1. Context
Diabetes mellitus (DM) is a chronic, non-communicable condition that adversely affects several aspects of individuals’ lives, including their physical and mental health (1). Obesity, a sedentary lifestyle, and demands on the quality of life all worsen the problem (2). Diabetes requires long treatment; therefore, self-management is required (3). The first step to realizing self-empowerment in patients with type 2 DM (T2DM) is having a good understanding of self-management (4). So far, various methods have been used in research on self-management and self-empowerment of patients with T2DM. Unfortunately, optimal diabetes care is hindered by many factors, including the lifestyle choices of patients and lack of patient education (5). Establishing and implementing self-management require the right method and support (6).
Since 1980, the prevalence of diabetes has doubled worldwide; in adults aged 60 and older, it is now 8.5%, up from 4.7% (7). According to the International Diabetes Federation (IDF), in 2015, there were 415 million adults with diabetes aged 20 to 79, and this figure rose to 425 million in 2017 (1, 8). Only a third of DM patients can properly self-manage their disease; therefore, more than half of individuals with DM worry about their condition and its complicated management (9, 10).
Patients who want to control their DM need to commit to leading a healthier lifestyle and making consistent decisions (11). As a result, self-management becomes a way to achieve self-empowerment by enabling patients to manage their health and care for themselves (12). Increasing the patient’s sense of empowerment will enable them to think critically and make good decisions. Self-empowerment encourages patients to take responsibility for their own well-being.
Self-management has been improved through a variety of approaches: Using offline and online methods to intervene individually and in groups. In a previous review, it has been mentioned that several types of interventions have benefits for controlling the condition of T2DM patients, including improving glycaemic control with face-to-face delivery reporting educational and/or psychological interventions (13, 14), physical activity dietary programs (15-17), and religiosity or spirituality (18). However, other review studies have shown that the intervention is not effective because, at the end of the study, the intervention cannot provide significant improvement data regarding the condition of T2DM patients (19). In addition, another reason states that it is still an individual intervention; thus, it needs to be combined with other interventions (2).
To manage T2DM patients, individual interventions can be performed using the internet with myDIDeA (Malaysian Dietary Intervention for People with Type 2 Diabetes: An e-Approach), a 6-month web-based, individualized dietary intervention to help T2DM with uncontrolled hemoglobin A1c (HbA1c). Also, this website provides information about diet, attitude, and behavior (DKAB), stages of diet change (DSOC), fasting blood glucose (FBG), and HbA1c (20). The intervention with a support group is used to carry out the group intervention. Patients are given training through handbooks that are tailored to their specific cultures (21), a diary to record maintenance activities (22), a diabetes self-management record sheet (DSMRS) (23), a self-help worksheet (24), an educational booklet (11), an education module (25), and interactive teaching (26).
Despite numerous studies of diabetes management, there is no comprehensive study that has summarized these studies. Accordingly, this study aimed to review and summarize the potential method of self-management to improve self-empowerment.
2. Evidence Acquisition
This narrative review aimed to summarize the effective method of self-management to improve self-empowerment. Scopus, Science Direct, ProQuest, CINAHL, and SAGE databases were searched to retrieve studies published up to August 2020 on self-management in T2DM patients. All databases were searched using the combination of the following keywords: “self-management education” OR “diabetes self-management education” OR “patient education” OR “self-administration” OR “self-care” AND “type 2 diabetes mellitus” OR “diabetes mellitus type 2” AND "glycosylated hemoglobin A" OR "glycosylated hemoglobin A1c" OR "hemoglobin A glycosylated" AND "health-related quality of life" OR "life quality.” The author focused on the study design, population, type of intervention to deliver diabetes management, expected outcome for the patient, and time to deliver the intervention (Appendix 1 in Supplementary File).
