1. Background
Diabetes is the cardinal cause of death globally (1, 2). From a total of 3.7 million deaths linked to blood glucose level in 2012, diabetes was the direct cause of 1.5 million deaths worldwide and additional 2.2 million deaths were caused by increasing risk of cardiovascular and other diseases due to hyperglycemia (3, 4). It expected for diabetes to become the 7th leading cause of death by 2030 (4).
In the context of Bangladesh, there was a significant rise in the prevalence of diabetes among adults, in the past few years, indicated by a recent meta-analysis (5). Nowadays, 7.1 million adults are affected by diabetes, and this number is expected to increase to 13.6 million by 2040 (1). Prevalence is higher in urban (8.1%) populations than rural (2.3%) (6, 7). Moreover, Bangladesh is among the top ten countries with the highest number of adults with diabetes (8).
Progression of type 2 DM consequences certain acute and chronic complications in the majority of cases (9, 10). The present situation in Bangladesh will lead to consistent rise in the number of people with diabetic complications (11, 12). Due to the insidious nature of this disease, many people remain undiagnosed until complications appear (13). Lack of proper care at the early stage of development influences the patient’s quality of life, which also thrusts a considerable economic burden (14). The development of chronic complications is influenced by hyperglycemia (15). In almost all high-income countries, diabetes is a leading cause of cardiovascular disease, blindness, kidney failure, and lower limb amputation (8). The risk of dying among people with diabetes is twice than that of people without diabetes (16). Necessary interventions should be put in place, otherwise the cost of care for type 2 diabetes mellitus patients will have a negative impact on the health care system, as suggested by experts (17).
Many initiatives have already been taken to educate people with diabetes on how to minimize the complications, the impact is yet to be revealed. This primary particulars can be useful to execute future interventional strategies.
2. Objectives
This study was carried out with the aim of determining knowledge, attitude, and practices regarding complications of diabetes among patients with type 2 diabetes in Dhaka, Bangladesh.
3. Methods
The study was designed as a questionnaire based, cross-sectional analysis. Among all suitable patients, by employing convenient sampling, 425 patients with type 2 diabetes were recruited from the outpatient department of BIRDEM hospital in Dhaka, the capital of Bangladesh, in June 2016. This is the largest tertiary care hospital of the Diabetic Association of Bangladesh, providing facilities particularly for individuals with diabetes, regarding general health and emergency treatments for all illnesses and accidents. The sample included patients with type-2 diabetes older than 18 years attending for follow up or seeking general treatment in medicine outpatient departments except diabetes-related complications (such as diabetic foot, diabetic retinopathy, nephropathy, and neuropathy) with at least 1 year since the initial diagnosis of diabetes (1 year was to assure at least 1 training session on diabetes). Exclusion criteria included the presence of gestational diabetes mellitus, age of younger than 18 years, and being inpatients. Those unable to answer the questionnaire because of dementia, psychosis or profound deafness were excluded from the study.
3.1. Questionnaire Design
A pre-tested structured, bilingual questionnaire was developed to investigate key research questions comprised of both open- and close-ended questions. Each participant was interviewed face-to-face by a data collection team. The questionnaire was divided to 6 main categories, including demographic information, socioeconomic information, diabetes history and knowledge, attitude and practice-related information. Relevant questions were asked from the respondents, such as that of the knowledge module; emphasis was placed to assess the level of knowledge of respondents for complication of diabetes. To assess knowledge, attitude, and practices, 14, 12, and 9 questions were asked, respectively. Medical records were reviewed for recent hemoglobin A1C (HbA1C) levels (within 6 months of the inclusion), retrospectively. Ethical considerations were fulfilled by obtaining verbal consent and maintaining the confidentiality.
3.2. The KAP Score
To calculate knowledge, attitude and practices (KAP) score, a scoring system was prepared. Each correct answer was coded as 1, while each incorrect answer was coded as 0. In the practice section, components with better practice obtained a higher score up to 5, while respondents with poorer practice received lower scores. The final score for each category was then divided in quartiles. Four categories of knowledge, attitude and practice were outlined according to the score obtained by each respondent.
