1. Context
Diabetes mellitus is the most common metabolic disease associated with multiple complications such as cardiovascular diseases, kidney failure, blindness, and amputation of lower extremities (1). It is predicted that by the year 2035, there are about 592 million patients with type 2 diabetes worldwide (2). Moreover, it is estimated that over the next decade, the total number of diabetes-related deaths increases by more than 50% (3). Despite oral medication, insulin, and diet therapy, diabetic complications and immune response impairments are challenges in clinical treatment of these conditions. Although insulin therapy is the main treatment, patients with diabetes who have needle phobia often prefer alternative treatments. Hence, during the past years many efforts were made to develop effective alternative treatments especially an appropriate substitute for insulin delivery (4). Camel milk is supposed to be a suitable alternative as it has an insulin like protein, which does not form coagulum in the acidic environment of stomach (5). It is shown that the incidence risk of diabetes in camel breeders in India, who consume camel milk regularly, is much lower compared to other communities in which camel milk is not consumed (6). Radioimmunoassay analysis detected a high concentration of insulin (52 U/L) in camel milk (7); it also contains large concentrations of immunoglobulin, lactoferrin, lactoperoxidase, and peptidoglycan recognition protein, which have biological and pharmacological properties (8). Recent experimental and clinical studies showed the beneficiary effects of camel milk on diabetes by improving the glycemic control and decreasing insulin resistance (9-11). However, the anti-diabetic action of camel milk is not yet fully elucidated. Moreover, to the best of the authors` knowledge, there is no documented systematic review on the role of camel milk on diabetes. The current systematic review, taking in account all experimental and clinical trial studies, aimed at summarizing published data on the beneficial effects of camel milk to control type 1 and type 2 diabetes mellitus.
2. Evidence Acquisition
2.1. Search Strategy and Study Selection
A literature search was conducted on PubMed and Scopus for entire clinical trials and animal studies published on the effect of camel milk on diabetes markers up to November 2015. The search was conducted by 1 of the authors and there was no restriction regarding publication date. Moreover, reference lists of the included studies and key reviews in the area were scanned for any additional relevant studies. The search terms included (camel milk [Title/Abstract]) OR (camel dairy [Title/Abstract]) AND (diabetes [Title/Abstract]) OR (diabetic [Title/Abstract]) OR (hyperglycemia [Title/Abstract]) OR (fasting blood glucose [Title/Abstract]) OR (insulin resistance [Title/Abstract]) OR (serum insulin [Title/Abstract]) OR (impaired fasting glucose [Title/Abstract]) OR (impaired glucose tolerance [Title/Abstract]) OR (glucose homeostasis [Title/Abstract]). The search terms used for camel milk and diabetes sections were linked using ‘OR’, and the results of the 2 sections were combined by utilizing the ‘AND’.