The PICOS (population, intervention, comparator, outcome, and study design) framework was used in the article search strategy. The boundaries of the review question were clearly defined through the development of inclusion and exclusion criteria using the PICOS format (27-29). Inclusion criteria for this systematic review were (1) studies on T2DM patients in the scope of the hospital, clinic, or community, (2) studies that examined self-management interventions in T2DM patients with various delivery methods and durations of follow-up, (3) the comparator for the intervention group that was a standard care intervention delivered from a hospital, clinic, or community, (4) impact on increasing self-empowerment with indicators HbA1c and health-related quality of life, and (5) studies that were randomized controlled trials. Exclusion criteria were (1) T2DM patients whose follow-up periods were not explained in detail, (2) studies that discussed interventions but did not focus on improving self-management in T2DM patients, (3) studies that discussed other self-empowerment outcomes, such as cost efficiency and resource utilization for the care of T2DM patients, and (4) studies that were systematic reviews, editorials, meta-analyses, and review articles (narrative).
3. Results
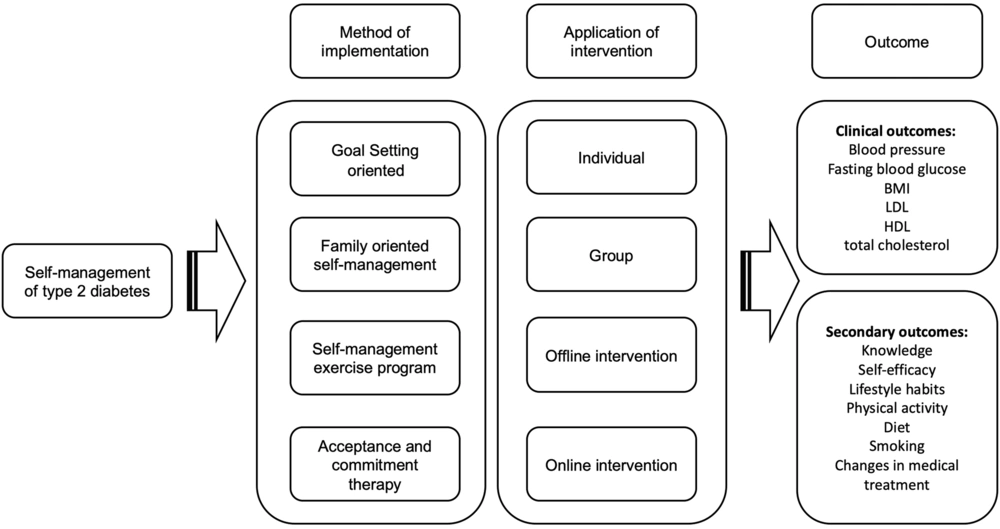
Of the 197 records retrieved by searching the databases, a total of 22 relevant studies were selected for this review. We first summarized the results of studies investigating the self-management method for T2DM. Next, we identified methods generally applied to people with T2DM, whether carried out individually, in groups, online, or offline. Based on the literature, primary and secondary outcomes have been used to determine the condition of patients with DM. Overall, the primary outcome included HbA1c and the quality of life of patients with T2DM. Other clinical outcomes reported to be expected in the patient were controlled blood pressure (22, 26, 30-35), controlled FBG (34, 36), body mass index (BMI) (26, 30, 31, 34, 35); low-density lipoprotein (LDL) (22, 36), high-density lipoprotein (HDL) (22), and total cholesterol (31). Some studies have also reported secondary outcomes, including patients’ knowledge (20, 21, 24, 30, 34, 37, 38), self-efficacy (21, 22, 24, 34, 36, 39-41), habits (20, 42, 43), physical activity (22, 24, 34, 40, 41), ability to follow the diet (20, 22, 34, 44, 45), smoking (21, 45), changes in medical treatment (31, 35, 42, 44, 46), self-management support (38, 44, 47-49), waist circumference (30-32), and healthy behavior (20, 21, 24, 31, 33, 38, 47, 48, 50).
