1. Background
Insulin resistance is considered to be a risk factor for the development of metabolic syndrome (MetS). A recent review has elucidated the genetic background for the cause-effect relationship between these pathological conditions (1). In addition, the serum C-reactive protein (CRP), widely used as an indicator of systemic inflammation is associated with insulin resistance and the risk of MetS development (2).
Serum gamma-glutamyl transferase (GGT) has been used as an indicator of alcohol overload and several hepatic inflammatory diseases, and is considered as a useful biomarker of the risk of MetS or cardiovascular disease (3, 4). In addition, serum alanine aminotransferase (ALT) is also a predictive biomarker for MetS (5).
Hyperuricemia is also a risk factor for MetS, which has been explained based on the insulin resistance, visceral fat accumulation or xanthine oxidoreductase metabolism (6-8).
2. Objectives
The author conducted a one-year follow-up study to investigate the predictive ability of two insulin-related biomarkers, namely, the homeostasis model assessment for insulin resistance (HOMA-IR), and quantitative insulin sensitivity check index (QUICKI) (9-12), in combination with some other risk factors, as independent variables, for identifying the risk of MetS development.
3. Patients and Methods
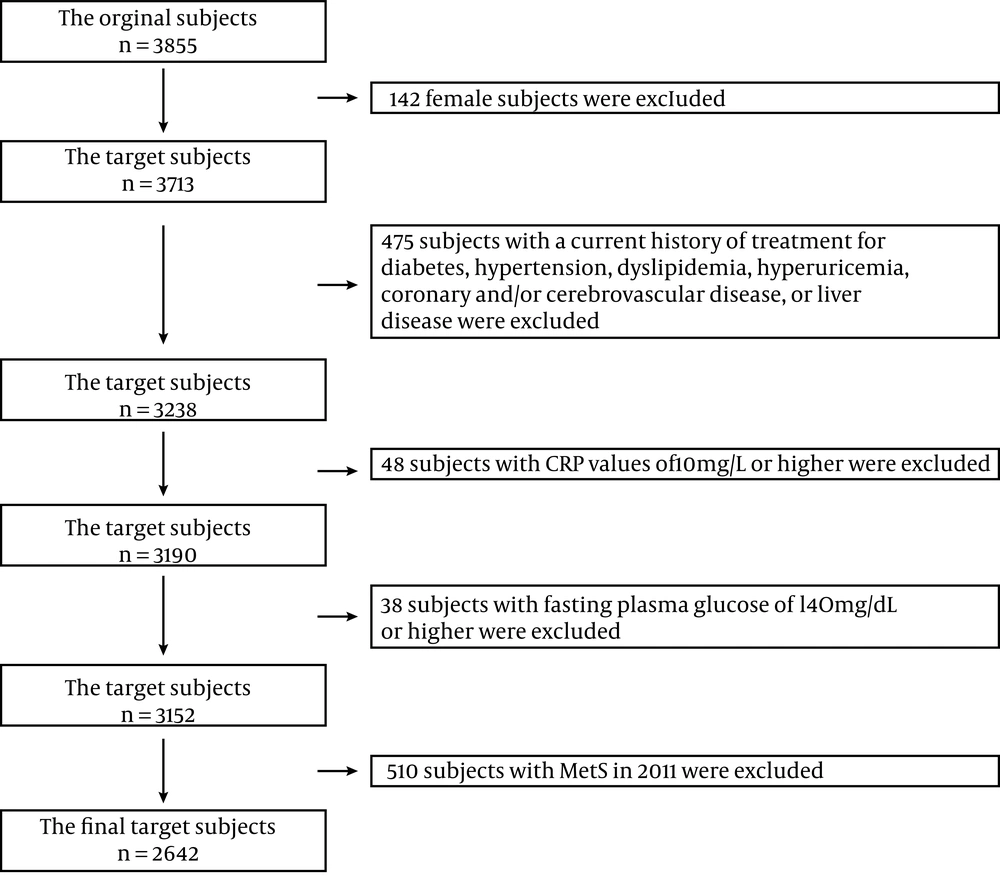
A total of 3713 male workers (age range, 35 – 63 years) of a Japanese company were recruited for this study. All the subjects had responded to a questionnaire containing questions on the current medical and treatment history and some lifestyle factors. They underwent two consecutive annual health examinations, which included measurements of the waist circumference (WC) and systolic/diastolic blood pressure (measured in the sitting position after the subjects had rested for 3 minutes), and collection of fasting blood samples. Subjects with a current history of treatment for diabetes, hypertension, dyslipidemia, hyperuricemia, coronary and/or cerebrovascular disease, and liver disease were excluded (n = 475). Subjects with CRP values of 10 mg/L or higher were excluded by considering acute occult inflammation or chronic infectious disorder (n = 48), and subjects with MetS or high plasma glucose levels (>= 140 mg/dL) at the baseline study were also excluded to maintain the validity of the results on the insulin-related biomarkers (n = 38). Namely, as a simple surrogate index for insulin sensitivity/resistance, I adopted the upper limitation value of plasma fasting glucose for HOMA-IR and QUICKI at 140 mg/dL in this study ( 13 ). As the number of subjects with Mets in 2011 was 510, the final target subject became 2642 (Figure 1).
