1. Introduction
The clinical manifestations of pericardial effusion span a wide range, from an incidental observation during imaging to a potentially lethal emergency scenario like pericardial tamponade.
They can be grouped into inflammatory (due to viruses, bacteria, and mycobacterial infections, cardiac injury, autoimmune syndrome, urea, and drug hypersensitivity) and non-inflammatory (primary or secondary, metabolic, traumatic, or due to reduced lymphatic drainage). The preferred examination modality for diagnosis is echocardiography, which allows pericardial effusion to be classified according to size, localization, and hemodynamic status (1).
Due to the impact of the increased thyroid-stimulating hormone on the pathophysiology of the effusion, pericardial effusion may occur during severe hypothyroidism. However, it is uncommon in cases of central hypothyroidism (2).
Sheehan syndrome is the cause of 6% of all cases of hypopituitarism (3). Postpartum hemorrhage (PPH) causes spasms in smaller vessels, apoplexy, and pituitary necrosis. A lack of anterior pituitary hormone due to the infraction and necrosis of the physiologically enlarged pituitary gland of pregnancy typically causes this condition (4). Sheehan syndrome's extended latency period and silent nature are to blame for the challenging diagnosis of this syndrome. Inadequate therapy for Sheehan syndrome could have fatal results and severe clinical outcomes such as adrenal crisis, circulatory collapse, myxedema coma, and hyponatremia (5).
2. Objectives
About 70% of India's population live in villages. Eighteen million of the projected 25 million deliveries occur annually in rural regions with subpar or nonexistent maternal and perinatal services. PPH is a common delivery complication that typically affects 2 - 4% of vaginal deliveries and 6% of cesarean deliveries, with uterine atony being the cause in roughly 50% of cases (6). As a result, quite a few females may experience this issue.
This study describes the case of a middle-aged woman with panhypopituitarism and the strategy for effective management.
3. Case Presentation
A 48-year-old woman who had experienced diffuse chest pain came to the emergency room (ER). The chest pain, initiated five years back, which was episodic in nature and lasted for a week, and since then, similar recurrent episodes have occurred every six months until present. She also had a history of multiple episodes of shortness of breath, headache, and loss of consciousness. Moreover, she reported involuntary weight loss of approximately 15 kg over five years. Also, 600 mL of straw-colored fluid was aspirated two years ago during an emergency pericardiocentesis. She was empirically given anti-tubercular therapy for nine months, given tubercular pericardial effusion. Despite anti-tubercular therapy, her symptoms persisted.
She was alert, asthenic, with marked mucocutaneous pallor, afebrile, blood pressure of 80/60 mm of Hg, pulse of 124/min, respiratory rate of 26/min, and oxygen saturation at room air of 92%. On auscultation, she had venous jugular engorgement with bilaterally decreased vesicular breath sounds in lung bases and decreased heart sounds.
The results of the investigations pointed to central hypothyroidism with lowered free T3 levels, free T4 levels, and TSH levels. The leading question revealed her eight-year amenorrhea history since her last pregnancy. This pregnancy was complicated by postpartum hemorrhage. Other investigations were done to rule out hypopituitarism, and serum hormone levels (Table 1) indicated panhypopituitarism.
| Serum Hormones | Actual Values | Reference Range |
|---|---|---|
| Cortisol | 1.23 µg/dL | 5 - 23 µg/dL |
| FSH | 1.2 mIU/mL | 36 - 138 mIU/mL |
| LH | 1.6 mIU/mL | 14 - 48 mIU/mL |
| Prolactin | 1.99 ng/mL | 3.1 - 20.5 ng/mL |
| Estradiol | < 10 pg/mL | < 30 pg/mL for post-menopausal women |
| Free T3 | 0.899 pg/mL | 1.5 - 5 pg/mL |
| Free T4 | 0.103 pg/mL | 0.95 - 2.25 ng/mL |
| TSH | 0.7 µIU/mL | 0.2 - 5.1 µIU/mL |
Serum Hormone Levels
Panhypopituitarism was identified as the diagnosis, along with significant central hypothyroidism and hypocortisolism (Table 1).
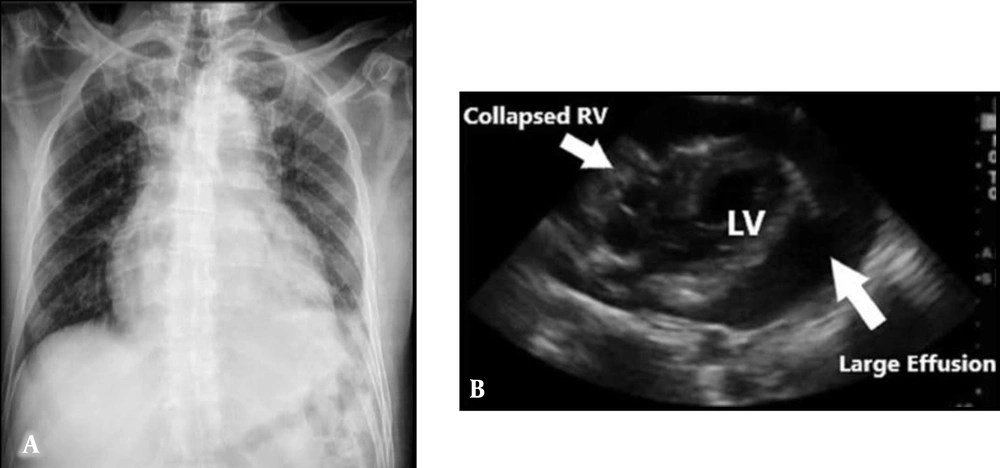
Her chest X-ray showed cardiomegaly with prominent broncho vascular markings in both upper zones, suggestive of pericardial effusion with pulmonary edema, and her electrocardiogram showed low voltage complexes (Figure 1A).