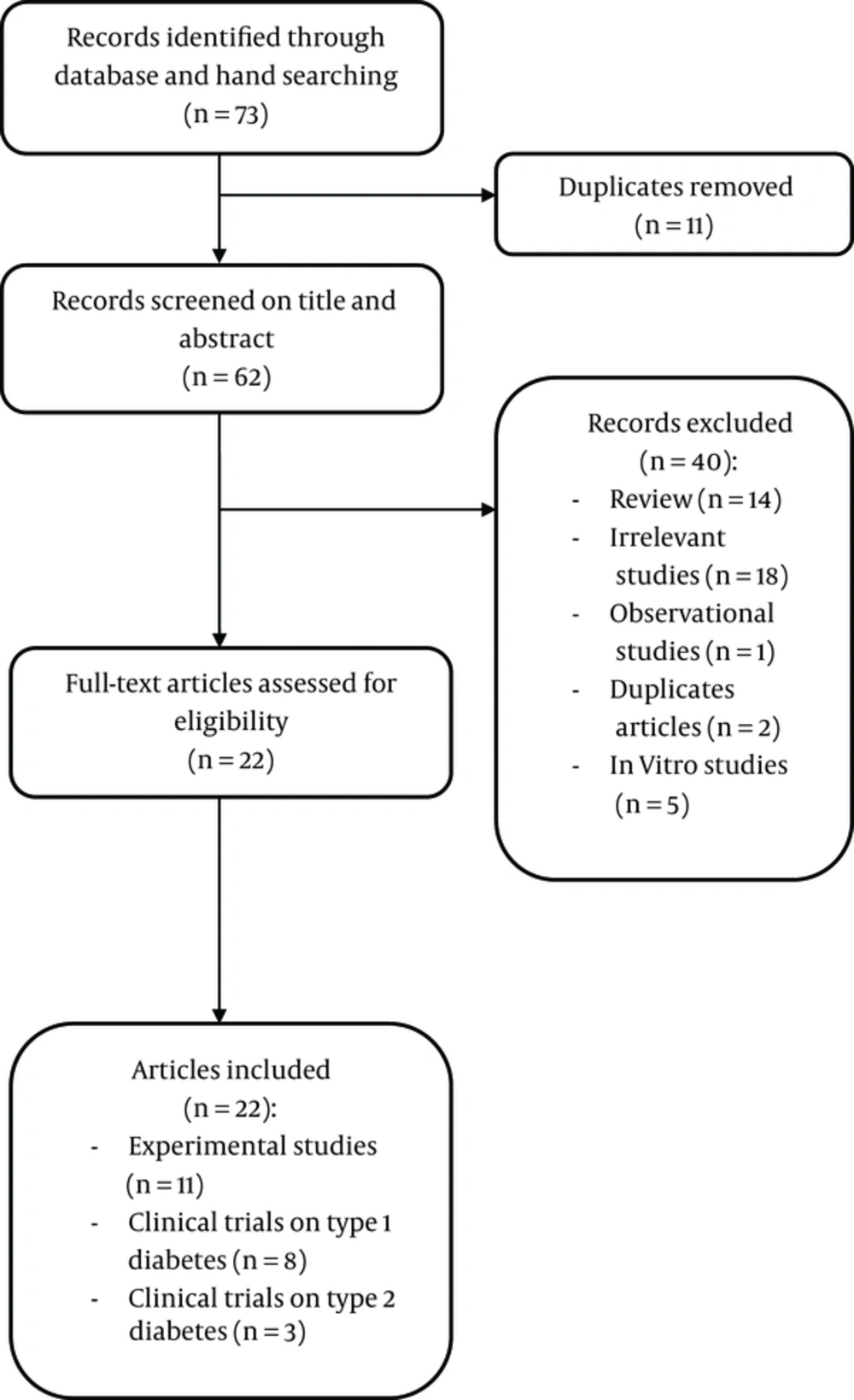
The search results of databases were combined and duplicates were removed. After that, screening of article titles and abstracts was performed independently by 2 investigators, and irrelevant studies were removed. Then, the full texts of potentially eligible studies were reviewed before definitive inclusion. Disagreements between the 2 investigators were resolved by consensus, and the studies were included if they assessed the effect of camel milk on glycemic control or lipid profiles among patients with diabetes, or experimentally induced diabetic animals.
2.2. Eligibility Criteria
Studies had to meet the following criteria to be included in the current review:
- Measurements of the glucose parameters: Fasting blood sugar levels (FBS), general blood glucose levels, postprandial blood glucose levels, serum levels of insulin, insulin resistance [homeostatic model assessment-insulin resistance (HOMA-IR)], and glycated hemoglobin (HbA1c).
- Measurements of the lipid profiles Total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), and triglycerides (TG).
- Types of interventions: Intervention criteria including daily treatment by camel milk in animal or human samples with diabetes, with no dose limits considered.
- Language: English
Obviously irrelevant studies, in vitro studies, studies that did not include any of the primary outcome measures, studies in languages other than English, non-experimental studies (case studies, case series, cross-sectional, case-control, and cohort), study protocols, and literature reviews were excluded from the current systematic review.