Informed consent was obtained from the study participants, and the study protocol was approved by the ethics committee of the university.
Data on lifestyle-related variables was gathered from the self-administered questionnaire. Smoking habit was categorized as current smoking (0) or no smoking, including ex-smoking (1). Drinking habit was categorized as everyday drinking (0) or occasional drinking, including no drinking (1). Physical activity was categorized as everyday exercise, including walking for ≥ 1 hour (1) or no daily exercise habit (0). Especially, I used the following questionnaire to evaluate habitual exercise; “Do you take exercise every day, including walking for at least one hour?”
The author used the criteria of the National Cholesterol Education Program Adult Treatment Panel III (ATP III), in which MetS is defined based on the presence of three or more of the following criteria: central obesity (waist circumference ≥ 85 cm) (14); hypertriglyceridemia (serum triglyceride ≥ 150 mg/dL); reduced serum level of high-density lipoprotein (HDL) cholesterol (serum HDL < 40 mg/dL); high-blood pressure (systolic BP ≥ 130 mmHg and/or a diastolic BP ≥ 85 mm Hg); high fasting plasma glucose (FPG) (≥ 100 mg/dL) (15).
Serum ALT, GGT, and uric acid were measured with an automatic analyzer (7700 series, Hitachi, Tokyo). Serum high-sensitivity CRP measurement was based on a Latex turbidity assay (Mitsubishi Kagaku Iatron, Tokyo, Japan) using the Hitachi 7700 auto-analyzer. The detection limit of this assay is 0.1 mg/L. The intraassay CVs for repeated measurements ranged from 0.84% to 2.54%. Insulin was measured using CLEIA (Fujirebio Inc, Tokyo, Japan) and Lumipulse Presto II. The detection limit of this assay is 0.3 mIU/L. The intraassay CV for repeated measurements was 3.06%. Serum HDL cholesterol, triglyceride, and glucose levels were determined enzymatically with a Hitachi 7700 auto-analyzer.
As the insulin-related biomarkers, HOMA-IR and QUICKI were calculated as follows:
HOMA-R = (FPG × insulin)/405; QUICKI = 1/ (common logarithms (FPG × insulin))
The units of glucose and insulin for the HOMA-R calculation were mg/dL and mIU/L, respectively.
Mathematically, the association between these two indicators becomes a monotone decreasing function. The distribution of HOMA-IR is logarithmic-normal; whereas, that of QUICKI is normal. Although FPG was used for the calculation, the serum insulin and HOMA-IR were closely related (16).