3.3. Statistical Analysis
The collected data was entered in the statistics package for social science (SPSS) version 22 for Windows. All continuous data were expressed as mean (± SD), and categorical variables were expressed as numbers and percentages. Descriptive statistics and frequency distributions were used to describe participant characteristics. The respondent’s socioeconomic status was calculated by using the principal component analysis (PCA) method according to the patient’s fixed assets and employment status. For variables with greater than two categories, one way analysis of variance ANOVA was used to compare means. After univariate and bivariate analysis, variables were entered in the software for multivariable analysis, considering all assumptions to meet the criteria. A forward selection method was applied using P values of 0.05 and 0.2 for including and excluding the variables from the final model, respectively. For analysis of attitude, the knowledge score was considered as an independent variable and for practice analysis both knowledge and attitude score were considered. Data was checked for the normal distribution of standardized residual plotting, observed cumulative probability, and expected cumulative probability.
4. Results
A total number of 425 patients with diabetes were enrolled in the study. Among them, 234 (55.1%) were males. Number of patients was higher the age group between 26 and 45 years (n = 231; 54.4%). The mean ± standard deviation (SD) of age of the study participants was 43.45 ± 11.81 years (range between 21 and 82 years). The majority of the participants (n = 190; 44.7%) were urban habitats.
The mean duration of diabetes was 9.16 ± 6.03 years. One hundred and seventy-four (40.9%) patients had a family history of diabetes. One hundred and sixty-four (38.6%) participants had attended educational programs on diabetes only once during the disease period. Nearly 60% of participants reported that a consultation time was provided between 5 to 10 minutes. One hundred and twelve (26.4%) patients reported that they were using herbal medication beside their regular prescriptions. Details are shown in Table 1.
| Characteristics | Valuesa |
|---|---|
| Age, y | 43.45 ± 11.81 |
| ≤ 25 | 17 (4) |
| 26 - 45 | 231 (54.4) |
| 46 - 65 | 156 (36.7) |
| > 65 | 21 (4.9) |
| Gender | |
| Male | 234 (55.1) |
| Female | 191 (44.9) |
| Marital status | |
| Married | 366 (86.1) |
| Unmarried | 59 (13.9) |
| Habitat | |
| Urban | 190 (44.7) |
| Semi-urban | 161 (37.9) |
| Rural | 74 (17.4) |
| Education | |
| Illiterate | 30 (7.1) |
| Primary to 8th grade | 93 (21.9) |
| Secondary | 71 (16.7) |
| Higher secondary | 122 (28.7) |
| Graduate and above | 109 (25.6) |
| Occupation | |
| Unemployed/laborer/retired | 43 (10.1) |
| Housewife | 125 (29.4) |
| Government services | 65 (15.3) |
| Private sector | 87 (20.5) |
| Business | 105 (24.7) |
| Socio-economic status | |
| Low income | 145 (34.1) |
| Average income | 140 (32.9) |
| Rich | 140 (32.9) |
| Duration of diabetes, y | 9.16 ± 6.03 |
| < 5 | 92 (21.6) |
| 5 - 10 | 204 (48.0) |
| >10 | 129 (30.4) |
| Family history of diabetes | |
| Yes | 174 (40.9) |
| No | 137 (32.2) |
| Unkonwn | 114 (26.8) |
| Educational programs | |
| Attended once | 164 (38.6) |
| Attended regularly | 104 (24.5) |
| Never attended | 157 (36.9) |
| Consultation Time, min | |
| < 5 | 70 (16.5) |
| 5 - 10 | 150 (58.8) |
| > 10 | 105 (24.7) |
| Methods of treatment | |
| Diet + Oral agents | 68 (16) |
| Diet + Insulin | 204 (48) |
| Diet + Oral agents + Insulin | 150 (35.3) |
| None | 3 (0.7) |
| Use of herbal medication | |
| Yes | 112 (26.4) |
| No | 313 (73.6) |
| Monitoring blood glucose | |
| Self monitoring | 16 (3.8) |
| Local pharmacy | 112 (26.4) |
| Hospital | 297 (69.9) |
aValues are expressed as mean ± SD or n. (%).