2.3. Data Extraction
Relevant data were extracted from studies. Disagreements between the 2 investigators were resolved through discussion until consensus. The data extraction form included the following information: first author’s name and year of publication, country and study design, sample size, range of follow-up, demographic characteristics of participants, dose of camel milk intake, and the evaluated outcomes.
2.4. Quality Assessment
Delphi checklist was used to assess the quality of the included clinical trials and score the studies (12). The quality of reports was assessed. Disagreements between the 2 investigators were resolved through discussion until consensus.
3. Results
3.1. Overview of Studies
The initial search yielded 73 articles that after removing the duplicates, 62 articles were assessed for titles and abstracts. Exclusion of the articles was based on the content and its relevance to the current review, based on the inclusion/exclusion criteria; hence, 40 articles were excluded for being review (n = 14), observational (n = 1), irrelevant to the main topic (n = 18), duplicates (n = 2), and in vitro studies (n = 5). Ultimately, 22 articles were included in the current systematic review, consisting of 11 animal studies and 11 clinical trials, 9 of which focused on type 1 diabetes and the other 3 ones on type 2 diabetes (Figure 1). Characteristics of the participants, interventions, methodological quality, and outcome measures of animal studies and clinical trials are summarized in Tables 1 - 3.
| Study (Year) | Target Species | Intervention Group | Control Group | Duration of Intervention | Outcomes |
|---|---|---|---|---|---|
| Korish (2014) (13) | Streptozotocin-induced diabetic rats (N = 80) | N = 20; 35 mL/rat/day camel milk | 1. Normal with no treatment (n = 20); 2. Normal+ camel milk (n = 20) 3. Diabetic with no treatment (n = 20) | 8 w | ↓Fasting blood glucose, ↓Serum insulin, ↓Lipid profile in camel milk group |
| Khan, AA. (2013) (14) | Streptozotocin-induced diabetic male rats N = 40 | (N = 8) Camel milk 400 mL/day | 1. Normal with no treatment (n = 8); 2. Normal+ camel milk (n = 8) 3. Diabetic with no treatment (n = 8); 4. Diabetic+ insulin treatment | 30 d | ↓Blood glucose, ↓Total cholesterol, ↓Triglyceride in camel milk group |
| Alabdulkarim, (2012) (15) | Female albino rats n = 30 | N = 12; 50-100% camel milk N = 12 50-100% camel milk | N = 6 No treatment | 6 w | No changes in plasma glucose and cholesterol in the camel milk and cow milk groups |
| Al-Numair et al. (2010 - 2011) (16-19)a | Streptozotocin-induced diabetic male albino rats N = 30 | N = 6, camel milk 250 mL/day | N = 18; No treatment | 45 d | ↓Plasma glucose in camel milk group; ↑Insulin levels in camel milk group |
| Al-Numair et al. (2010) (20) | Streptozotocin-induced diabetic male albino rats; N = 40 | N = 8; 250 mL/day camel milk (26 mL/day) | N = 24; No treatment | 45 d | ↓ Blood glucose in camel milk group; ↑Insulin levels in camel milk group |
| Sboui et al. (2010) (21) | Alloxan-induced diabetic dogs; N = 20 | TEST 1: N = 4; 500 mL/day camel milk | N = 4; 500 mL/day cow milk | 5 w | ↓Blood glucose, ↓Cholesterol in Camel milk group; ↑ Blood glucose, ↑Cholesterol in cow milk group |
| TEST 2: N = 4250 mL/day camel milk N = 4100 mL/day camel milk | No treatment | 5 w | ↓Blood glucose, ↓Cholesterol in dogs receiving 250 mL/day camel milk. No changes in blood glucose and cholesterol in dogs receiving 100 mL/day camel milk | ||
| Sboui et al. (2010) (11) | Alloxan-induced diabetic dogs N = 12 | TEST 1:N = 4; 500 mL/day camel milk | N = 4; 500 mL/day cow milk | 5 w | ↓Blood glucose, ↓Cholesterol in camel milk group; ↑Blood glucose, ↑Cholesterol in cow milk group |