All the statistical analyses were conducted using SPSS 16.0 for Windows (SPSS Japan, Tokyo). Spearman's rho was calculated for the univariate analysis. Then, a multiple logistic regression analysis was performed for predicting the risk of MetS development as the dependent variable. Three lifestyle factors were originally classified in a binary manner. Other independent variables were also converted to binary format, namely, age (≥ 45 and <45 years old), uric acid (≥ 7 and <7 mg/dL), ALT (≥ 45 and < 45 IU/L), GGT (≥ 50 and < 50 IU/L), CRP (≥ 1 and <1 mg/L), HOMA-IR (≥ 2.5 and < 2.5), and QUICKI (≤ 0.33 and >0.33), which were assigned the values of 1 and 0. A cut-off value of the highest tertile of age became 45 years, and cut-off value of CRP was adopted as "mildly elevated" (17, 18). P-values of less than 0.05 according to a two-tailed test were considered to denote statistical significance.
4. Results
Characteristics of the study population at baseline were presented in Table 1, and the correlation matrix was also presented in Table 2. The analysis revealed that HOMA-IR and QUICKI were mathematically equal. In addition, strong associations were observed between the serum insulin and HOMA-IR or QUICKI, with Spearman’s rho of 0.98 and -0.98, respectively.
| Variables | Results |
|---|---|
| Age, y | 43.2 ± 6.5 b |
| Waist circumference, cm | 81.7 ± 8.6 b |
| Systolic blood pressure, mmHg | 123.7 ± 12.0 b |
| Diastolic blood pressure, mmHg | 77.4 ± 9.4 b |
| Triglyceride, mg/dL | 110.8 ± 72.5 b |
| HDL cholesterol, mg/dL | 61.2 ± 15.3 b |
| Plasma glucose, mg/dL | 91.5 ± 9.1 b |
| Uric acid, mg/dL | 6.0 ± 1.2 b |
| HOMA-IRa | 1.3 (1.8) |
| CRP, mg/La | 0.4 (2.7) |
| ALT, IU/La | 24.5 (1.7) |
| GGT, IU/La | 30.9 (1.9) |
| Nosmoking or ex-smoking | 52.7% (1392/2642) |
| Exercise for ≥ 1 hour everyday | 37.4% (989/2642) |
| Not everyday drinking | 66.0% (1743/2642) |
aGeometric mean (geometric standard deviation)
Abbreviations: HDL; high-density lipoprotein, ALT; alanine aminotransferase, GGT; gamma-glutamyl transferase, CRP; C-reactive protein, HOMA-IR; the homeostasis model assessment for insulin
bMeans ± SD
| Spearman’s rhoa | FPG | Insulin | HOMA-IR |
|---|---|---|---|
| FPG | |||
| Insulin | 0.16 | ||
| HOMA-IR | 0.32 | 0.98 | |
| QUICKI | -0.32 | -0.98 | -1.0 |
aThere were significant associations among four variables with significance level of 0.01.
Abbreviations: FPG; fasting plasma glucose, HOMA-R; the homeostasis model assessment for insulin resistance, QUICKIl; the quantitative insulin sensitivity check index
The incidence of metabolic syndrome was 8.8% after one-year follow-up. Unadjusted and age-adjusted odds ratios (95% confidence intervals) of HOMA-IR (≥ 2.5) for MetS were 2.9 (2.1 - 4.0) and 3.0 (2.2 - 4.1), respectively (P < 0.001). In addition, unadjusted and age-adjusted odds ratios (95% confidence intervals) of QUICKI (≤ 0.33) for MetS were 3.2 (2.3 - 4.5) and 3.3 (2.3 - 4.6), respectively (P < 0.001). A multiple logistic regression analysis showed that absence of regular physical activity, age (≥ 45 years old), serum uric acid (≥ 7 mg/dL), serum alanine aminotransferase (≥ 45 IU/L), serum C-reactive protein (≥ 0.1 mg/L), and HOMA-IR (≥ 2.5) Were identified as significantly contributing to the risk of MetS, with odds ratios (95% confidence intervals) of 0.68 (0.50 – 0.92), 2.0 (1.5 – 2.6), 2.2 (1.6 – 3.0), 1.5 (1.02 – 2.2), 1.4 (1.01 – 2.0), and 2.3 (1.6 – 3.3) respectively (Table 3).
