1. Background
Ultrasound-guided fine needle aspiration (FNA) of the thyroid gland is a well-established diagnostic technique that enables the assessment of the cellular morphologic features of the thyroid, which therefore helps in the planning of therapeutic management for thyroid nodules (1).
Since 2009, “The bethesda system for reporting thyroid cytopathology” has been used to standardize the interpretation of FNA cytology (2, 3). Each of the proposed 6 cytological diagnostic categories has an increasing risk of malignancy, and treatment approaches are suggested for each one.
The treatment proposed for Bethesda categories II, V, and VI is well established and not subject to much discussion considering their malignancy rates (4). However, categories III and IV are subject to debate on the best treatment options since their malignancy rates are 5% - 15% and 15% - 30%, respectively (2), which allows for different approaches.
Bethesda category III includes the cytological findings: “atypia of undetermined significance” (AUS) and “follicular lesion of undetermined significance” (FLUS), while Bethesda category IV represents “follicular neoplasm/suspicious for follicular neoplasm”. The recommendations for both situations are controversial and include repeating FNA after 6 months, thyroidectomy or clinical follow-up (1-5). The difficulty in determining the actual risk of malignancy lies in the fact that a minority of cases undergo a thyroidectomy, and therefore, there is no histopathological analysis of the lesion (2, 6-8).
In these cases, definitive diagnosis can only be achieved through histopathological analyses. The presence of some architectural aspects such as capsular and/or vascular invasion is crucial to establish a cancer diagnosis, which poses as a significant limitation to the FNA method.
Due to the persistent controversies in management of thyroid nodules in Bethesda III and IV categories and the variability of malignancy rates reported in the literature, this subject remains extremely relevant. Detailed reports from different populations can help physicians on the decision between an observational or surgical approach.
This report is based on Bethesda category III and IV cases operated at a tertiary referral cancer center in a department of head and neck surgery, as well as their association with malignancy and other possible diagnoses. In this department, surgical intervention is carried out for all Bethesda category III and IV patients (unless there are excessively high clinical risks).
The aim of this study is to attribute an accurate malignancy rate to these 2 cytological categories in patients from this community so that a real parallel can be established between cytological and histopathological findings. Incidentally detected carcinomas in other nodules than those that were the target of the FNA were also considered separately in this study.
2. Methods
This cross-sectional study was approved by the institutional ethics committee, number 228/14.
From January 2010 to January 2014, 582 patients diagnosed with Bethesda category III and/or IV thyroid nodules, were referred to the head and neck surgery department at instituto do Cancer do estado de Sao Paulo (ICESP). A total of 33 patients had 2 nodules aspirated, yielding cytological features compatible with Bethesda categories III or IV. Bethesda category III had 22 cases in both nodules, 1 case was Bethesda category III in 1 nodule and IV in the other, and 10 cases were Bethesda category IV in both nodules. Patients presenting with other thyroid nodules with cytological analysis suggestive of malignancy were not included in this cohort. All patients had thyroid ultrasound recorded in our database. In all, 615 thyroid nodules classified as Bethesda category III or IV were submitted for histopathological examination. Not all patients (31 patients/32 nodules) had their fine needle aspirations conducted at this hospital. These external materials were reviewed by cytopathologists from our institution’s staff and were included in the study only after a diagnosis of Bethesda category III or IV nodules had been confirmed in the review.
The cytopathological reports were issued according to institutional protocol following the bethesda classification categories and done by a pathologist from the staff. All reports are signed by 2 pathologists in agreement.
All patients underwent surgical treatment with removal of the node classified as Bethesda category III or IV (total or partial thyroidectomy).
The term incidental carcinoma was used for the cases in which a malignant neoplasm was diagnosed after surgery, however, it was not identified in the nodule previously submitted to FNA.
Electronic medical records of each patient were reviewed to establish an association between the FNA cytology results and final histopathological diagnosis. The exact position of the nodule in the gland and its dimensions were considered to correctly determine if the cytology and histopathology results were for the same nodule. Also considered were the following: patient’s age at operation, patient’s sex, location and maximum diameter of the nodule on ultrasonography, maximum diameter and final histopathological analysis of the target nodule, other pathologic findings, final surgical treatment, TNM stage, as well as multifocality if carcinoma.
At the time of this study, the reclassification of the encapsulated follicular variant of papillary thyroid carcinoma had not yet been published, and therefore was not considered (9).
The values obtained from the study for each of the continuous variables were described using means, ranges, and medians. Relative and absolute frequencies were used for categorical variables. Data were gathered and analyzed using the Microsoft Excel® software (Microsoft Corporation®, Redmond, WA, USA).