Hailu et al. showed significant short-term improvements in related diabetes self-management education (DSME) parameters, including knowledge of diabetes and self-care practices. These findings are crucial for developing DSME programs in settings with constrained resources, both clinically and in terms of public health (21, 34, 38, 48, 51). Another study in Sri Lanka showed that teaching the patient to set goals in a diary had a clinically significant impact on glycemia, change in diet, physical activity, and self-efficacy of the participants in the intervention group (22). Patients with uncontrolled HbA1c (> 7.0%) can be managed using a diet planning called Web of MyDIDeA, containing a diet planning module. This study demonstrates that e-intervention can be a viable method for implementing chronic disease management in developing countries (20, 42). Besides using media, the engagement of family is also important for the diabetes patient to support the treatment. A study showed that the intervention group had significantly better independence, self-management, outcome expectations, and diabetes knowledge after the family was involved in the treatment program (24). The contribution of the community can lead patients to have better experience in diabetes treatment. Using peer-led structured patient education (which is carried out for 1 year) can improve blood sugar control with anthropometric parameters (HbA1c, BMI, and waist circumference) (30). The principle of peer-led is to focus on empowering each other (26, 52).
Any form of media can be used to give information about the management of diabetes patients. A study in Iran reported that educational booklets with the health belief model approach could significantly improve the metabolic condition and glycemic profiles than those in the control group. It also showed that knowledge, health beliefs, and quality of life were significantly improved in the intervention group (11, 35). Mobile phones also can maintain the condition of patients. It is commonly used by the health consultant to get better engagement with patients (32, 44, 47). This consultation may be combined with home visits to re-check the real condition of patients (31, 33, 41). Home visits may allow health practitioners to understand the real problem that makes a barrier for patients to continue the treatment. This consultation also allows patients to explore their feelings and conditions (37, 39).
Finally, 4 methods were discussed: Goal-setting-oriented, family-oriented self-management, self-management exercise program, and acceptance and commitment therapy (ACT) methods (Figure 1). These 4 methods represented other methods by considering the implementation method and the aspects of patient characteristics and conditions in every country. These 4 self-management methods of diabetes were delivered by a nurse or registered nurse certified to deliver and conduct the education. In this review, the results were presented as 4 sub-headings.
3.1. Goal-Setting-Oriented Method
Goal-setting is an important component of self-management, involving active collaboration between patients and nurses (22). The implementation of this method directs patients to increase compliance in carrying out physical activities, increase motivation to consume healthy foods, and reduce consumption of foods that can increase blood sugar. Goal-setting interventions must be accompanied by other supporting factors, including educational materials that must be able to facilitate discussion, not just the transfer of information between nurses and patients (21). Nurses must also understand the patient’s condition and spend enough time with the patient to set self-management goals (53). This is expected to motivate patients to carry out self-management.
3.2. Family-Oriented Self-management Method
Family support is one of the factors for patient compliance in carrying out self-management. Families who live in the same house with DM patients will affect the behavior of these patients (54). A good influence is shown by the enthusiasm and motivation given by the family to the patient; thus, the patient can be more confident in carrying out diabetes care. Families can play a role in reminding and helping supervise patients in maintaining health, such as early detection of diabetic ulcers and treatment of diabetic ulcer wounds (36).
3.3. Self-management Exercise Program
People with diabetes can benefit from a self-management exercise program that helps them improve their physical fitness. If done regularly, this activity can yield the best effects. Patients with diabetes should engage in physical activity since cardiovascular disease is a key risk factor that can increase morbidity. This is due to the fact that excessive blood sugar levels can harm nerves and blood vessels. Diabetes is often associated with high blood pressure, high cholesterol levels, and other lipid issues such as triglycerides. At the same time, these factors raise the risk of heart disease and stroke. Patients with diabetes can also control these risk factors by exercising regularly (41).
3.4. ACT
The goal of ACT is to compassionately assist patients in coping with any thoughts, feelings, worries, anxieties, or fears they may have regarding their diabetes and how to manage it so that they can live a happy and healthy life. Besides developing self-commitment and improving behavior, ACT tries to improve psychological problems by accepting the conditions that have been experienced. In patients with T2DM, the ACT intervention improved coping acceptance, self-management, and HbA1c levels (39).
