1. Introduction
Most thyroid tumors are primary and of epithelial origin, while tumors of mesenchymal origin, common in other organs, rarely occur in this gland (1-3). Vascular thyroid lesions include benign neoformation such as hemangiomas, and malignant tumors, like angiosarcoma and angiosarcomatoid carcinoma. Angiosarcoma is a rare soft tissue tumor, accounting for about 1-2 % of all sarcomas, mainly occurring in the skin and head and neck superficial soft tissues (1, 4, 5). Thyroid angiosarcoma is a rare malignant tumor of endothelial differentiation, mainly found in European mountainous regions of the Alps (Switzerland, Austria and Northern Italy), where it represents up to 16% of thyroid malignancies (1, 5-8). Its high prevalence in those regions is thought to be due to iodine deficiency associated goiter, because most thyroid angiosarcomas occur in a multinodular gland (6, 7). Although its etiology remains unknown, it was suggested that endothelial proliferation after recurrent hemorrhage in nodules within a long-standing multinodular goiter, can induce neoplastic transformation (1, 2). It is more common in females (ratio 9:3) and mainly occurs between the fifth and eighth decades (the median age of 65 years) (1, 6, 9). Generally, these tumors present as a painless infiltrating mass with tendency to increase its size (1), which can vary from 2.5 to 11cm, being usually unifocal (6, 10). Cytological characteristics of this type of cancer have not been clearly defined yet and are rarely described in the literature (5). Histological examination often reveals extensive areas of necrosis, hemorrhage with the presence of anastomosing channels lined by endothelial cells. Endothelial differentiation is evidenced by the expression of vascular markers such as CD31 (the most sensitive and specific marker), CD34 and factor VIII related antigen. In many cases, there may be coexpression of cytokeratins. Immunonegativity for thyroglobulin supports its diagnosis (6-8). Some authors believe that most thyroid angiosarcomas are in fact anaplastic thyroid carcinomas with angiomatoid features; however, this distinction is considered academic, since their prognosis and treatment are similar (1, 8, 11). Treatment of these tumors is conditioned by local aggressive behavior and high recurrence rate, consisting of radical surgery wherever feasible. Radiation therapy seems to be effective in some patients and can be complemented with chemotherapy using Adriamycin (1, 7). Recurrence and development of metastasis are common, even after complete resection (2) and the prognosis is poor, due to local aggressive behavior. Presence of distant metastasis and extracapsular tumor extension are frequently associated with a poor prognosis (1). Metastasis is commonly found in local lymph nodes, lung and bone marrow (1, 12). Mean 5-year survival rate is near 33% and most patients die in less than six months, regardless of treatment (1, 6).
2. Case Presentation
We present a 61-year-old-women with no relevant medical history, born in northern Portugal, where she has always lived. When a neck mass was noticed, neck ultrasound was performed showing two solid thyroid nodules, one in the right lobe with about 3 cm and another in the left lobe with about 9 mm. There were no associated compression symptoms. Fine needle aspiration (FNA) cytology was held reporting “suspicious for malignancy". The patient underwent total thyroidectomy and histological examination showed a 35 mm heterogeneous and hemorrhagic vascular neoplasm with dilated vessels, areas of necrosis, with swollen endothelial cells and atypical mitoses between thyroid follicles and cells. Immunohistochemistry staining showed negative results for cytokeratins MNF, CAM5.2, CD34, thyroglobulin and positive finding for CD31. These findings confirmed the diagnosis of angiosarcoma. A 4 mm papillary microcarcinoma was also identified in the left lobe, without any poor prognosis criteria. Neck computerized tomography (CT) scan performed two months after the operation showed a 35 mm nodular lesion in the right surgical bed, with irregular margins, conditioning tracheal deviation. The patient was referred to our institution. FNA of the nodule was held showing local recurrence of the previously diagnosed malignancy. 18F-FDG PET-CT identified a single neck hypermetabolic lesion compatible with tumor recurrence (Figure 1).