Only 3.8% (n = 16) of respondents reported that they monitored their blood glucose by themselves and nearly 70% (n = 297) at the hospital. The mean Random Blood Glucose was 11.06 ± 3.17 mmol/L (range 4.80 to 19.80 mmol/L), noted from the patients guidebook provided by the hospital for routine checkups. Mean HbA1c was 9.73 ± 2.65% (range 3.8% to 16.7%). Most of the participants mentioned that the source of their information regarding diabetes and its complications was doctors. The percentage was approximately 64% (n = 270) (Table 2).
| Sources | No. (%) |
|---|---|
| Physicians | 270 (63.5) |
| Friends/relatives | 13 (3.1) |
| Magazines/books | 45 (10.6) |
| Television/radio | 45 (10.6) |
| Newspaper | 42 (9.9) |
| Internet | 10 (2.4) |
4.1. Knowledge Score
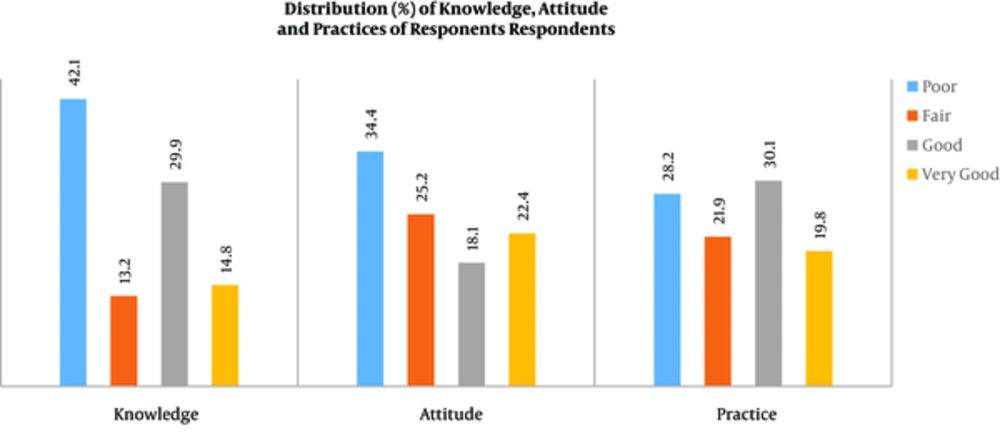
The maximum knowledge score was 14. The mean score was 9.2 (95% CI 8.9 - 9.4) and standard deviation (SD) was ± 2.11, with a range of 4 to 14. The study indicated that less than 50% of participants had poor knowledge regarding diabetic complications (n = 179; 42.1%). Nearly 15% of participants possessed very good knowledge (n = 63; 14.8%).
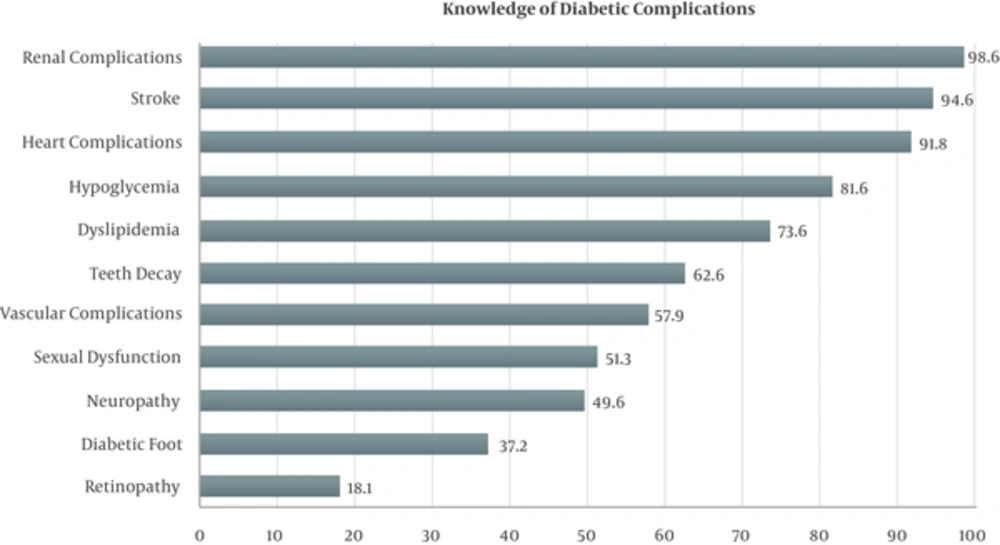
Approximately 81% (n = 343) of participants agreed that uncontrolled diabetes could cause certain complications. According to the correct answers given by the respondents, eye complication (retinopathy) was least known (n = 77; 18.1%). Most were known about renal and heart complications. Stroke due to uncontrolled diabetes was also known (n = 402; 94.6%). Regarding prevention of diabetic complications, 68% (n = 289) of respondents notified that they knew how to prevent these complications. Details are visualized in Figure 1.
