to provide an adequate understanding of factors affecting educational intervention outcomes, especially those related to the socioeconomic status of Iranians.
5.2. Practice Implications
Health care providers and patient education are important approaches to enhance glycemic control (4, 5). Accordingly, the evaluation of the effect of patient education on diabetes management has been done in most national research. However, the research related to multidisciplinary team members’ education for diabetes management is scarce. It seems that preparing a comprehensive research priority according to the national need assessment helps both policymakers and researchers to consider all aspects of diabetes education and its effect on DM management.