| TEST 2: (n = 4)control group receiving 500 mL/day camel milk | No treatment | 5 w | ↓Blood glucose, ↓Cholesterol | ||
| Wang et al. (2009) (22)b | Type 2 diabetic rats N = 32 | 1. Camel milk 2.Rosiglitazone + camel milk | 1. No treatment 2. Rosiglitazone | 14 w | ↓Blood glucose, ↓Plasma insulin, ↓Cholesterol, ↓Triglyceride in camel milk, rosiglitazone, rosiglitazone + camel milk groups compared to diabetic control group with no treatment |
| ↓Plasma insulin, ↓ Triglyceride in Rosiglitazone + camel milk group compared to rosiglitazone group |
aAl-Numair K.S. et al. in 4 studies with the same sample size and design evaluated the effect of camel milk on hyperlipidemia, activating of ATPase, antioxidant factors, collagen abnormalities, and glycoprotein components in streptozotocin-diabetic rats (16-19).
bAs the full text of this article was not accessible, some details were not available.
| Study (year) | Target Population | Intervention Group | Control Group | Duration of Intervention | Outcomes | The Quality of Study (Delphi) |
|---|---|---|---|---|---|---|
| Agrawal et al. (2011) (10) | N = 24; 14 - 16 years | N = 12 Camel milk 500 mL/day | N = 12 Usual care | 2 y | ↓Insulin dose, ↓hemoglobin A1c, ↓Fasting blood sugar in camel milk group | 5/9 |
| Agrawal et al. (2009) (23) | N = 24; Mean age: 19 years | N = 24 Before-after Came milk 500 mL/day | N = 12 Usual care | 6 mo | ↓Insulin dose, ↓Lipid profile, no changes in Hemoglobin A1c, mean plasma glucose and plasma insulin in camel milk group | 2/9 |
| Mohamad et al. (2009) (9) | N = 54; 17 - 20 years | N = 27 Camel milk 500 mL/day | N = 27 Usual care | 16 w | ↓Insulin dose, ↓Fasting blood sugar, ↓HemoglobinA1c,↑Serum insulin in camel milk group | 4/9 |
| Agrawal et al. (2007) (24) | N = 50; 13-14 years | N = 25; camel milk 500 mL/day | N = 25; Usual care | 12 mo | ↓Insulin dose, ↓Blood glucose,↓HemoglobinA1c in camel milk group | 2/9 |
| Agrawal et al. (2005) (25) | N = 24; 13-15 years | N = 12 camel milk 500 mL/day | N = 12 Usual care | 52 w | ↓Insulin dose, ↓Fasting blood sugar, ↓Hemoglobin A1c, no changes in plasma insulin in camel milk group | 4/9 |
| Agrawal et al. (2005) (26) | N = 24; 6 - 25 years | N = 12 camel milk 500 mL/day | N = 12 Usual care | 1 y | ↓Insulin dose, ↓Fasting blood sugar, ↓HemoglobinA1c, no changes in plasma insulin in camel milk group | 4/9 |
| Agrawal et al. (2003) (27) | N = 24; mean age: 20 years | N = 12; camel milk 500 mL/day | N = 12; Usual care | 3 mo | ↓Insulin dose, ↓Fasting blood sugar, ↓HemoglobinA1c, no changes in plasma insulin in camel milk group | 4/9 |
| Agrawal et al. (2003) (28) | N = 24; Mean age: 20 years | N = 12; camel milk 500 mL/day | N = 12; Usual care | 3 mo (crossover design) | ↓Insulin dose, ↓Fasting blood sugar, ↓Hemoglobin A1c, no changes in plasma insulin and lipid profile in camel milk group | 5/9 |
| Study (Year) | Target Population | Intervention Group | Control Group | Duration of Intervention | Outcomes | The Quality of Study (Delphi) |
|---|---|---|---|---|---|---|
| Ejtahed et al. (2015) (29) | N = 20; 20 - 70 years | N = 11; 500 mL/day camel milk | N = 9; 500 mL/day cow milk | 2 mo | No changes in fasting blood sugar and lipid profile,↑ insulin in both groups. ↑HOMA-IR in camel milk group | 4/9 |
| Agrawal et al. (2011) (30) | N = 28;44-54 years | N = 14; 500 mL/day camel milk | N = 14; 500 mL/day Cow milk | 3 mo (crossover) | ↓Fasting blood sugar, ↓HemoglobinA1C, ↑HOMA-IR in camel milk group | 4/9 |
| Wang et al. (2009) (22)a | N = 12 | N = 6 camel milk 500 mL/day | N = 6; Usual care | - | ↓Blood sugar, ↓Plasma insulin, ↓Dose of drug, ↓Cholesterol, ↓Triglyceride in camel milk group | - |
Abbreviation: HOMA-IR, Homeostatic model assessment-insulin resistance.