The study indicated that patients with older age had better knowledge (P ≤ 0.001). Females had higher knowledge than males (P = 0.004). Patients living in urban and semi-urban areas (P = 0.022), educated above secondary level (P ≤ 0.001) and working in the government and private sector (P = 0.018) had better knowledge compared to their respective groups. Socioeconomic status of the respondents had an influence on patients knowledge (P = 0.003). Patients, who had diabetes for more than 10 years had better knowledge regarding its complications than patients, who had diabetes for less than 10 years (P = 0.008). Table 3 shows the details (Figure 2).
| Variables | Knowledge | Attitude | Practice | |||
|---|---|---|---|---|---|---|
| Mean ± SD | P Value | Mean ± SD | P Value | Mean ± SD | P Value | |
| Age, y | < 0.00 | < 0.001 | 0.368 | |||
| ≤ 25 | 7.47 ± 1.41 | 5.41 ± 1.50 | 15.88 ± 2.26 | |||
| 26 - 45 | 8.80 ± 1.97 | 7.19 ± 2.44 | 16.95 ± 3.82 | |||
| 46 - 65 | 9.86 ± 2.13 | 9.02 ± 2.82 | 16.91 ± 3.79 | |||
| > 65 | 9.85 ± 2.26 | 8.71 ± 2.75 | 16.85 ± 4.49 | |||
| Gender | 0.004 | < 0.001 | < 0.001 | |||
| Male | 8.92 ± 2.10 | 7.11 ± 2.40 | 17.48 ± 3.67 | |||
| Female | 9.58 ± 2.08 | 8.79 ± 2.88 | 16.16 ± 3.81 | |||
| Marital status | 0.094 | 0.003 | 0.001 | |||
| Married | 9.25 ± 2.12 | 8.02 ± 2.82 | 17.13 ± 3.88 | |||
| Unmarried | 8.76 ± 2.03 | 6.89 ± 2.89 | 15.38 ± 2.12 | |||
| Habitat | 0.022 | 0.155 | < 0.001 | |||
| Urban | 9.18 ± 2.17 | 8.01 ± 2.76 | 17.53 ± 3.71 | |||
| Semi-urban | 9.49 ± 2.12 | 7.95 ± 2.98 | 15.98 ± 3.07 | |||
| Rural | 8.54 ± 1.79 | 7.31 ± 2.13 | 17.21 ± 4.82 | |||
| Education | < 0.001 | < 0.001 | 0.001 | |||
| Illiterate | 7.93 ± 1.63 | 6.26 ± 1.33 | 17.56 ± 3.48 | |||
| Primary to 8th grade | 8.59 ± 1.66 | 7.04 ± 1.88 | 16.95 ± 4.44 | |||
| Secondary | 8.87 ± 1.82 | 8.23 ± 2.77 | 16.15 ± 3.80 | |||
| Higher secondary | 9.62 ± 2.12 | 8.39 ± 2.99 | 16.08 ± 3.08 | |||
| Graduate and above | 9.77 ± 2.38 | 8.19 ± 3.09 | 18.03 ± 3.45 | |||
| Occupation | 0.018 | < 0.001 | 0.087 | |||
| Unemployed/laborer/retired | 9.20 ± 2.25 | 7.76 ± 2.66 | 17.58 ± 3.61 | |||
| Housewife | 9.12 ± 1.94 | 8.29 ± 2.66 | 16.33 ± 4.06 | |||
| Government services | 9.15 ± 2.40 | 7.30 ± 2.86 | 17.15 ± 3.56 | |||
| Private sector | 9.81 ± 2.04 | 8.78 ± 3.03 | 16.44 ± 3.69 | |||
| Business | 8.77 ± 2.04 | 7.00 ± 2.28 | 17.47 ± 3.66 | |||
| Socio-economic status | 0.003 | 0.460 | 0.064 | |||
| Low income | 9.07 ± 1.93 | 7.95 ± 2.67 | 16.40 ± 3.88 | |||
| Average income | 8.82 ± 2.14 | 7.63 ± 2.70 | 16.84 ± 3.91 | |||
| Rich | 9.67 ± 2.19 | 8.02 ± 2.90 | 17.45 ± 3.91 | |||
| Duration of diabetes, y | 0.008 | < 0.001 | 0.089 | |||
| < 5 | 8.79 ± 1.80 | 7.15 ± 2.53 | 16.98 ± 3.87 | |||
| 5 - 10 | 9.08 ± 2.13 | 7.68 ± 2.78 | 16.50 ± 3.53 | |||
| >10 | 9.64 ± 2.23 | 8.72 ± 2.68 | 17.43 ± 4.07 | |||