3. Results
A total of 582 patients presenting with Bethesda category III or IV thyroid FNA results were analyzed in this study with a total of 615 nodules. The majority of patients were female (89.6%) and 10.4% were male. The mean age at diagnosis was 54 years and varied from 15 to 86 years.
In 10 patients, partial thyroidectomy was initially performed, however, thyroidectomy was completed with a second operation due to the histopathological diagnosis of carcinoma, according to institutional protocol. A total of 64 patients underwent a partial thyroidectomy (with a normal unaffected lobe) and 518 underwent a total thyroidectomy.
In the female group, 406 patients (77.8%) had nodules diagnosed as Bethesda category III, 115 (22%) as Bethesda category IV, and 1 patient had 2 nodules, 1 in each category.
In the male group, 49 patients (81.7%) had Bethesda category III nodules and 11 (18.3%) had Bethesda category IV nodules.
Malignancy was diagnosed in 160 women (30.7%) and 25 men (41.7%). The average age for the malignancy group was 49.7 years (median 54, range 22 - 85). Among the patients whose final diagnosis was a benign thyroid nodule, the average age was 55.6 years old (median 60, range 15 - 86).
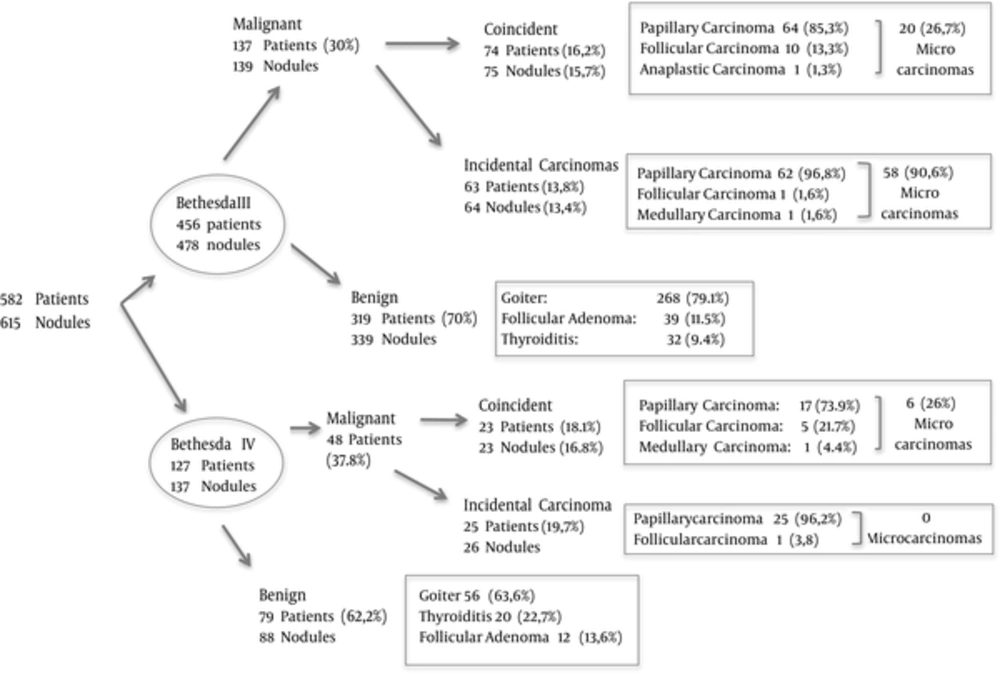
The detailed data describing the FNA and histopathological results is shown in Figure 1.
A total of 88 (15.1%) patients had incidental carcinomas (63 were in the bethesda category III group and 25 were in the Bethesda category IV group). They represented 47.6% of the 185 patients with a malignant diagnosis. The average diameter of these tumors was 0.5 cm (median 0.3 cm, range 0.1 to 2.9 cm) and multifocality was observed in 31 patients (35.2%). Ten patients (11.4%) had tumors with extrathyroidal extension (pT3), and 2 were diagnosed with node metastasis. Eighty-five patients (96.6%) had papillary carcinomas (follicular variant in 42, classic in 40, oncocytic in 2, and solid in 1), 2 had follicular carcinomas, and 1 had a medullary carcinoma. Of these tumors, 93% were microcarcinomas, which is a lesion smaller than or equal to 1 cm in size. Among these tumors, 8 had extrathyroidal extensions (9.8%) and 2 had cervical node metastasis.
Overall, 46 individuals (52.3%) had a malignant neoplasm diagnosed in the thyroid lobe contralateral to the lobe containing the nodule that was aspirated and 40 patients (45.5%) had carcinomas exclusively in the contralateral lobe. The average diameter was 0.6 cm (median 0.3 cm, range 0.1 to 2.9 cm). Only 3 cases were not microcarcinomas and were measured as 2.9 cm, 2.0 cm, and 1.4 cm.