aAs the full text of this article was not accessible, some details were not available.
3.2. Camel Milk and Diabetes
3.2.1. Animal Studies
Out of 11 experimental studies, 2 were conducted on dogs; in the first study, Sboui et al. evaluated the effect of camel milk on blood glucose and cholesterol in alloxan-induced diabetic dogs (n = 12). They divided dogs into 3 groups, 1 healthy controls and 2 diabetic groups; 1 of the diabetic groups and the controls received 500 mL/day camel milk, while the other diabetic group received 500 mL/day cow milk. After 5 weeks, blood glucose and cholesterol concentration significantly decreased in the camel milk receiving diabetic group, but increased in the cow milk diabetic group, alterations observed even after 3 weeks of intervention. The control group showed no significant difference in the mentioned parameters after the intervention period; results also showed that substituting cow milk with camel milk in the cow milk diabetic group led to significant improvement in blood glucose (from 10.88 ± 0.50 to 5.77 ± 0.44 mM/L, P value < 0.05) and cholesterol status (from 6.17 ± 0.15 to 4.35 ± 0.61 mM/L, P value < 0.05) after 4 weeks (21). In the other study, Sboui et al. compared the anti-diabetic effect of 3 amounts of camel milk: 100, 250, and 500 mL on alloxan- induced diabetic dogs. After 5 weeks, both groups treated with 500 or 250 mL camel milk showed significant decrease in blood glucose (about 48%, P value < 0.05) and cholesterol (about 22%, P value < 0.05), with no significant differences between the 2 groups. No significant difference was observed in such parameters in the dogs treated with 100 mL of camel milk (11); however, there was no control group in this study and the effect of camel milk was not compared with any kind of milks or treatments.
The other 9 studies were conducted on rats, and all had control groups for their intervention; however, there were some variations in the study design, sample size, duration, and dosages of camel milk administration; in 6 of them diabetes was induced by streptozotocin. Most of them demonstrated the effectiveness and superiority of camel milk in glycemic control and insulin sensitivity as well as improvement of lipid profiles in the diabetes induced animals, when compared to the controlled or cow milk groups. However, in the study by Alabdulkarim et al. no significant difference was observed in plasma glucose and triglyceride levels after administering either camel or cow milk; in this study, 30 healthy female albino rats, aged 128 days were randomly divided into 5 groups, with the control group receiving no milk, 2 groups were fed with 50% to 100% camel milk and 2 other groups with 50% to 100% cow milk (15). This study did not demonstrate the hypoglycemic effect of camel milk in the healthy rats. However, it is noteworthy that this study was conducted on healthy rats; therefore, it was not logically appropriate to conclude about the anti-diabetic effects of camel milk. Baseline blood sugar should be considered in the interpretation of results.