| Family history of diabetes | 0.401 | 0.137 | < 0.001 | |||
| Yes | 9.25 ± 2.08 | 7.85 ± 2.61 | 17.54 ± 3.96 | |||
| No | 8.99 ± 2.13 | 8.19 ± 2.71 | 17.26 ± 3.62 | |||
| Unkown | 9.32 ± 2.13 | 7.50 ± 2.99 | 15.44 ± 3.34 | |||
| Educational programs Attended once | 10.23 ± 1.95 | < 0.001 | 9.56 ± 2.96 | < 0.001 | 15.73 ± 3.11 | < 0.001 |
| Attended regularly | 9.25 ± 2.25 | 7.22 ± 2.44 | 16.67 ± 3.36 | |||
| Never attended | 8.05 ± 1.53 | 6.53 ± 1.53 | 18.24 ± 4.25 | |||
| Consultation time, min | 9.40 ± 1.92 | < 0.001 | 8.52 ± 2.78 | < 0.001 | 15.74 ± 3.89 | 0.005 |
| < 5 | ||||||
| 5 - 10 minutes | 9.48 ± 2.12 | 8.28 ± 2.90 | 16.90 ± 3.83 | |||
| > 10 minutes | 8.34 ± 1.99 | 6.43 ± 1.73 | 17.62 ± 3.43 | |||
| Methods of treatment | 0.299 | 0.026 | 0.070 | |||
| Diet + Oral agents | 8.88 ± 1.92 | 8.08 ± 2.71 | 17.66 ± 4.26 | |||
| Diet + Insulin | 9.11 ± 2.05 | 7.58 ± 2.70 | 16.85 ± 3.71 | |||
| Diet + Oral agents + Insulin | 9.43 ± 2.07 | 8.08 ± 2.81 | 16.67 ± 3.63 | |||
| None | 9.00 ± 2.00 | 11.66 ± 0.57 | 12.66 ± 1.15 | |||
| Use of herbal medication | 0.001 | < 0.001 | 0.370 | |||
| Yes | 8.61 ± 1.86 | 6.78 ± 1.89 | 16.61 ± 4.02 | |||
| No | 9.39 ± 2.16 | 8.25 ± 2.91 | 16.99 ± 3.70 | |||
| Monitoring blood glucose | < 0.001 | < 0.001 | 0.999 | |||
| Self monitoring | 10.68 ± 2.30 | 7.75 ± 3.45 | 16.93 ± 3.58 | |||
| Local pharmacy | 8.52 ± 2.06 | 6.50 ± 2.16 | 16.89 ± 3.34 | |||
| Hospital | 9.36 ± 2.05 | 8.39 ± 2.15 | 16.88 ± 3.96 | |||
Abbreviation: SD, standard deviation.
aP ≤ 0.05 is significant.
4.2. Attitude Score
The maximum attitude score was 13. The mean score was 7.87 (95% CI for mean 7.6 - 8.1) and standard deviation (SD) was ± 2.76 with a range of 2 to 13. Nearly 35% (n = 146; 34.4%) of participants had a poor attitude regarding diabetic complications. About 23% (n = 95) of the participants possessed a very good attitude level.
The majority of the respondents reported that they could prevent diabetic complications (66%), and good glycemic control was one of the ways to prevent it (66.4%). Only 45% of respondents agreed that regular blood glucose monitoring is helpful for preventing DM complications. Furthermore, 80% of the participants thought that smoking could exacerbate vascular complications due to diabetes while about 70% agreed that exercising regularly was helpful in preventing complications. Most of the participants agreed that diabetic complications reduced life expectancy (69%).
Age and gender of the respondents had a significant influence on attitude. Older age group (P ≤ 0.001) and being a female (P ≤ 0.001) was associated with a positive attitude. Married patients had better attitude score than unmarried patients (P = 0.003). Patients with duration of diabetes more than 10 years had better attitude score than those who had duration of diabetes less than 10 years (P ≤ 0.001) (Table 3).