4. Discussion
The current study consisted of a large single-institutional cohort of patients presenting with thyroid nodules classified as Bethesda category III or IV, with all patients undergoing a thyroidectomy. We had a real stratification of the risk of malignancy among those individuals, unlike other studies, in which, patients who underwent surgery had specific pre-screenings with inherent selection bias. We identified a 16% rate of malignancy in nodules classified as Bethesda category III, and 17% among those classified as bethesda category IV. When incidental carcinomas were included, these rates nearly doubled. The whole cohort was classified at the time of care under The bethesda system rather than retrospectively reviewed and assigned a category. For both bethesda categories III and IV, papillary carcinoma represented a majority of the malignant neoplasms, with approximately 50% of these being the follicular variant.
The probability of malignancy for each Bethesda category varies widely in the literature, especially for categories III and IV, which have the largest variability (1, 6, 8, 10-12). There is also a notable difference in the percentage of patients who had a histopathological follow-up (4, 6, 8, 10-17), mainly those with Bethesda category III nodules, with a range of 30% to 90% according to the reviewed data. This is the most controversial cytological category since its use is not uniform across institutions and there is some degree of subjectivity in the distinction between categories III and IV (10, 11).
Our study demonstrated that the rates of malignancy were almost the same in the patients with thyroid nodules classified as bethesda category III (16.2%) and bethesda category IV (18.1%). When considering the number of nodules, rather than the number of patients, these numbers decreased to 15.7% and 16.8%, respectively. For bethesda category III nodules, we found a malignancy rate higher than the upper limit described by The Bethesda System (an approximation of 5% - 15%) (2). For Bethesda category IV nodules, the malignancy rate was close to the lower limit anticipated by the system (15% - 30%). However, these numbers are lower than those described in other studies, with specific exceptions, as presented in Table 1. These findings can be explained by the fact that the whole cohort underwent surgery, rather than just selected patients with the most suspicious nodules based on radiological data. In addition, for Bethesda category IV nodules, where surgical resection is suggested, the rates of histopathological follow-ups were as low as 59% in the reviewed articles (4, 13, 15). We can also consider the possibility of heterogeneous and subjective interpretation of these categories between different observers in different institutions (8). Epidemiological and geographical discrepancies must also be considered.
| Reference | Bethesda III | Bethesda IV | ||||
|---|---|---|---|---|---|---|
| Histopathological Follow-Up (N) | % of the Cohort | % Malignancy | Histopathological Follow-Up (N) | % of the Cohort | % Malignancy | |
| Theoharis et al. 2009 | 27 | 30.3 | 48.1 | 102 | 61.4 | 34.3 |
| Jo et al. 2010 | 53 | 50.0 | 17.0 | 177 | 59.4 | 25.4 |
| VanderLaan et al. 2011 | 199 | 38.9 | 43.0 | a | a | a |
| Bongiovanni et al. 2012 | 132 | 53.2 | 14.4 | 698 | 78.8 | 32.1 |
| Mathur et al. 2014 | 255 | 31.6 | 39.0 | a | a | a |
| Ho et al. 2014 | 369 | 68.2 | 37.9 | a | a | a |
| Deniwar et al. 2015 | 65 | 69.0 | 34.0 | 42 | 97.7 | 50.0 |
| Rosario 2014 | 150 | 90.0 | 22.6 | a | a | a |
| De Napoli et al. 2016 | a | a | a | 258 | b | 34.9 |
| Present study | 478 | 100.0 | 15.7 | 137 | 100.0 | 16.8 |
Abbreviation: N, number of thyroid nodules evaluated.
aNot included in the study.
bData not shown.
In a meta-analysis, 25445 thyroid FNAs were reported with a histopathological follow-up in 6362 cases (25%). In the Bethesda category III group, 39% of patients underwent surgical resection, with a 15.9% malignancy rate. In the Bethesda category IV group, 70% of the patients underwent surgery. Among them, 26.1% of the target nodules were neoplastic. The variability in diagnosis was attributed to differences in population characteristics, nodule selection, and classification bias (2).