Wang et al. evaluated the efficacy of camel milk on long-term glycemic control in diabetic rats; 32 obese rats were randomly divided into 4 groups: the diabetic control group, camel milk group, diabetic rosiglitazone maleate group, and diabetic rosiglitazone maleate + camel milk group. After 14 weeks of treatment, blood glucose, triglycerides, total cholesterol, and plasma insulin significantly decreased in the rosiglitazone maleate, the rosiglitazone maleate + camel milk and the camel milk group compared to the diabetes group. The Rosiglitazone maleate and rosiglitazone maleate + camel milk groups showed significant decrease in blood triglycerides (0.68 ± 0.19 vs. 0.51 ± 0.11 mM/L, P value < 0.05), and plasma insulin (43.52 ± 18.93 vs. 26.49 ± 5.60 mIU/L, P value < 0.05). The rosiglitazone maleate + camel milk group had better treatment of type 2 diabetes animal models than rosiglitazone maleate group (22).
Al-Numair et al. in 5 studies on streptozotocin-induced diabetic rats, evaluated the effect of camel milk on hyperlipidemia, activating of ATPase, antioxidant factors, collagen abnormalities, and glycoprotein components (16-20); 30 male albino rats were randomly divided into 5 groups (6 animals in each group): non-diabetic control, non-diabetic fed with 250 mL/day camel milk, diabetic control, diabetic fed with 250 mL/day camel milk, and diabetic given 600 µg/kg body weight glibenclamide; all groups were treated for a period of 45 days. Diabetic rats treated with camel milk or glibenclamide showed a significant decrease in blood glucose (about 43% and 58%, respectively) and glycoproteins, and an increase in the insulin levels (P value < 0.05); results also showed that treatment with camel milk improved the plasma total cholesterol, triglyceride, free fatty acid, LDL, and HDL-cholesterol (about 42%, 26%, 42%, 25% and 13% respectively, P value < 0.05) in diabetic rats. It seems that all of these 5 studies conducted by Al-Numair et al. were 1 survey with reporting different results in different papers.
Khan et al. examined the effect of camel milk on 40 diabetic rats, divided in a model similar to that of Al-Numair. However, the rats in the 2nd and 4th groups were fed 400 mL/day camel milk and the 5th group was treated with insulin instead of glibenclamide. The intervention period was 30 days and similar outcomes were obtained ie, decreased blood glucose (from 520 to 235 mg/dL, P value < 0.05), triglyceride (about 35%, P value < 0.05), and total cholesterol (about 34%, P value < 0.05) following camel milk treatment (14). Korish et al. categorized 80 rats in 4 groups: the normal and diabetic control with no treatment and the normal and diabetic groups treated with 35 mL/day camel milk for 8 weeks. At the end of the study, diabetic rats treated with camel milk showed significant decrease in fasting glucose (about 57%, P value < 0.001), increased HDL-cholesterol (about 32%, P value < 0.001), decreased HOMA-IR (about 52%, P value < 0.05), and increased fasting insulin (about 34%, P value < 0.05), compared to diabetic controls, while the control rats treated with camel milk showed no significant changes in comparison with normal controls (13).
Overall, camel milk treatment led to improvement of blood glucose, serum insulin, and lipid profile in diabetic animals. This potential positive role on diabetes control could be related to the high content of insulin and insulin like proteins that can increase the activity of insulin receptors (31). Moreover, camel milk is believed to decrease β-cell injuries because of certain specific types of immunoglobulins, protective proteins (lactoferrin and lactoperoxidase), and antioxidant agents; eg, zinc and vitamin c and b3 (24). However, more experimental studies are needed to confirm the superiority and efficacy of camel milk, compared with other milks and alternative treatments for diabetes.