Abbreviations: ALT; alanine aminotransferase, GGT; gamma-glutamyl transferase, CRP; C-reactive protein, HOMA-IR; the homeostasis model assessment for insulin resistance
When QUICKI was used instead of HOMA-IR, the absence of regular physical activity, age (≥ 45 years old), serum uric acid (≥ 7 mg/dL), serum gamma-glutamyl transferase (≥ 50 IU/L), and QUICKI (≤ 0.33) were identified as significantly contributing to the risk of MetS, with odds ratios (95% confidence intervals) of 0.68 (0.51 – 0.93), 2.0 (1.5 – 2.6), 2.2 (1.6 – 3.0), 1.4 (1.01 – 2.0), and 2.5 (1.7 – 3.6) respectively (Table 4).
ALT; alanine aminotransferase, GGT; gamma-glutamyl transferase, CRP; C-reactive protein, QUICKI; the quantitative insulin sensitivity check index
5. Discussion
The predictive ability of insulin resistance or insulin sensitivity for MetS in Japanese male subjects was checked by a one-year follow-up study. HOMA-IR and QUICKI were equally contributed to the incidence of MetS after adjustments for other independent variables.
WHO defined insulin resistance as a HOMA-IR of ≥ 1.8 (19). In this study, the author adopted another criterion for insulin resistance in patients with HOMA-IR ≥ 2.5, which is popular in Japan. The author also adopted QUICKI ≤ 0.33 as a criterion of insulin sensitivity. The results of the study showed a strong association between the serum insulin and HOMA-IR or QUICKI in this study. This means that insulin-related biomarkers can be used interchangeably; although, there is a limitation that both HOMA-IR and QUICKI can only be applied reliably for subjects with fasting glucose levels under 140 mg/dL. The author previously reported that there was a high correlation of insulin with HOMA and QICKI, but low correlation with FPG (16). In this study, the same finding was observed and contribution of FPG to HOMA-IR and QUICKI was relatively small.
Among the lifestyle factors, only habitual exercise contributed significantly to lowering the risk of MetS in this study, which was consistent with a previous report (20). Smoking is known to be associated with insulin resistance and the risk of MetS development (21-23); however, our present results did not corroborate this notion. This discrepancy should be explored by further follow-up of the target population. By logistic regression analysis, physical activity was identified as a low-risk factor, as it was associated with a reduction in the incidence of MetS by 32%.
Serum ALT has been reported to be associated with adiposity and insulin resistance (24), and serum GGT to be a predictor of cardiovascular mortality (25). In my study, serum ALT or GGT was selected as a significant contributor to the risk of MetS when HOMA-IR or QUICKI was used as an independent variable, respectively. However, as the P value was near 0.05, the contribution was not statistically strong for either case in this study. The findings were similar for serum CRP, which has been found to contribute significantly to the risk of MetS. In contrast, serum uric acid was found to be significantly associated with the risk of MetS, its significance being equivalent to that of age. This finding was consistent with the results of a long-term follow-up study suggesting that serum uric acid was associated with the risk of MetS and cardiovascular mortality (26).
Categorization of continuous variable leads to the loss of power. But understanding the level of risk improves by categorization. As simplest categorization is the binary classification, the author adopted binary conversion of independent variable for logistic regression analysis.
This study was a one-year follow-up study, and the causality could only be partially determined. But the two insulin-related biomarkers examined exhibited equivalent ability as predictive markers for MetS in this study.