VanderLaan et al. reported 512 (10.9% of the cohort) cases as AUS. A repeat FNA was performed in 287 (56.1%) of the nodules after the initial AUS diagnosis, and 199 patients (38.9%) underwent thyroidectomy, with or without repeat FNA. Of the nodules, 43% were malignant. Patients with a histopathological follow-up after AUS diagnosis had a similar rate of malignancy (41%), as did patients who had a later AUS diagnosis (43%). Seven patients with benign cytological diagnosis after an initial bethesda category III classification underwent thyroidectomy and 29% had a final malignant diagnosis. In patients with a histopathological follow-up, there was no statistically significant difference in the rates of malignancy in those with benign aspirate after initial AUS classification compared to those with no repeat aspiration or a repeat bethesda category III diagnosis, indicating that surgery, rather than repeat FNA, may be a more appropriate diagnostic approach for these patients. It is also unclear why a repeat FNA resulting in a benign diagnosis should be more or less reliable than the first AUS/FLUS diagnosis (6).
Additionally, in a cohort of 4827 cytological specimens, 806 were classified as AUS after review in a different study (10). Among them, 255 patients underwent a thyroidectomy with 39% malignancies. The authors observed that AUS sub-classifications such as the “presence of focal nuclear atypia”, “focal microfollicular proliferation”, “focal Hurthle cell proliferation”, and “others” were associated with malignancy in 54%, 39%, 19%, and 26%, respectively, which are higher risks of malignancy than originally predicted based on The bethesda system. The authors recommended surgical resection for this cytological condition.
In another review of 3080 thyroid FNAs, the malignancy rate in the Bethesda category III group was 17% and 25.4% in the bethesda category IV group (15). Although, only approximately 50% of the cohort underwent surgery, this is the study with malignancy rates closest to our results.
In the present study, 137 patients with nodules classified as bethesda category III (30%) had carcinomas, including incidental carcinomas, and 39 (8.6%) had follicular adenomas, accounting for at least 176 (38.6%) patients who benefited from surgical treatment. In the bethesda category IV group, 60 (47.2%) patients were in this situation, including the incidental findings. Although most of the cases were microcarcinomas, their oncological evolution is not predictable and a balance between the risk of a potentially delayed diagnosis and an unnecessary operation should be taken into consideration (7). When incidental carcinomas were included, malignancy rates were similar in the 2 groups of patients (30% and 37.8%, respectively). Among incidental findings (15.1% of the total sample and 47.6% of patients with a malignant diagnosis) we observed that in 52.3% of the cases the carcinoma was identified in the lobe contralateral to the lobe that was aspirated. In addition, in 45.5%, the malignant neoplasia was found exclusively in the contralateral lobe. Only 3 of these lesions were not microcarcinomas. Thus, if total thyroidectomy had not been indicated for these patients, the chances of leaving a carcinomatous lesion were significant. The rate of papillary carcinoma was 96%.
The majority of reports relating cytological to histopathological diagnoses did not consider incidental carcinomas and the data are very heterogeneous regarding these results. Theoharis et al. calculated a 3.6% incidence of incidental carcinomas in an equivalent Bethesda category III and 5.5% in an equivalent Bethesda category IV among 2468 patients who underwent thyroid FNA (30.3% underwent surgical treatment in the first group, and 61.4% in the second group). However, if incidental carcinomas had been included in the study by Ho et al., the cumulative rate of malignancy would have been 57.2% among Bethesda category III nodules. In a cohort of 256 patients who underwent a thyroidectomy due to a benign disease (18), 11% were diagnosed with incidental carcinomas, similar to our results; 40% had multifocal lesions, and 57.5% were considered microcarcinomas. In another group of 586 patients who underwent thyroidectomies for reasons other than suspicion of cancer, 9.7% were incidental carcinomas, of which 96.5% were microcarcinomas (19). Among micropapillary carcinomas (incidental or not), a 33.7% rate of multifocality and a 7.4% rate of extrathyroidal extension were observed, similar to our findings. However, lymph node involvement was found in 15.8% (5.5% in incidental carcinomas), while it was observed in 4.6% (5 patients among 108) of our cases of microcarcinomas. The rates of incidental carcinomas and microcarcinomas in the thyroid gland vary across institutions. In addition, papillary microcarcinomas have been described in as many as 35% of autopsy studies, with 47% multifocality (20). Beyond geographical differences, when considering the large difference in reported prevalence, one must consider the attention to detail required by pathologists identifying microcarcinomas, whose diagnosis depends on millimetric histological sections. The rates of lymph node involvement also depend on appropriate sampling during the surgical procedure, which is not typically done in cases of presumed benign nature.
4.1. Conclusion
This paper provides a more precise correlation of malignancy rates with thyroid nodules classified as Bethesda categories III and IV, especially due to the fact that all patients in the cohort underwent surgical intervention. We observed a 16% rate of malignancy in nodules classified as bethesda category III as well as a 17% rate among those classified as bethesda category IV and found incidental carcinomas in 15% of patients.