3.2.2. Human Studies
3.2.2.1. Type 1 Diabetes
Agrawal et al. in 5 randomized controlled clinical trials, examined the effect of camel milk along with insulin therapy in patients with type 1diabetes. The sample size in all the studies was 24 subjects. The control group (n = 12) received usual care, while the intervention group received 500 mL/day camel milk in addition to usual care. In the 1st and 2nd studies, the mean age of participants was 20 years and the intervention time was 3 months. However, the 2nd study had crossover design and after a 1-month wash out period, the regimen was interchanged and intervention and control groups were switched over to cow milk and camel milk, respectively, for another 3 months. A significant reduction was observed in FBS (from 115.66 to 100 mg/dL, P value = 0.002), HbA1c (from 9.54% to 9.08%, P value = 0.002), and the mean doses of insulin injection (from 41.66 to 30 U/day, P value = 0.002) in patients receiving camel milk even after 3 months of treatments; however, fasting plasma insulin, lipid profiles, and C-peptide levels showed no significant change in either group (27, 28). The investigators rechecked this hypothesis on 13 to 15 and 6 to 25 year-old subjects in 2 other studies with one year intervention period (25, 26). Moreover, in a study performed on 14 to 16 year-old patients with type 1 diabetes for 2 years (10), which demonstrated the same results in improving FBS (from 118.58 to 93.16 mg/dL), HbA1c (from 7.81% to 5.44%), and the mean doses of insulin (P value < 0.05). In another study, 50 patients newly diagnosed with type 1diabetes, aged 13 to 14 years, were divided into 2 groups, the usual care and the 500 mL/d camel milk + usual care groups. After 12 months, FBS (about 14%), HbA1c (about 8%) and the doses of insulin (about 37%) decreased, and C-peptide levels (about 12%) increased significantly, in patients receiving camel milk (24). Although, in these studies, the effect of camel milk on diabetes parameters was assessed in different age groups with differences in duration of camel milk supplementation, in all of them except for 1, the comparison between camel milk and other kinds of milk was ignored.
The beneficial effect of camel milk in diabetic nephropathy by improvement in micro albuminuria was observed in a study performed on 24 patients with type 1diabetes, mean age 19 years, given 500 mL/day camel milk in addition to usual care for 6 months; although mean plasma glucose, insulin, and C-peptide levels showed no significant changes in these patients after 6 months, their lipid profiles and the mean dose of insulin injection to obtain glycemic control decreased significantly (from 41.6 to 28.3 U/day, P value < 0.01); however, this study had no control group and the effect of camel milk was not compared with any kind of milks or treatments in this study (23).
Mohamad et al. evaluated the effect of camel milk in 54 young patients with type 1diabetes, age range 17 to 20 years, randomly divided into 2 groups: the usual care and the 500 mL/d camel milk + usual care. After 16 weeks of intervention, FBS and HbA1c decreased (56% and 25%, respectively, P value < 0.001) while C-peptide levels increased significantly (88%, P value = 0.007) in the group treated with camel milk (9).
Overall, most of these studies indicate the beneficial effects of camel milk on type 1 diabetes through reduction in FBS, HbA1c, and the mean doses of insulin injection. However, they are not high qualified according to Delphi checklist (the mean score was 3) and more valid studies are needed to prescribe camel milk in type 1 diabetes.