4. Discussion
4.1. Goal-Setting-Oriented Method
Jayasuriya et al. showed that after a follow-up of 6 months, there was a significant improvement in HbA1c levels in the intervention group (22). DSME-Sri Lanka (DSM-SL) in the intervention group applies a goal-setting-oriented principle that involves patients and nurses making plans and targets in the care of T2DM patients. The results of this study are in line with Cheng et al., stating that the interaction of nurses and patients will form a supportive environment and help patients find their strengths in carrying out self-management and overcoming existing difficulties (55). Other studies have also shown that the interaction between nurses and patients is key to successful self-management (42). Setting goals is an important part of self-management that requires active engagement between patients and nurses. These interventions have demonstrated effectiveness by planning actions, demonstrating the physical activity, eating healthy foods, and avoiding potentially harmful foods. Prior to the intervention, the patient will be given a goal-oriented motivational interview and client-centered counseling to bring about behavior change by helping clients to explore and solve problems in self-management. Structurally, this intervention is suitable for people with diabetes in ethnic minority groups with an empowerment model involving a nurse and patient interaction (22).
4.2. Family-Oriented Self-management Method
Nurses offered a diabetic self-management educational program with a family orientation. It can boost self-efficacy and self-care practices, both of which are essential to avoid diabetes complications. It was created with self-efficacy theory and included family members in supportive care (24). Positive attitudes toward diabetes treatment and support from friends and family are connected with adequate diabetes care (56).
Family support can help T2DM patients gain confidence in their capacity to self-manage their condition. T2DM patients who live in a family setting and are cared for by family members will develop a sense of self-awareness and drive to practice self-care. Various things can be done to help family members with DM. One method is to raise self-awareness so that DM disease can be recognized. Patients with incurable DM should be aware of their prognosis to better control their disease (57). Living with ailing family members is another type of activity that can be done to help them. Providing support, time, and encouragement to continue learning and seeking further understanding about DM is also important.
4.3. Self-management Exercise Program
Diabetes is a chronic illness that lasts a lifetime. Acute, chronic, and significant problems occur as the disease advances, eroding patients’ faith in their ability to recover. Patients increasingly lose interest in self-management and therapy compliance, resulting in illness worsening. The usefulness of a diabetic education and self-management program on T2DM self-management, particularly in the short term, was supported by evidence. Diet and exercise guidance were at the heart of the first line of defense (34).
The data also show that the program is more successful than simply providing a pedometer in boosting daily steps in T2DM patients. The data also show that both programs result in increased self-reported physical activity and better glycemic control. As a result, in situations such as diabetic clinics in developing countries with limited resources for providing behavior modification programs, providing T2DM patients with pedometers may be sufficient to increase physical activity to levels that enhance glucose control (58).
4.4. ACT
Regarding diabetes self-management, ACT uses mindfulness meditation to improve a person’s ability to respond effectively to difficult thoughts and feelings in a variety of situations. This protocol includes exposure-based and experiential exercises, metaphorical language, and mindfulness training with deep breathing to help reduce stress and calm the mind (39).
Mindfulness training combined with deep breathing improves patients in refining consciousness by practicing a nonreactive, non-evaluative, moment-to-moment awareness from a deliberately non-judgmental stance. Patients are advised to examine their thoughts and emotions but not to judge them or become engrossed in them (59). This allows both happy and negative ideas and emotions to pass swiftly and help you become more aware of how your thoughts, feelings, and behaviors affect your emotional, mental, and physical health. This may also aid in better noticing, understanding, and integrating their own experience of self and environment, as well as reducing distractive or ruminative thoughts (59).
5. Conclusions
Diabetes self-management can be done with various methods. Each country has its own methods that are adapted to the conditions of society and the desired outcome. Of the various existing methods, there are 4 types of methods that can represent other methods, including goal-setting-oriented, family-oriented self-management, self-management exercise program, and ACT methods. These 4 methods can improve the health condition of T2DM patients with the main outcomes of controlling HbA1c levels and improving the quality of life of T2DM patients through other secondary outcomes. The government has a role in making policies so that this method can be implemented in health services, especially primary health services that are very close to the community, through existing health workers.