4.3. Practice Score
The maximum practice score was 27. The mean score was 16.89 (95% CI for mean 16.25 to 17.53) and standard deviation (SD) was ± 3.79 with a range of 3 to 27. The finding was that nearly 20% (n = 84; 19.8%) of the participants scored good in practice regarding diabetic complications. Almost 30% (n = 120; 28.2%) of the participants possessed poor practice.
More than 95% (n = 407; 95.8%) of the patients reported that they monitored their blood glucose on a regular basis and more than 85% of patients followed their prescription regularly, yet only about 60% (n = 243; 57.2%) performed exercise on a daily basis. Less than 50% of respondents reported about regular feet examination. Periodical kidney examination was done by approximately 64% (n = 271; 63.8%) of the respondents.
Practice score is also influenced by gender, habitat, marital status, and education. Unlike knowledge and attitude, mean score of practice was higher among males (P ≤ 0.001). Similarly, mean score of practice was higher among married patients (P = 0.001). Urban habitats had better practice score than semi-urban and rural habitats (P ≤ 0.001). Family history of diabetes had a significant influence on patients practice score (P ≤ 0.001) (Table 3).
4.4. Multivariable Analysis
Multiple linear regression analysis showed that the predictors that influenced knowledge score were age, gender, education, occupation, socioeconomic status, and educational program. Keeping all other variables on the baseline, if age was increased by 1 year, the knowledge score was also increased by 0.04 (P value < 0.001). Females had better knowledge than males by 0.55 (P value 0.04). Controlling all other predictors, respondents with higher degrees had better knowledge score than illiterates (P value 0.002). Respondents, who had attended the educational program had better knowledge than those who never attended by 1.49 (P value < 0.001).
Keeping all the variables on the baseline, one unit increase in knowledge score improved the attitude by 0.39 (P value < 0.001). Attitude score was improved by 0.07 with every year increase in age (P value < 0.001). Controlling all other predictors, females had a better attitude score by 1.24 than males (P value < 0.001). Attitude was better among those who attended the educational program than those who never attended by 1.99 (P value < 0.001). Poor attitude level was noticed among respondents taking multiple treatment methods.
Marital status was a significant predicator for practice. Controlling other predictors, married respondents had good practice score than unmarried respondents (P value 0.017). Duration of diabetes mellitus (DM) (Years) was another significant influencing factor for practice. One year increase in the duration of DM improved practice score by 0.07 (P value 0.021). While other predictors were controlled, patients with family history of DM had better practice by 2.05 (P value < 0.001). Respondents attended the educational program regularly and had a lower practice score. Higher educated respondents had better practice score by 1.44 than illiterates (P value 0.045). Details are shown in Table 4.
| Predictors | Knowledge | Attitude | Practice | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | Coef. | 95% CI | ||||
| Lower | Upper | Lower | Upper | Lower | Upper | ||||
| Age | 0.04a | 0.03 | 0.06 | 0.07a | 0.05 | 0.08 | - | - | - |
| Sex | |||||||||
| Male | Reference | Reference | - | ||||||
| Female | 0.55b | 0.21 | 1.12 | 1.24a | 0.83 | 1.65 | - | - | - |
| Education | |||||||||
| Illiterate | Reference | Reference | Reference | ||||||
| Primary to 8th grade | 0.62 | -0.16 | 1.39 | 0.29 | -0.50 | 1.10 | 0.09 | -1.31 | 1.49 |
| Secondary | 0.67 | -0.15 | 1.49 | 1.29b | 0.26 | 1.92 | -0.53 | -2.00 | 0.94 |
| Higher secondary | 1.22b | 0.44 | 1.99 | 1.08b | 0.28 | 1.89 | -0.04 | -1.44 | 1.35 |