3.2.2.2. Type 2 Diabetes
Studies on the hypoglycemic potential of camel milk on type 2 diabetes are limited. Wang et al. randomly divided 12 patients with type 2 diabetes into 2 groups, with 6 patients receiving routine diabetes management and 6 other patients consumed 500 mL/day of raw camel milk. The dose of potential rosiglitazone maleate administration was adjusted in both groups. In the group receiving camel milk, there was a significant reduction in the mean blood sugar (123.0 to 94.2 mg/dL, P value < 0.001), plasma insulin (19.76 to 6.21 mIU/L, P value < 0.001), dose of drug (4.67 to 1.67 U/d, P < 0.001), blood triglycerides (1.83 to 1.42 mM/L, P value < 0.001), and blood total cholesterol (7.7 to 6.1 mM/L, P value < 0.001), compared with baseline values (22). Agrawal et al. in a crossover design study, prescribed 500 mL/day cow milk to 14 healthy males and 500 mL/day camel milk to 14 males with type 2 diabetes for 3 months; after 1 month washout period, the regimen was interchanged for 3 months. FBS, HbA1c, and insulin levels showed an improving trend both in males with diabetes and the healthy ones after camel milk consumption (30). Ejtahed et al. in a randomized, single-blinded controlled clinical trial evaluated the effect of camel milk on blood sugar and lipid profiles of 20 patients with type 2 diabetes aged 20to 70 years. Intervention group (n = 11) received 500 mL/day camel milk and control group (n = 9) consumed 500 mL/day cow milk for 2 months. Fasting blood sugar, lipid profiles and blood pressure showed no significant differences between the 2 groups at the end of the study, but insulin concentration significantly increased (about 23%, P value < 0.05) in the camel milk group during the study (29). The variation in camel milk composition and clinical characteristics of participants, short duration of intervention, and low sample size could be the reasons of inconsistent results in this study.
There are some possible mechanisms, which justify the anti-diabetic effects of camel milk. Camel milk contains considerable level of insulin encapsulated in nanoparticles to transport this hormone intact into the bloodstream. Camel milk insulin resists coagulum formation in the stomach, and is absorbed in the small intestine (32). Furthermore, camel milk has small insulin-like molecules that act like insulin in interacting with their receptors (33). Camel milk has special proteins, lyzozymes, lactoferrin, and lactoperoxidase, which are resistant to digestion by pepsin in the stomach; these proteins do not coagulate easily at low pH, and have a good buffering capacity (34).
As high production of oxidative stress factors in diabetes can lead to deleterious effects including damage to polyunsaturated fatty acids in membrane lipids, proteins, DNA, and eventually cell death (35), 1 of the positive roles of camel milk in diabetes is its high level of antioxidants postulated to have anti-inflammatory effects and immune-modulatory functions on the β-Cells of the pancreas (13, 36). Whey protein of camel milk is easily available and is supposed to reduce the effects of oxygen radicals by increasing glutathione (37, 38); in addition to restoring normal ß-Cell mass and suppressing inflammatory cytokines which lead to ß-Cell apoptosis in type 1 diabetes (39).
Certain other proteins in camel milk such as lactoferrin have an anti-inflammatory effect, which can inhibit the production of pro-inflammatory cytokines; eg, tumor necrosis factor (TNF)-α, interleukin (IL)-1 and IL-6 in mononuclear cells (40). On the other hand, camel milk decreases TNF-α and down regulates the expression of iNOS, the major source of NO generation during inflammation (41).
Increased oxidative damage also has a strong positive association with abnormal lipid profiles, commonly observed in patients with diabetes (42), the damage which could be improved by the anti-inflammatory effect of camel milk consumption. High levels of antioxidant agents such as zinc, selenium, and other trace elements (43) in camel milk are also reported to prevent lipid peroxidation, via enhancing the anti-oxidant system (44), or by glutathione peroxidase activation (45). Overall, there are limited studies with inconsistent results regarding the effects of camel milk on type 2 diabetes and further research is required to confirm the long-term efficacy of camel milk on biomarkers of type 2 diabetes.
4. Conclusions
In the current systematic review, the potentially positive effects of camel milk on diabetes mellitus were explored. Data available on experimental research and most of the human studies indicated that camel milk administration can have positive effects on glycemic control, by reducing fasting blood sugar, decreasing insulin resistance, and improving lipid profiles among patients with diabetes. In most studies, the recommended dose of camel milk was 500 mL/day which led to improvement of diabetes markers even after 3 months in patients with diabetes. Moreover, the superiority of camel milk, compared to cow milk was demonstrated in some human studies. Although the high amount of digestion resistant insulin and high level of antioxidants as anti-inflammatory factors are the possible explanation for anti-diabetic effect of camel milk in this review, however, more valid and comprehensive studies are needed to support these findings.