An echocardiogram confirmed a global simple pericardial effusion with evidence of cardiac tamponade and hemodynamic compromise (Figure 1B).
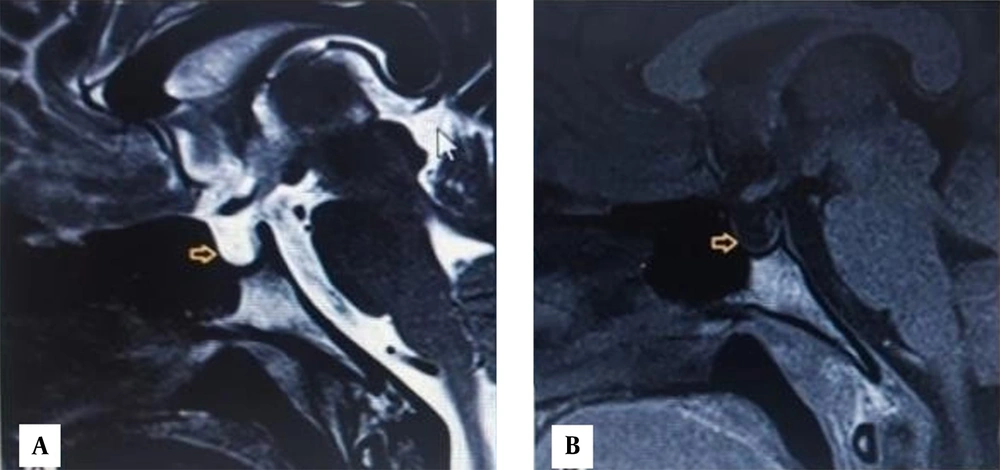
MRI brain with the pituitary protocol was done, which showed empty sella (Figure 2).
Based on the history of postpartum hemorrhage, a diagnosis of Sheehan syndrome was given. MRI of the pituitary showed empty sella, suggestive of complete anterior pituitary failure.
4. Results
At the initial visit, symptomatic treatment (NSAIDs, IV fluids) was done, and MRI was advised with no reduction in symptoms. Hormone replacement therapy with hydrocortisone (5 mg twice a day) and levothyroxine (50 µg) was started with other symptomatic treatment, and clinical improvement was noted within one month. Pericardiocentesis was done to withdraw the pericardial fluid, and the patient was followed-up regularly, showing no recurrence of pericardial effusion.
5. Discussion
This case report shows an unusual presentation of panhypopituitarism with massive pericardial effusion. Panhypopituitarism, when the pituitary gland fails to generate the majority of all hormones, is an uncommon disorder (incidence of 2.07 - 4.2 cases per 100,000 people/year and a prevalence of 37.5 - 45.5 cases per 100,000 people) (7, 8). The most common cause is the presence of pituitary tumoral lesions (macroadenomas, cysts, metastases), with other causes being pituitary surgery or radiotherapy.
The severity of the hormone insufficiency, as well as the quantity and type of the pituitary hormones impacted, all influence the clinical manifestation (8). In addition to endocrine dysfunction symptoms, patients may experience symptoms related to the underlying pathology (5). Life-threatening consequences such as adrenal crisis, coma, and heart failure related to myxedema can result from panhypopituitarism (2, 9, 10).
Sheehan syndrome is diagnosed based on a history of postpartum hemorrhage and the presence of an empty sella on an MRI of the pituitary. PPH is a common delivery complication, with incidence rates of 2 - 4% after vaginal birth and 6% following cesarean sections, with uterine atony being the primary cause in roughly 50% of cases. Consequently, a sizable proportion of females may have this issue (11).
In 3 - 6% of all instances of hypothyroidism, pericardial effusion develops; these cases resolve after returning to the euthyroid state (12). A very uncommon symptom of central hypothyroidism is pericardial effusion. It results from the deposition of glycosaminoglycans, protein extravasation brought on by increased capillary permeability, poor lymphatic drainage, and sodium and water retention (2, 10). Inferred from the finding of a partially empty sella, the case may have been complicated by asymptomatic pituitary apoplexy. The patient's overall condition gradually improved due to pericardiocentesis and hormone replacement therapy. No pericardial effusion recurrence has been shown during the three-year follow-up visit.
5.1. Conclusions
(1) Recurrent pericardial effusion should be evaluated with a comprehensive history and detailed biochemical analysis in an Indian setting in females.
(2) Before starting anti-tubercular therapy, try to rule out other causes of pericardial effusion, like central hypothyroidism.
(3) After a history of PPH, a woman should be followed for at least five years with clinical and biochemical evaluation for early detection of panhypopituitarism.