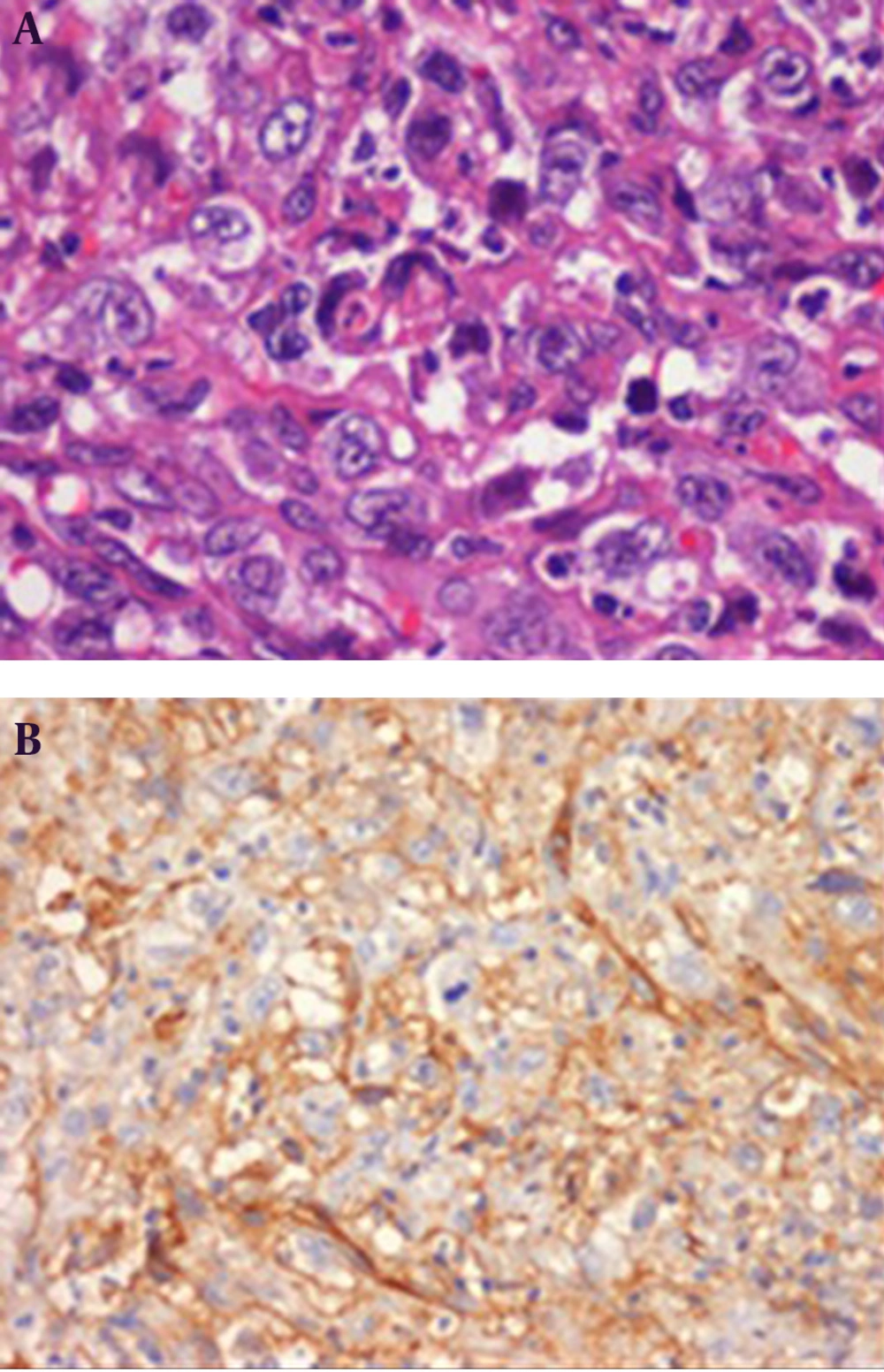
Tumor resection was performed and invasion to larynx, trachea and esophagus was noticed intraoperatively. Histological examination revealed a 2.5 cm angiosarcoma, with positive surgical margins and immunohistochemistry staining showed the same features described above, including strong positivity result for CD31 with cytoplasmic and membranous pattern (Figure 2).
It was decided to treat the patient with local radiotherapy (60Gy), completed four years ago. The patient was kept under close surveillance at our institution, and about six years after the initial diagnosis, there was no clinical, analytical or imaging (neck CT, magnetic resonance imaging) evidence of tumor recurrence.
3. Conclusions
We described a rare case of thyroid angiosarcoma associated with a papillary microcarcinoma on the contralateral lobe in a patient living outside the Alpine region. A recent literature review by Kaur et al. (13) identified 48 cases of thyroid angiosarcoma worldwide. Since then, as far as we know, three more cases were published (14-16), and including one we described, there are a total of 52 patients with thyroid angiosarcoma in the literature. Generally, there was a favorable outcome despite initial local recurrence with invasion to adjacent organs. We are unaware of what might exactly influenced the patient’s prognosis, but we believe that local radiotherapy may have an important role in the treatment of these types of lesions. Data available is insufficient to suggest the most suitable approach to this type of cases, but surgical treatment of head and neck angiosarcoma followed by radiotherapy improved patient’s survival (13). However, there are some reports of patients treated with radiotherapy who did not respond to that modality of treatment (5, 6, 17). We could not find any similar case of such a long disease free period, after radiation treatment. In areas not associated with endemic multinodular goiter, cases with higher than average survival have been reported (1), comparable to our patient’s case. Good prognosis has been associated with absence of extra glandular extension (9), which was found in this case, but not changing the final outcome. The low incidence of these tumors in non-Alpine regions makes them difficult to diagnose and treat. Being so, we believe that multidisciplinary collaboration is essential in addressing this and other rare thyroid neoplasms.