| Graduate and above | 1.27b | 0.45 | 2.09 | 0.77 | -0.03 | 1.58 | 1.44b | 0.03 | 2.85 |
| Occupation | |||||||||
| Unemployed/retired | Reference | - | - | ||||||
| Housewife | -0.01 | -0.82 | 0.79 | - | - | - | - | - | - |
| Government service | 0.04 | -0.74 | 0.82 | - | - | - | - | - | - |
| Private sector | 0.59 | -0.18 | 1.37 | - | - | - | - | - | - |
| Business | 0.46 | -0.28 | 1.21 | - | - | - | - | - | - |
| Socio-economic status | Reference | - | - | ||||||
| Low income | |||||||||
| Average income | -0.15 | -0.60 | 0.29 | - | - | - | - | - | - |
| Rich | 0.51b | 0.03 | 0.98 | - | - | - | - | - | - |
| Educational programs | |||||||||
| Never attended | Reference | Reference | Reference | ||||||
| Attended once | 1.49a | 1.05 | 1.95 | 1.33a | 0.84 | 1.83 | 1.95a | -2.83 | -1.07 |
| Attended regularly | 1.05a | 0.59 | 1.50 | 0.19 | -0.32 | 0.72 | -1.57c | -2.54 | -0.69 |
| Consultation time, min | |||||||||
| < 5 | Reference | - | - | ||||||
| 5 - 10 | 0.01 | -0.49 | 0.50 | - | - | - | - | - | - |
| > 10 | -0.36 | -0.96 | 0.24 | - | - | - | - | - | - |
| Monitoring blood glucose | |||||||||
| Self monitoring | Reference | Reference | - | ||||||
| Local pharmacy | -1.55c | -2.48 | -0.61 | 0.33 | -0.69 | 1.36 | - | - | - |
| Hospital | -1.09b | -2.01 | -0.19 | 1.08b | 0.09 | 2.05 | - | - | - |
| Family history of diabetes | |||||||||
| Unknown | - | Reference | Reference | ||||||
| Yes | - | - | - | 0.97a | -1.48 | -0.46 | 2.05a | -2.92 | -1.18 |
| No | - | - | - | -0.58b | -1.03 | -0.14 | 0.22 | -0.55 | 1.00 |
| Methods of treatment | |||||||||
| None | - | Reference | - | ||||||
| Diet + Oral agents | - | - | - | -3.45c | -5.69 | -1.19 | - | - | - |
| Diet + Insulin | - | - | - | 3.89a | -6.11 | -1.69 | - | - | - |
| Diet + Oralagents + Insulin | - | - | - | 4.06a | -6.28 | -1.84 | - | - | - |
| Marital status | |||||||||
| Married | - | - | Reference | ||||||
| Unmarried | - | - | - | - | - | - | -1.21b | -2.19 | -0.21 |
| Duration of diabetes | - | - | - | - | - | - | 0.07b | 0.01 | 0.13 |
| Knowledge score | N/A | 0.39a | 0.29 | 0.50 | -0.17 | -0.36 | 0.02 | ||
| Attitude score | N/A | N/A | -0.19b | -0.34 | -0.04 | ||||
| Constant | 5.85 | 4.25 | 7.44 | 1.81 | -0.98 | 4.59 | 22.03 | 19.74 | 24.32 |
| Adjusted R2 | 0.324 | 0.52 | 0.23 | ||||||
Abbreviations: CI, confidence interval; Coef., coefficient.
a < 0.0001.
b < 0.05.
c < 0.001.
5. Discussion
Several studies have been carried out on knowledge, attitude, and practices (KAP) of diabetes (18-22) or knowledge of complications of type 2 diabetes (23, 24). Similar studies have been conducted in Bangladesh (25-28). Therefore, no study was found assessing the Knowledge, Attitude and Practices (KAP) of diabetes complications among patients with type 2 diabetes. However, it was difficult to compare the current results with others.
Very few participants had good knowldege about diabetic complications, which is similar to others (23, 24). The majority of the participants had a poor attitude level. The results showed that participants with better knowledge also had a better attitude score. In the practice section, only 30.1% were in good practice category. Those were a small number of patients, who were able to manage their health conditions to avoid further complications. These figures are supported by other similar studies (22).
In the current study, it is shown that nearly 81% of respondents knew diabetes could cause certain complicaitons if remained uncontrolled, while in another study it was only 51.1% and 59.6%, respectively (23, 24). Cardiovascular (91.8%), cerebrovascular (94.6%), and renal complications (98.6%) were known by most of the participants while eye complcations (18.1%) were least known in this study. Similarity was found with other studies (28, 29). However, inadequate knowledge regarding complications of diabetes tend to decrease awareness and may lead to high economic burden in terms of management of complications.
The present study revealed that 66% of respondents agreed that they could prevent diabetic complications while in other studies the figure was 62.3 in Pakistan and 52.7 in Ethiopia (18, 22). In this study, almost 80% respondents had agreed that smoking can exacerbate diabetic foot complication, while another study reported that nearly half of the respondents were unware about smoking and its relationship with diabetic foot complications (24).
It is generally believed that males are more knowlegeable for healthy lifestyles than females. A study in Pakistan showed better knowledge level in males regarding diabetic complcaitions than females (30), yet the study of Haque et al. (2009) showed no significant difference in different genders (26). In the current study, keeping other predictors controlled, gender was a significant predictor of knowledge and attitude, where females scored better.
The present study found similarity with the study of Niroomand et al. (2015), in that age was associated with patient’s knowledge, attitude, and practices regarding diabetes (31). In the current study, knowledge and attitude was improved with age. Hence, this may suggest that younger patients need greater motivation from their physician and family.
Good knowledge was significant among participants, who had higher socioeconomic status. This finding was consistent with other studies in India and Ethiopia (20, 32). This could be explained by the fact that participants with higher socioeconomic status have better access to education and alternative private checkups without waiting for conservative treatment facilities in the health system. In the current study, controlling other variables, educational status had a significant association with good knowledge, attitude, and practices. Other studies also led to the same findings (20, 22, 33). This might be because educated participants are able to read necessary information easily compared to the illiterates.
In this study, the main source of information was health porofessinals (63.5%), particuarly physicians. This statement was supported by a study in Ethiopia (20). This emphasizes on media contribution, which was very low in this study (10.6%) compared to other studies in Gujarat, India (32). Consultation time given by doctors was less than five minutes, reported by nearly 17% of participants in the current study, which was better than India (43%) and Ethiopia (58%) (20, 32). Lack of information related to the disease persists. The explanation might be physician’s focus on acute management rather than preventive care or heavy load of patients. Existing clinical evidence suggests that increasing community awareness regarding diabetes management is an ultimate tool for halting complications due to diabetes (34).
A recent study in Iran found a positive significant correlation between disease duration and complication with knowledge, attitude, and practice level (31). In the current study, duration of diabetes was a significant predictor of practice. This may be due to regular counseling and contact with health professionals. Another study in Iran, reported having had no effect of duration of diabetes with knowledge and practice regarding diabetes foot care, which may indicate the usefulness of patient education in healthcare facilities (24).
Attending an educational program was significantly associated with knowledge, attitude, and practices in the present study. Respondents, who attended educational programs performed better than those who never attended. It is important to know that providing education to vulnerable groups could become a cost-effective public health strategy (33) and properly designed educational programs could provide precise knowlege of diabetes even for less educated people (35).
Having positive family history of diabetes had a positive influence on patient’s attitude and practice, though it was not associated with knowledge, which is in contrast with the findings of other studies (36). Receiving information from the family with chronic disease might influence the patient’s attitude and daily practice, which can be a good source of information (31), yet, such informal sources are not always reliable.
This study could help in planning larger studies addressing the challenges in this project. As the current study was based on outpatients in one hospital, the results may not be typical of all diabetic patients in Bangladesh. The use of questionnaires for measuring knowledge, attitude, and practice areas could be another limitation because it is hard to avoid while assessing areas related to subjective fields of health, knowledge, choice, gratification, and identical areas bring risk of bias such that related with social desirability effect (37).
Evidence suggests that training and self-management is a core part of the treatment of diabetes (38). Patient education is the most constructive track that could assist with early detection, lessen the complications, and assist with the management of diabetes (39). This study re-emphasized the fact that properly designed and implemented education and other support programs would be more fruitful for patients with diabetes. Provided complete information on patient’s characteristics, healthcare professionals could effectively design their care processes, according to the patients’ needs (40). Self-care is an effective way to reduce complications of diabetes (41).
5.1. Conclusions
Lack of knowledge, poor attitude, and poor practice level were found in this surveyed communinty, particularly in males, illieterates and low income groups. Younger age group and rural habitats need greater attention in educational campaigns and physicians counselling. Physicians active participation and time for providing structured education and counseling for patients may bring better therapeutic outcome and lessen complications. Self management of patients should be encouraged. Source of information collected in this study will help identify popular medium that should be strengthened for future awareness and provide an educational base for patients. The sources will also be helpful in dissemination of knowledge on the preventive aspects of diabetic complications.